Abstract
South Africa currently has the highest number of cases of HIV in the world. HIV antiretrovirals (ARVs) are publicly available across the country to address this crisis. However, a consequence of widely available ARVs has been the diversion of these drugs for recreational usage in a drug cocktail commonly known as “nyaope” or “whoonga,” which poses a significant public health concern. To better understand nyaope, we conducted a systematic review investigating the risks and consequences associated with its usage. Following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, searches were conducted in eight different databases and screened thereafter. Articles were eligible for inclusion if they included analysis of least one nyaope user and considered either demographics, risk factors, or consequences of usage. Data extracted included study characteristics and limitations, as well as demographic factors, risk factors for usage in the general population, and consequences. Quality assessments were performed using the Joanna Briggs Institute’s tools. Searches produced a total of 228 articles and, after screening, a total of 19 articles were eligible for inclusion. There was a pooled total of 807 nyaope users, all in South Africa. Major risk factors for usage were being male, unemployed, not completing secondary education, pressure from peer groups, having HIV, prior use of cannabis, and to a lesser extent, usage of other substances such as alcohol and tobacco. While young adults tend to be at high-risk, evidence indicates that adolescents are also at-risk. Consequences of usage include high rates of infection, cortical atrophy, depression, and addiction. Addiction was shown to lead to individuals stealing from friends and family to pay for the drugs. HIV-positive nyaope users were more likely to partake in risk behaviours and tended to have high viral loads. Nyaope’s rise has been linked to many health and social issues. Considering that this may also disrupt HIV control efforts in South Africa, there is an urgent need to address the rise of nyaope.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
HIV in South Africa
South Africa currently has the highest prevalence of human immunodeficiency virus (HIV) globally [1, 2]. In recent years, the country has taken significant steps to help more HIV-positive South African citizens gain access to treatment for this disease. Antiretroviral therapy (ART) has improved the lives of people living with HIV as this therapy has decreased mortality and morbidity, and increased lifespan. Adherence to daily oral medication is an important determinant for suppression and prevention of drug-resistant viral strains. However, maintaining adherence to daily drug intake remains a challenging task [3]. In 2010, the South Africa’s Department of Health implemented an effective program to provide increased access of antiretrovirals (ARVs), free of cost to HIV-infected South African citizens [4]. However, an unexpected result of the increased availability of treatment for HIV has been the emergence of recreational ARV use across the country.
Recreational ARV Use
Understanding why ARVs are being consumed for purposes other than the treatment of HIV requires an explanation of the physiological effects of the drugs. Not all ARVs have neuropsychiatric effects. Efavirenz is one of the primary drugs used in ART, found to have psychoactive properties comparable to the hallucinatory drug lysergic acid diethylamide (LSD), including mania and psychosis [5, 6]. Efavirenz and another commonly used ARV known as ritonavir also seem to have specific euphoric effects when mixed with drugs such as methamphetamine, ecstasy, heroin, tobacco, and cannabis [7,8,9]. Mixtures of recreational drugs containing ARVs have also been found to contain rat poison, household cleaning supplies, milk powder, pool cleaner, and bicarbonate of soda [10,11,12]. Though users of this drug cocktail typically smoke the mixture, some individuals have been reported to inject the mixture [13]. This drug cocktail has most frequently been referred to as nyaope.
Nyaope
Nyaope is a highly potent drug compared to other well-known drugs; while it frequently contains substances such as ARVs, cannabis, heroin, rat poison and detergent, it is worthwhile to denote the chemical makeup of nyaope has been shown to also vary and may change over time [14]. Though it is most commonly referred to as nyaope, in prior studies and media reports, this drug cocktail has also been referred to by a number of other names; these include whoonga [10, 15,16,17], kataza [11, 18], plazana [8, 19, 20], ungah [8, 19, 20], and BoMkon [8, 21, 22].
According to media reports, the mixture of nyaope had begun being used as early as the year 2000 [16]. However, there is a lack of concrete evidence to back up the claim by these reports that nyaope use had begun in 2000. Instead, the earliest available reports concretely documenting recreational nyaope use were published from 2006 and onwards [10, 17,18,19,20,21]. Based on the recognition that the usage of nyaope was becoming widespread across the country, in 2014 the South African government criminalized the possession and distribution of nyaope, with the selling of nyaope being potentially punishable with a prison sentence of up to 25 years [23].
Objective
Despite concerns regarding the increased usage of nyaope over time [10, 24], the risk factors for nyaope use in the general population, and its consequences for users, are currently not well understood. Therefore, this paper will provide an overview of this relatively new phenomenon. Our objective is to provide a systematic review of the literature regarding the risk factors and consequences of using nyaope.
