Abstract
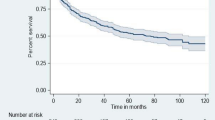
We explored the predictors and predictive models of loss to follow-up (LTFU) during the first year of anti-retroviral therapy (ART). LTFU was defined as the failure to visit the clinic for antiretroviral drugs for ≥ 90 days after the last missed scheduled visit. Based on the electronic medical records of 5953 patients who were HIV positive and began ART between 2016 and 2019 in China, the LTFU rate was 7.24 (95% confidence interval 6.49–7.97) per 100 person-years during the first year of ART. ART baseline factors were associated with LTFU, but were non-optimal predictors. A model including ART process-related factors such as follow-up behaviors and physical health status had an area under the receiver operating characteristic curve of 73.4% for predicting LTFU. Therefore, the medical records of follow-up visits can be used to identify patients with a high risk of LTFU and allow interventions to be implemented proactively.
Similar content being viewed by others

Data Availability
Not applicable.
Code availability
Not applicable.
References
Collaborators GH. Global, regional, and national incidence, prevalence, and mortality of HIV, 1980–2017, and forecasts to 2030, for 195 countries and territories: a systematic analysis for the Global Burden of Diseases, Injuries, and Risk Factors Study 2017. Lancet HIV. 2019;6(12):e831–59.
Balogun M, Meloni ST, Igwilo UU, et al. Status of HIV-infected patients classified as lost to follow up from a large antiretroviral program in southwest Nigeria. PLoS One. 2019;14(7):e0219903.
Geng EH, Bangsberg DR, Musinguzi N, et al. Understanding reasons for and outcomes of patients lost to follow-up in antiretroviral therapy programs in Africa through a sampling-based approach. J Acquir Immune Defic Syndr. 2010;53(3):405–11.
Holmes CB, Sikazwe I, Sikombe K, et al. Estimated mortality on HIV treatment among active patients and patients lost to follow-up in 4 provinces of Zambia: findings from a multistage sampling-based survey. PLoS Med. 2018;15(1):e1002489.
Cohen MS, Chen YQ, McCauley M, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365(6):493–505.
UNAIDS. Accelerating action to end the AIDS epidemic by 2030. 2015. Available at: https://www.unaids.org/sites/default/files/media_asset/201506_JC2743_Understanding_FastTrack_en.pdf. Accessed 2 2020.
Nsanzimana S, Forrest JI. Many pathways to ending AIDS by 2030. Lancet HIV. 2018;5(8):e407–8.
de Almeida MC, de Jesus Pedroso N, do Socorro Lina van Keulen M, et al. Loss to follow-up in a cohort of HIV-infected patients in a regional referral outpatient clinic in Brazil. AIDS Behav. 2014;18(12):2387–96.
Opio D, Semitala FC, Kakeeto A, et al. Loss to follow-up and associated factors among adult people living with HIV at public health facilities in Wakiso district, Uganda: a retrospective cohort study. BMC Health Serv Res. 2019;19(1):628.
Januraga PP, Reekie J, Mulyani T, et al. The cascade of HIV care among key populations in Indonesia: a prospective cohort study. Lancet HIV. 2018;5(10):e560–8.
Jiamsakul A, Kiertiburanakul S, Ng OT, et al. Long-term loss to follow-up in the TREAT asia HIV observational database (TAHOD). HIV Med. 2019;20(7):439–49.
Jose S, Delpech V, Howarth A, et al. A continuum of HIV care describing mortality and loss to follow-up: a longitudinal cohort study. Lancet HIV. 2018;5(6):e301–8.
Sheehan DM, Fennie KP, Mauck DE, Maddox LM, Lieb S, Trepka MJ. Retention in HIV care and viral suppression: individual- and neighborhood-level predictors of racial/ethnic differences, Florida, 2015. AIDS Patient Care STDS. 2017;31(4):167–75.
Anderson AN, Higgins CM, Haardorfer R, Holstad MM, Nguyen MLT, Waldrop-Valverde D. Disparities in retention in care among adults living with HIV/AIDS: a systematic review. AIDS Behav. 2020;24(4):985–97.
Balde A, Lievre L, Maiga AI, et al. Risk factors for loss to follow-up, transfer or death among people living with HIV on their first antiretroviral therapy regimen in Mali. HIV Med. 2019;20(1):47–53.
Ridgway JP, Almirol EA, Schmitt J, Schuble T, Schneider JA. Travel time to clinic but not neighborhood crime rate is associated with retention in care among HIV-positive patients. AIDS Behav. 2018;22(9):3003–8.
Jerene D, Abebe W, Taye K, Ruff A, Hallstrom I. Adolescents living with HIV are at higher risk of death and loss to follow up from care: analysis of cohort data from eight health facilities in Ethiopia. PLoS One. 2019;14(10):e0223655.
Berheto TM, Haile DB, Mohammed S. Predictors of loss to follow-up in patients living with HIV/AIDS after initiation of antiretroviral therapy. N Am J Med Sci. 2014;6(9):453–9.
Clouse K, Pettifor A, Maskew M, et al. Initiating antiretroviral therapy when presenting with higher CD4 cell counts results in reduced loss to follow-up in a resource-limited setting. AIDS. 2013;27(4):645–50.
De La Mata NL, Ly PS, Nguyen KV, et al. Loss to follow-up trends in HIV-positive patients receiving antiretroviral treatment in asia from 2003 to 2013. J Acquir Immune Defic Syndr. 2017;74(5):555–62.
Seifu W, Ali W, Meresa B. Predictors of loss to follow up among adult clients attending antiretroviral treatment at Karamara general hospital, Jigjiga town, Eastern Ethiopia, 2015: a retrospective cohort study. BMC Infect Dis. 2018;18(1):280.
Elopre L, Hook EW, Westfall AO, et al. The role of early HIV status disclosure in retention in HIV care. AIDS Patient Care STDS. 2015;29(12):646–50.
Rothman AJ. Toward a theory-based analysis of behavioral maintenance. Health Psychol. 2000;19(1s):64–9.
Li TS, Tubiana R, Katlama C, Calvez V, Mohand HA, Autran B. Long-lasting recovery in CD4 T-cell function and viral-load reduction after highly active antiretroviral therapy in advanced HIV-1 disease. Lancet. 1998;351(9117):1682–6.
The Strategies for Management of Antiretroviral Therapy Study G. Major clinical outcomes in antiretroviral therapy (ART)–naive participants and in those not receiving ART at baseline in the SMART study. J Infect Dis. 2008;197(8):1133–44.
Kim MJ, Kim SW, Chang HH, et al. Comparison of antiretroviral regimens: adverse effects and tolerability failure that cause regimen switching. Infect Chemother. 2015;47(4):231–8.
Shroufi A, Van Cutsem G, Cambiano V, et al. Simplifying switch to second-line antiretroviral therapy in sub Saharan Africa: predicted effect of using a single viral load to define efavirenz-based first-line failure. AIDS. 2019;33(10):1635–44.
Pence BW, Bengtson AM, Boswell S, et al. Who will show? predicting missed visits among patients in routine HIV primary care in the United States. AIDS Behav. 2019;23(2):418–26.
Rohr JK, Ive P, Horsburgh CR, et al. Developing a predictive risk model for first-line antiretroviral therapy failure in South Africa. J Int AIDS Soc. 2016;19(1):20987.
Woodward B, Person A, Rebeiro P, Kheshti A, Raffanti S, Pettit A. Risk prediction tool for medical appointment attendance among HIV-infected persons with unsuppressed viremia. AIDS Patient Care STDS. 2015;29(5):240–7.
World Health Organization. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection recommendations for a public health approach—second edition. 2016. Available at: https://apps.who.int/iris/bitstream/handle/10665/208825/9789241549684_eng.pdf?sequence=1. Accessed 2 Dec 2020.
China Center for Disease Control and Prevention. Renewed guideline on the use of free antiretroviral therapy for the people living with HIV/AIDS. 2016. Available at: http://www.chinacdc.cn/jgxx/zgjkzxb/178_9730/03/201612/t20161220_136713.html. Accessed 2 Dec 2020.
UNAIDS. Country progress report—China. 2018. Available at: https://www.unaids.org/sites/default/files/country/documents/CHN_2018_countryreport.pdf. Accessed 2 Dec 2020.
National Health Commission of the People’s Republic of China. New progress in the fight against AIDS in China in 2019. 2019. Available at: http://www.nhc.gov.cn/jkj/s3586/201911/c2388ce70bdd404ea6dfcd886591784d.shtml. Accessed 2 Dec 2020.
Zhu H, Napravnik S, Eron J, et al. Attrition among human immunodeficiency virus (HIV)- infected patients initiating antiretroviral therapy in China, 2003–2010. PLoS One. 2012;7(6):e39414.
Kang R, Luo L, Chen H, et al. Treatment outcomes of initial differential antiretroviral regimens among HIV patients in Southwest China: comparison from an observational cohort study. BMJ Open. 2019;9(3):e025666.
Tang Z, Pan SW, Ruan Y, et al. Effects of high CD4 cell counts on death and attrition among HIV patients receiving antiretroviral treatment: an observational cohort study. Sci Rep. 2017;7(1):3129.
Guangzhou Eighth People’s Hospital. Introduction to the infectious clinic. 2019. Available at: http://www.gz8h.com.cn/info/1499/2601.htm. Accessed 2 Dec 2020.
Ma Y, Zhang F, Zhao Y, et al. Cohort profile: the Chinese national free antiretroviral treatment cohort. Int J Epidemiol. 2010;39(4):973–9.
Haas AD, Tenthani L, Msukwa MT, et al. Retention in care during the first 3 years of antiretroviral therapy for women in Malawi’s option B+ programme: an observational cohort study. Lancet HIV. 2016;3(4):e175–82.
Chi BH, Yiannoutsos CT, Westfall AO, et al. Universal definition of loss to follow-up in HIV treatment programs: a statistical analysis of 111 facilities in Africa, Asia, and Latin America. PLoS Med. 2011;8(10):e1001111.