Methods
Database Searches
Our systematic review workflow followed the ‘Preferred Items for Systematic Review and Meta-Analyses’ (PRISMA) guidelines [25]. On April 3rd 2022, searches were conducted in eight databases: PubMed, Scopus, CINAHL, Global Health, Ovid Medline, PsycINFO, ScienceDirect, and SocIndex. Search terms in respective databases included the numerous ways in which nyaope has previously been referred to, which were the following: “Whoonga” OR “Nyaope” OR “Plazana” OR “Kwape” OR “Ungah” OR “Kataza” OR “BoMkon”. No restrictions were placed based on the date of publication.
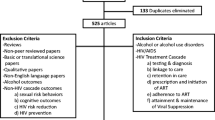
Screening Process
We removed all duplicate articles for the review process. Next, articles were screened for eligibility based on title, abstract, and keyword. After that, all remaining articles were assessed by full-text analysis to determine if they were eligible for inclusion in the review. Articles were included if they fulfilled the following criteria for inclusion: (1) available in English, (2) included at least one individual using nyaope, (3) analyzed demographics/risk factors for nyaope use or effects/consequences of its usage. There were no restrictions placed based on the country of study and no restrictions based on study design for original research studies, but articles were excluded if they were not original research (such as reviews, editorials, and commentaries).
Data Extraction
Data on study characteristics was first extracted from the included studies. Extracted data on study characteristics included the following: location of study, study design, source of data, term(s) used for drug, total nyaope users compared to total participants, and limitations of the study. Next, data was extracted based on the characteristics of nyaope users. The following data was extracted for this purpose: total nyaope users, gender, age, risk factors for nyaope usage, and consequences of usage. We also included an additional column for other findings (if relevant) for each study. Examples of additional findings included length of nyaope use, pregnancy, age when individuals began using nyaope, and substance co-use.
Quality Assessment
All studies that were included underwent a quality assessment using the Joanna Briggs Institute’s (JBI) critical appraisal tools [26]. The JBI tools were chosen as they offer a valid quality appraisal tool across multiple types of methodologies; this was important for our review as included studies had the following study designs: qualitative, case–control, cross-sectional, case report, and cohort. Following the approach conducted in other reviews [27, 28], the JBI tools were adapted to provide a numeric score, with qualitative studies and case–control studies each on ten-item scales, cross-sectional studies and case reports each on different eight-item scales, and cohort studies on an eleven-item scale. Similar to an approach previously taken [28], numeric scores were depicted graphically, with the scores being used to assess differences in methodological quality.
Results
Eligible Studies
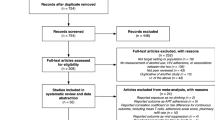
Combined searches from all eight databases produced a total of 228 results. 137 articles remained after the removal of duplicates. After screening by title and abstract, 43 articles remained. A total of 19 articles [6, 13, 14, 29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44] fulfilled the criteria for inclusion and were therefore eligible for analysis (Fig. 1) [25].
PRISMA 2020 flow diagram [25]
Study Characteristics
All 19 studies were conducted in South Africa, with 13 taking place in Gauteng Province [13, 29,30,31,32, 35, 36, 39,40,41,42,43,44], two in Western Cape [6, 43], two in KwaZulu-Natal [33, 38], one in Mpumalanga [29], one in Northwest [29], and one in Eastern Cape [14]. One study did not specify the province within South Africa [37], whereas another study was conducted across the country [34]. An additional was study conducted in three provinces: Gauteng, Mpumalanga, and Northwest [29]. There were a range of different methodologies among included studies: six studies had a qualitative design [14, 29,30,31,32,33], five were cross-sectional studies [6, 13, 34,35,36], four were case reports [37,38,39,40], two were retrospective cohort studies [41, 42], one was a prospective cohort study [43], and one study had a case–control design [44]. The most frequently noted limitations included low participant totals in studies, study eligibility being restricted to adult participants, and a heavy reliance on self-reporting. “Nyaope” was a term used for the drug in all 19 studies, and nine studies also utilized the term “whoonga” [6, 30, 33, 35, 37, 38, 40, 41, 43]. Other terms also used were “wunga” [6, 40, 41], “pinch” [35], “unga” [35], “sugars” [37], and “kataza” [37]. The complete characteristics of the 19 included studies are listed in Table 1.
By study, the characteristics of nyaope users are listed in Table 2. There was a pooled total of 807 nyaope users. Total participants by analysis ranged from 1 to 221. Of the seven studies where both men and women were described as eligible for inclusion [13, 29, 31, 36, 41,42,43], six studies had a considerably higher number of male nyaope users than women [6, 13, 29, 31, 36, 41]. In one study where both men and women were eligible for inclusion, 97.1% of nyaope users were male [41].
Quality Assessments
Quality assessments for all included studies are depicted in Fig. 2, and critical appraisal checklists are shown in Supplementary Tables 1–5. Studies generally ranged from mid to low quality overall. Qualitative studies had a mean score of 7.83 (SD = 1.33) on a ten-item scale, cross-sectional studies had a mean score of 5.00 (SD = 1.00) on an eight-item scale, case reports had a mean score of 5.50 (SD = 1.73) on an eight-item scale, cohort studies had a mean score of 7.00 (SD = 1.00) on an eleven-item scale, and the single case–control study had a score of 8.00 on a ten-item scale. The most frequent methodological flaws shown across studies were the limited strategies to address confounding factors, infrequent determination of the extent of nyaope use, and an inconsistent consideration of unanticipated adverse effects of usage.

(Adapted from Adalbert et al. [28])
Quality assessment scores by study
Risk Factors
In the majority of studies, nyaope users were most frequently between 18 and 29 years of age [13, 29,30,31, 33,34,35,36, 39,40,41, 44], though a number of studies also demonstrated that there are nyaope users in their 30s and 40s [13, 29,30,31, 34, 35, 43, 44]. While those under 18 years were not eligible for inclusion in many of the included studies, some studies showed that nyaope usage is also occurring in adolescents as young as 13 years of age [6, 14, 37].
Across the included studies, one of the most frequent risk factors for nyaope usage was unemployment [14, 29,30,31, 33,34,35,36, 41]. In one study, 100% of nyaope users were unemployed [41]. Other studies also had high rates of unemployment for nyaope users, at 96% [35], 86% [29], and 74% [31].
Prior substance use and co-substance use were also frequently noted as risk factors for nyaope usage [6, 29, 33, 35,36,37,38,39, 44]. The most commonly used substance associated with nyaope use was cannabis [29, 33, 35,36,37], and other substances commonly used were tobacco and alcohol [6, 29, 35, 36, 38, 39, 44]. One study found that 52% of nyaope users previously used cannabis, 13% used cigarettes, and 14% used other drugs [29]. Another study demonstrated that 92.9% of nyaope users were concurrently using alcohol and nicotine regularly and that 92.9% were concurrently using cannabis [44]. The same study found that 100% of participants were using opioids [44].
In particular, limited education and a lack of secondary education completion were also noted in several studies as common risk factors for nyaope use [13, 31, 33, 35, 41]. Other risk factors discussed were pressure to use from peers [13, 31, 33, 36, 37], being HIV-positive [30, 34, 40, 41, 43], limited familial support [32, 36], and having a Black racial background [33, 34].
Consequences
The most commonly noted consequence of nyaope usage across studies was the intense addiction that the drug cocktail causes. Many users were receiving ongoing treatment to address addiction to nyaope [13, 29, 32, 36, 37, 42]. One study noted that nyaope use was significantly associated with non-completion of substance abuse treatment [42].
Symptoms of withdrawal, including pain [39] and an inability to sleep [29], were also described. Due to the addictive nature of nyaope, study participants described using all of their income to obtain more of the substance [14, 29, 31, 37], drop out of school [14, 31, 37], and steal from others [14, 31, 37]. These forms of theft were also reported to have additional consequences, including stigma, social rejection, and loss of family trust [14, 29, 31, 37]. One study also described that transactional sex was used to finance nyaope addiction [30].
Nyaope users had several medical complications with a wide array of clinical manifestations. Studies demonstrated nyaope users were shown to have diarrhea, facial swelling, vomiting, stomach cramps, erectile dysfunction, vein damage, right heart failure, and cortical atrophy [14, 35, 40, 41, 44]. Nyaope users were shown to be at risk for hepatitis B, hepatitis C, tuberculosis, and infective endocarditis [31, 40, 41]. Those using nyaope also showed a number of psychological symptoms including loss of behavioral control/antisocial behavior [13, 14, 29, 31, 44], negative self-perceptions [29, 36], depression [31, 43, 44], decreased motivation [14, 31], mood swings [14, 31], and hallucinations [14]. Among those with HIV, infection rates were markedly elevated [41]. It is also worth denoting that HIV-positive nyaope users were shown to be participating in transactional sex to finance nyaope use [30], were injecting the drug cocktail [30, 40], and not adhering to ARV treatment [41].