Nordentoft PB, Engell-Sorensen T, Jespersen S, et al. Assessing factors for loss to follow-up of HIV infected patients in Guinea-Bissau. Infection. 2017;45(2):187–97.
Mugavero MJ, Davila JA, Nevin CR, Giordano TP. From access to engagement: measuring retention in outpatient HIV clinical care. AIDS Patient Care STDS. 2010;24(10):607–13.
China Center for Disease Control and Prevention. National manual on free antiretroviral treatment. 4th edn. Beijing: People’s Medical Publishing House; 2016.
Steyerberg EW, Harrell FE Jr, Borsboom GJ, Eijkemans MJ, Vergouwe Y, Habbema JD. Internal validation of predictive models: efficiency of some procedures for logistic regression analysis. J Clin Epidemiol. 2001;54(8):774–81.
Grimsrud A, Cornell M, Schomaker M, et al. CD4 count at antiretroviral therapy initiation and the risk of loss to follow-up: results from a multicentre cohort study. J Epidemiol Community Health. 2016;70(6):549–55.
Sayegh CS, Wood SM, Belzer M, Dowshen NL. Comparing different measures of retention in care among a cohort of adolescents and young adults living with behaviorally-acquired HIV. AIDS Behav. 2020;24(1):304–10.
Van Beckhoven D, Florence E, Ruelle J, et al. Good continuum of HIV care in Belgium despite weaknesses in retention and linkage to care among migrants. BMC Infect Dis. 2015;15:496.
Elul B, Lamb MR, Lahuerta M, et al. A combination intervention strategy to improve linkage to and retention in HIV care following diagnosis in Mozambique: a cluster-randomized study. PLoS Med. 2017;14(11):e1002433.
Gardner LI, Giordano TP, Marks G, et al. Enhanced personal contact with HIV patients improves retention in primary care: a randomized trial in 6 US HIV clinics. Clin Infect Dis. 2014;59(5):725–34.
Chen WT, Shiu CS, Yang JP, et al. Antiretroviral therapy (art) side effect impacted on quality of life, and depressive symptomatology: a mixed-method study. J AIDS Clin Res. 2013;4:218.
Abgrall S, Ingle SM, May MT, et al. Durability of first ART regimen and risk factors for modification, interruption or death in HIV-positive patients starting ART in Europe and North America 2002–2009. AIDS. 2013;27(5):803–13.
Trickey A, May MT, Vehreschild J-J, et al. Survival of HIV-positive patients starting antiretroviral therapy between 1996 and 2013: a collaborative analysis of cohort studies. Lancet HIV. 2017;4(8):e349–56.
Fan X, She R, Liu C, et al. Evaluation of smartphone APP-based case-management services among antiretroviral treatment-naive HIV-positive men who have sex with men: a randomized controlled trial protocol. BMC Public Health. 2020;20(1):85.
Silva DS, De Boni RB, Lake JE, et al. Retention in early care at an HIV outpatient clinic in Rio de Janeiro, Brazil, 2000–2013. AIDS Behav. 2016;20(5):1039–48.
Bulsara SM, Wainberg ML, Newton-John TRO. Predictors of adult retention in HIV care: a systematic review. AIDS Behav. 2018;22(3):752–64.
Nachega JB, Marconi VC, van Zyl GU, et al. HIV treatment adherence, drug resistance, virologic failure: evolving concepts. Infect Disord Drug Targets. 2011;11(2):167–74.
Fox MP, Bor J, Brennan AT, et al. Estimating retention in HIV care accounting for patient transfers: a national laboratory cohort study in South Africa. PLoS Med. 2018;15(6):e1002589.
Funding
This study was funded by the National Natural Science Foundation of China (Grant No. 71774178), Science and Technology Planning Project of Guangdong (Grant No. 2017A020212006), the National Science and Technology Major Project of the Ministry of Science and Technology of China (Grant No. 2018ZX10715004), Chinese 13th Five-Year National Science and Technology Major Project (2018ZX10302103-002, 2017ZX10202101-003), and the Major Project of Health Care Collaborative Innovation of Guangzhou Science and Technology Innovation Commission (201803040002).
Author information
Authors and Affiliations
Contributions
JG, LL, and JX developed the research questions, designed the study. LL, WC, CL, HZ, PD, and QL contributed to the acquisition of the data. JX and XC conducted the data analyses for this manuscript. JX and JG wrote the manuscript. CL, HZ, PD, and QL assisted with the interpretation of the data. CH, JTL, YH and WC revised the manuscript. All authors critically reviewed and edited the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was approved by the Institutional Review Board (IRB) of the School of Public Health, Sun Yat-sen University, Guangzhou, China (No. 2019-139).
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Xie, J., Gu, J., Chen, X. et al. Baseline and Process Factors of Anti-Retroviral Therapy That Predict Loss to Follow-up Among People Living with HIV/AIDS in China: A Retrospective Cohort Study. AIDS Behav 26, 1126–1137 (2022). https://doi.org/10.1007/s10461-021-03466-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-021-03466-8