Notably, two studies included nyaope users who used the drug cocktail while pregnant [38, 39]. Of these pregnant nyaope users, one infant died, with the cause of death linked to the mother’s nyaope usage [38]. Other infants born of nyaope-using mothers had serious clinical symptoms such as septic shock, respiratory distress, seizure, multi-organ dysfunction, and retinopathy of prematurity [38, 39].
Discussion
Nyaope Addiction
The overall findings of this review contribute to the existing literature regarding nyaope. While it has previously been demonstrated that the emergence of this drug cocktail is a rising social issue, the risk factors for nyaope usage have not previously been understood. Furthermore, the biopsychosocial consequences of usage have not previously been described in great detail. Our findings therefore add to the existing literature in numerous ways. Our review demonstrated that being male, a teenager/young adult, unemployed, HIV-positive, and having a prior history of substance use are all major risk factors for nyaope usage. The majority of the studies included in our review were conducted in Gauteng Province. Consequences of nyaope usage have been shown to be widespread for users. These consequences include erectile dysfunction, cortical atrophy, infection, depression, mood swings, and hallucinations. Additionally, nyaope usage among pregnant mothers has been shown to be particularly dangerous. Our findings also highlight that numerous individual and societal issues arise due to the increased use of nyaope. One of the primary concerns is the highly addictive aspects of this substance, which makes it very difficult for the individual to stop using the drugs.
A study by Möller et al. provides insight into the possible neurological basis for the addictive aspects of ARVs and nyaope [9]. This study was conducted on rats and demonstrated the addictive nature of efavirenz, with numerous similarities to the psychoactive properties of methamphetamines and tetrahydrocannabinol [9]. Additionally, the seriousness of withdrawal after one ceases nyaope usage provides further insight into these drugs' addictiveness. The withdrawal effects of nyaope, which can occur for as long as about a week, include the appearance of flu-like symptoms, nausea, severe cramps, cold chills, frequent sweating, and constant diarrhea [13, 45]. When an addicted individual attempts to stop abusing these drugs, this can lead to criminality, dropping out of school, and lying to family members to facilitate continued drug use. Assisting individuals in getting through these powerful withdrawal symptoms is important for successful rehabilitation. Rehabilitation programs in South Africa can help individuals addicted to these drugs deal with withdrawal symptoms by creating more detoxification services that are unique to these particular substances [23]. It is critical to denote that while there are severe withdrawal symptoms for nyaope users, these symptoms have not been shown to occur among HIV-positive individuals who discontinue usage of their prescribed ARVs, or who miss doses of the ARVs [46]. There is hence a clear need to better understand the biological basis of withdrawal for nyaope in order to better guide the development of treatment for the withdrawal symptoms.
Rehabilitation Programs
While addressing withdrawal symptoms is of high priority in rehabilitation programs, this alone is not adequate in fully supporting nyaope users. Several health complications can arise due to the frequent use of nyaope. Addressing these psychological and physical symptoms would be of high value in rehabilitation programs. This technique could effectively occur by including social workers, counselors, and group therapy during rehabilitation [23, 47]. Mahlangu and Geyer highlight how nyaope users expressed a desire for psychotherapy before and after their treatments [32]. Accordingly, the inclusion of such services could be of value in ensuring that individuals can work towards dealing with the psychological issues involved in this addiction. Notably, a number of nyaope users were concurrently utilizing other substances, such as cannabis, alcohol, tobacco, and methamphetamines. Rehabilitation programs therefore should also utilize approaches that are equipped to deal with the polydrug use. This will require multidisciplinary approaches that should emphasize harm reduction approaches when necessary.
To ensure that nyaope users do not eventually relapse, rehabilitation services should make efforts to ensure that former users can reintegrate into society. This also requires an understanding of what factors may have caused the individual to become addicted in the first place. Strain theories predict that impoverished individuals may resort to substance misuse as a form of “retreatism” [48]. Considering that most nyaope users are unemployed and living in poverty [23], this seems to describe the current situation in South Africa appropriately. Helping individuals find employment can hence be a valuable means of ensuring complete rehabilitation. This would involve assisting nyaope users to develop employable skills and providing them with various forms of temporary employment [45]. As unemployment is denoted as one of the most common risk factors for commencing nyaope usage, there is a need to establish efforts to increase employment levels across the nation of South Africa. This will be particularly important for unemployed, young, Black South African men, who are at the highest risk of nyaope usage.
There is a clear need for community level support to be provided by rehabilitation programs funded primarily by the public sector. With nyaope costing as low as 25 rands for a single joint, it is highly accessible in many impoverished communities [29]. However, many of the worst affected communities do not have access to affordable rehabilitation services due to limited investment for these programs in the public sector, and due to the unaffordability of many of the programs in the private sector [29]. Therefore, supportive rehabilitation programs need to be available at minimal cost for users and must be widely available in impoverished communities.
Nyaope Prevention
Our review indicates that addressing issues of peer pressure and general ignorance of the consequences of nyaope use will be crucial for prevention. One way that this can occur is by having educators share media reports that provide truthful information about the most devastating effects of mixtures with ARVs. There is some evidence indicating that such efforts may be successful. One study demonstrated that the reason why nyaope was not popular at an educational institution was related to the prevalence of negative stigma associated with usage based on a belief that the drug composition included several dangerous substances such as painkillers, benzene, rat pellets, and ARVs [49, 50]. Accordingly, sharing media reports that highlight the worst aspects of this mixture may deter more youth in the future. It is important to denote that removal of stigma towards nyaope users in an empathizing manner will also be integral in ensuring that more users are able to feel safe and comfortable in seeking treatment. Understanding nyaope stigma can hence have a valuable role in both ensuring prevention of high-risk groups, and in increasing rates of rehabilitation for users.
A lack of public knowledge about the dangers of nyaope demonstrates that resources should be invested in informing adolescents, young adults, and the wider community about the risks of consuming this drug mixture. This can occur by creating government-funded workshops that educate individuals about the dangers of nyaope, recreational ARV use, and the dangers of addiction in general. This should also involve public broadcasts and education campaigns warning of the dangers of nyaope use. Creating educational warnings to entire communities and at-risk groups can result in lasting change that deters individuals from using nyaope [51].
Undoubtedly, addressing high levels of nyaope usage will also involve managing other forms of substance misuse among adolescents and young adults as prior substance use is a notable risk factor for nyaope usage. Younger individuals with a high level of usage of substances such as cannabis, tobacco, and alcohol tend to deal with neglect and come from challenging home environments or reside in single-parent households [18]. Reaching out to these at-risk individuals to lower levels of other substance use can potentially lead to less nyaope usage over time.
Nyaope prevention among HIV-positive individuals will be particularly important for a number of reasons. The diversion of ARV treatment can have negative consequences for the person who is no longer on treatment as they will likely have an increased viral load. This therefore increases their risk of progression to AIDS. As demonstrated in a prior study, there is also a clear need to further understand if the diversion of ARVs for nyaope is contributing to drug-resistance of treatment [52]. Considering that HIV-positive nyaope users have been shown to partake in certain behaviours which increase the risk of transmitting HIV to others, such as transactional sex and injecting with shared needles [16], there is a clear need to increase support services to HIV-positive individuals who are at risk of nyaope use. Protective and harm-reduction services, in the form of condom promotion and syringe exchange, will also offer utility in supporting this vulnerable population. Critically, there is a need to monitor the risk of violence towards HIV-positive patients and HIV healthcare providers, as both of these groups have been the victims of such violence in the past by those seeking to obtain ARVs for recreational usage [29, 53, 54]. The issues of theft and redirection of ARVs due to nyaope indicate that this is a concern for wider South African society.
Limitations
It is important to consider and recognize the limitations of this systematic review. While several different study designs and methodologies were included, a high proportion of studies either did not include quantitative data or had a small sample size. As demonstrated by the quality appraisals, many studies were hence unable to consider confounding variables, and many adverse consequences of nyaope usage were not able to be accounted for. This indicates that a large proportion of the complex consequences of nyaope are likely to remain only partially understood. More research is thus needed on the biopsychosocial consequences of nyaope use. Furthermore, while many studies indicated that nyaope usage might be a serious issue among adolescent populations, those under 18 were not eligible for inclusion in many studies reviewed. Therefore, there is a need for larger quantitative studies that include adolescent populations. Lastly, numerous studies could not determine the temporality of factors under study. For example, it is not well established if nyaope users tend to deal with depression due to nyaope usage or if individuals dealing with depression tend to be more likely to use nyaope. Regardless of these limitations, our findings provide a useful starting point for understanding how to support nyaope users during their addiction and how to focus on at-risk populations to prevent them from starting nyaope usage.
Conclusion
The diversion of ARVs for recreational use in the drug cocktail known as “nyaope” poses important implications for its users and their broader community. Our findings highlight that important risk factors for the use of nyaope include unemployment, non-completion of secondary school, being HIV-positive, and prior substance use. Furthermore, those of male gender and younger age are at increased risk of nyaope use; other social factors including peer pressure and stressful home environments can also lend themselves to substance use. Important medical consequences associated with the consumption of nyaope include infection risk, psychological distress, and strong addiction with severe withdrawal symptoms following cessation. Notably, the implications of nyaope use extend beyond the individual medical and psychological consequences to the wider community. Importantly, nyaope addiction can cause financial hardships and damage to family relationships, leading to a tendency for criminality and social stigmatization. In consideration of the severity of issues associated with nyaope, public health campaigns should address these documented risk factors to prevent nyaope use and reduce the burden of concomitant biopsychosocial consequences.
Data Availability
The authors have provided all relevant data in our submission.
References
Central Intelligence Agency (CIA). Country comparison: HIV/AIDS—people living with HIV/AIDS. CIA World Factbook. 2016. https://www.cia.gov/library/publications/the-world-factbook/rankorder/2156rank.html. Accessed 8 Dec 2018.
UNAIDS. Countries—South Africa. UNAIDS; 2018. http://www.unaids.org/en/regionscountries/countries/southafrica. Accessed 8 Dec 2018.
Thoueille P, Choong E, Cavassini M, Buclin T, Decosterd LA. Long-acting antiretrovirals: a new era for the management and prevention of HIV infection. J Antimicrob Chemother. 2021;77(2):290–302.
Michel J, Matlakala C, English R, Lessells R, Newell ML. Collective patient behaviours derailing ART roll-out in KwaZulu-Natal: perspectives of health care providers. AIDS Res Ther. 2013;10(1):20.
Gatch MB, Kozlenkov A, Huang RQ, Yang W, Nguyen JD, González-Maeso J, Rice KC, France CP, Dillon GH, Forster MJ, Schetz JA. The HIV antiretroviral drug efavirenz has LSD-like properties. Neuropsychopharmacology. 2013;38(12):2373–84. https://doi.org/10.1038/npp.2013.135.
DeAtley T, Mathews C, Stein DJ, Grelotti D, Brown LK, Givenco D, Atujuna M, Beardslee W, Kuo C. Risk and protective factors for whoonga use among adolescents in South Africa. Addict Behav Rep. 2020;11(2020): 100277. https://doi.org/10.1016/j.abrep.2020.100277.
Davis GP, Surratt HL, Levin FR, Blanco C. Antiretroviral medication: an emerging category of prescription drug misuse. Am J Addict. 2014;23(6):519–25. https://doi.org/10.1111/j.1521-0391.2013.12107.x.
Dalwadi DA, Ozuna L, Harvey BH, Viljoen M, Schetz JA. Adverse neuropsychiatric events and recreational use of efavirenz and other HIV-1 antiretroviral drugs. Pharmacol Rev. 2018;70(3):684–711.
Möller M, Fourie J, Harvey BH. Efavirenz exposure, alone and in combination with known drugs of abuse, engenders addictive-like bio-behavioural changes in rats. Sci Rep. 2018;8(1):1–13.
Grelotti DJ, Closson EF, Smit JA, Mabude Z, Matthews LT, Safren SA, Bangsberg DR, Mimiaga MJ. Whoonga: potential recreational use of HIV antiretroviral medication in South Africa. AIDS Behav. 2014;18(3):511–8.
Manu E, Maluleke XT, Douglas M. Knowledge of high school learners regarding substance use within high school premises in the Buffalo Flats of East London, Eastern Cape Province, South Africa. J Child Adolesc Subst Abuse. 2017;26(1):1–10.
Marks M, Howell S. Cops, drugs and interloping academics: an ethnographic exploration of the possibility of policing drugs differently in South Africa. Police Pract Res. 2016;14(4):341–52. https://doi.org/10.1080/15614263.2016.1175176.
Fernandes L, Mokwena KE. The role of locus of control in nyaope addiction treatment. S Afr Fam Pract. 2016;58(4):153–7.
Bala S, Kang’ethe S. The dangers associated with female adolescents consuming nyaope drug in Buttersworth, South Africa. J Hum Rights Soc Work. 2021;2021(6):307–17. https://doi.org/10.1007/s41134-021-00173-1.
Fihlani P. ‘Whoonga’ threat to South African HIV patients. Durban: BBC News; 2011. https://www.bbc.com/news/world-africa-12389399. Accessed 28 May 2022.
Rough K, Dietrich J, Essien T, Grelotti DJ, Bansberg DR, Gray G, Katz IT. Whoonga and the abuse and diversion of antiretrovirals in Soweto, South Africa. AIDS Behav. 2014;18(7):1378–80.
Chinuoya M, Rikhotso R, Ngunyulu RN, Peu MD, Mataboge MLS, Mulaudzi FM, Jiyane PM. ‘Some mix it with other things to smoke’: perceived use and misuse of ARV by street thugs in Tshwane District, South Africa. Afr J Phys Health Edu Recreat Dance. 2014;1:113–26.
Nzama MV, Ajani OA. Substance abuse among high school learners in South Africa: a case study of promoting factors. Afr J Dev Stud. 2021;2021(si1):219–42.
Mthembi PM, Mwenesongole EM, Cole MD. Chemical profiling of the street cocktail drug ‘nyaope’in South Africa using GC–MS I: stability studies of components of ‘nyaope’in organic solvents. Forensic Sci Int. 2018;292:115–24.
Mthembu K. Grandma desperate for help. Mpumalanga News; 2013. https://mpumalanganews.co.za/25437/grandma-desperate-help/.
Nkosi R. Nyaope rules Umjindi. Lowvelder; 2014. https://lowvelder.co.za/545624/nyaope-rules-umjindi/.
Prinsloo J, Ovens M. An exploration of lifestyle theory as pertaining to the use of illegal drugs by young persons at risk in informal settlements in South Africa. Acta Criminol. 2015;2015(sed-3):42–53.
Mokwena KE. The novel psychoactive substance ‘Nyaope’ brings unique challenges to mental health services in South Africa. Int J Emerg Ment Health Hum Resilience. 2015;17(1):251–2.
Larkan F, Van Wyk B, Saris J. Of remedies and poisons: recreational use of antiretroviral drugs in the social imagination of South African carers. Afr Sociol Rev. 2010;14(2):62–73.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372: n71. https://doi.org/10.1136/bmj.n71.
Joanna Briggs Institute. Critical appraisal tools. 2020. https://jbi.global/critical-appraisal-tools. Accessed 14 Apr 2021.
Bowring AL, Veronese V, Doyle JS, Stoove M, Hellard M. HIV and sexual risk among men who have sex with men and women in Asia: a systematic review and meta-analysis. AIDS Behav. 2016;20(10):2243–65. https://doi.org/10.1007/s10461-015-1281-x.
Adalbert JR, Varshney K, Tobin R, et al. Clinical outcomes in patients co-infected with COVID-19 and Staphylococcus aureus: a scoping review. BMC Infect Dis. 2021;21:985. https://doi.org/10.1186/s12879-021-06616-4.
Mokwena KE. “Consider our plight”: a cry for help from nyaope users. Health Sa Gesondheid. 2015;21:137–42. https://doi.org/10.1016/j.hsag.2015.09.001.
Lefoka MH, Netangaheni TR. A plea of those who are affected most by HIV: the utterances by women who inject nyaope residing in the City of Tshwane Municipality, Gauteng. Afr J Primary Health Care Fam Med. 2021;13(1):1–9.
Fernandes L, Mokwena KE. Nyaope addiction: the despair of a lost generation. Afr J Drug Alcohol Stud. 2020;19(1):37–51.
Mahlangu S, Geyer S. The aftercare needs of nyaope users: implications for aftercare and reintegration services. Soc Work. 2018;54(3):327–45.
Tyree GA, Mosery N, Closson EF, Mabude Z, du Toit C, Bangsberg DR, Safren SA, Mayer KH, Smit JA, Mimiaga MJ, Grelotti DJ. Trajectories of initiation for the heroin-based drug whoonga—qualitative evidence from South Africa. Int J Drug Policy. 2020;2020(82): 102799. https://doi.org/10.1016/j.drugpo.2020.102799.
Harker N, Lucas WC, Laubscher R, Dada S, Myers B, Parry CD. Is South Africa being spared the global opioid crisis? A review of trends in drug treatment demand for heroin, nyaope and codeine-related medicines in South Africa (2012–2017). Int J Drug Policy. 2020;83: 102839.
Moroatshehla SM, Mokwena K, Mutambirwa S. Impact of nyaope use on erectile function of the users: an exploratory study in three townships of Tshwane District, South Africa. J Drug Alcohol Res. 2020;9(6):1–8.
Mokwena K, Shandukani F, Fernandes L. A profile of substance abuse clients admitted to an in-patient treatment centre in Tshwane, South Africa. J Drug Alcohol Res. 2021;10(6):1–7.
Groenewald C, Essack Z. “I started that day and continued for 2 years”: a case report on adolescent ‘whoonga’ addiction. J Subst Use. 2019;24(6):578–80.
Mashiloane CP, Jeena PH, Thula SA, Singh SA, Masekela R. Maternal use of a combination of recreational and antiretroviral drugs (nyaope/whoonga): case reports of their effects on the respiratory system in infants. Afr J Thorac Crit Care Med. 2021;27(3):120.
Thomas R, Velaphi S. Abuse of antiretroviral drugs combined with addictive drugs by pregnant women is associated with adverse effects in infants and risk of resistance. S Afr J Child Health. 2014;8(2):78–9.
Meel R, Peters F, Essop MR. Tricuspid valve endocarditis associated with intravenous nyoape use: a report of 3 cases: forum-clinical alert. S Afr Med J. 2014;104(12):853–5.
Meel R, Essop MR. Striking increase in the incidence of infective endocarditis associated with recreational drug abuse in urban South Africa. S Afr Med J. 2018;108(7):585.
Dreyer J, Pooe JM, Dzikiti L, Kruger C. Factors associated with successful completion of a substance rehabilitation programme at a psychiatric training hospital. S Afr J Psychiatry. 2020;24(1):1–1.
Magidson JF, Iyer HS, Regenauer KS, Grelotti DJ, Dietrich JJ, Courtney I, Tshabalala G, Orrell C, Gray GE, Bangsberg DR, Katz IT. Recreational ART use among individuals living with HIV/AIDS in South Africa: examining longitudinal ART initiation and viral suppression. Drug Alcohol Depend. 2019;198:192–8.
Ndlovu NA, Morgan N, Malapile S, Subramaney U, Daniels W, Naidoo J, van den Heuvel MP, Calvey T. Fronto-temporal cortical atrophy in ‘nyaope’ combination heroin and cannabis use disorder. Drug Alcohol Depend. 2021;221: 108630.
Ettang D. ‘Desperados, druggies and delinquents’: devising a community-based security regime to combat drug related crime. Afr Dev. 2017;42(3):157–76.
Centers for Disease Control and Prevention. Guidelines for the use of antiretroviral agents in adults and adolescents living with HIV. 2022. https://clinicalinfo.hiv.gov/en/guidelines/hiv-clinical-guidelines-adult-and-adolescent-arv/discontinuation-or-interruption. Accessed 29 May 2022.
Shembe ZT. The effects of whoonga on the learning of affected youth in Kwa-Dabeka Township. Thesis in Master of Education (Socio-education). University of South Africa; 2013.
Mosher CJ, Akins S. Drugs and drug policy: the control of consciousness alteration. Thousand Oaks: Sage; 2007.
Gerardy J. Cheap heroin is killing our children. Saturday Star. 2007 Independent News & Media Public Limited Company; 2007.
Muswede T, Roelofse CJ. Drug use and postgraduate students’ career prospects: implications for career counselling intervention strategies. TD. 2018;14(1):1–8.
Khosa P, Dube N, Nkomo TS. Investigating the implementation of the ke-moja substance abuse prevention programme in South Africa’s Gauteng Province. Open J Soc Sci. 2017;5(8):70–82.
Grelotti DJ, Closson EF, Mimiaga MJ. Pretreatment HIV antiretroviral exposure as a result of the recreational use of antiretroviral medication. Lancet Infect Dis. 2013;13:10–2. https://doi.org/10.1016/S1473-3099(12)70294-3.
Tsuyuki K, Surratt HL, Levi-Minzi MA, O’Grady CL, Kurtz SP. The demand for antiretroviral drugs in the illicit marketplace: implications for HIV disease management among vulnerable populations. AIDS Behav. 2015;19:857–68. https://doi.org/10.1007/sl0461-014-0856-2.
Kuo C, Giovenco D, DeAtley T, Hoare J, Underhill K, Atujuna M, Mathews C, Stein DJ, Brown LK, Operario D. Recreational use of HIV antiretroviral medication and implications for HIV pre-exposure prophylaxis and treatment. AIDS Behav. 2020;24(9):2650–5.
Acknowledgements
No other individuals have made any contributions to the manuscript.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions No financial support was provided.
Author information
Authors and Affiliations
Contributions
KV created the project design, wrote most of the manuscript, completed the reviewing process, and made edits. SDB served as a second reviewer for the review process, helped with project design, and provided edits to the manuscript. SKD helped with project design, made contributions to the manuscript, offered insights and recommendations based on expertise, and made edits to the manuscript. PS & DS assisted with the review process, assisted with writing of the manuscript, and provided edits to the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Ethical Approval
Ethics approval was not required for this systematic review.
Consent to Participate
There were no human or non-human participants in this review, and consent for participation was therefore not required.
Consent for Publication
The authors consent to publishing all submitted data and images.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Varshney, K., Browning, S.D., Debnath, S.K. et al. A Systematic Review of Risk Factors and Consequences of Nyaope Usage: The Illicit Street Drug Containing HIV Antiretrovirals. AIDS Behav 27, 558–577 (2023). https://doi.org/10.1007/s10461-022-03791-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-022-03791-6