Abstract
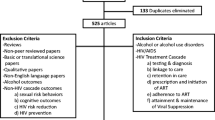
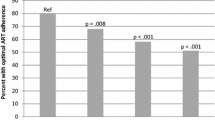
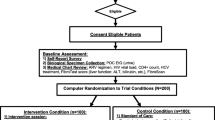
We evaluated associations between levels of alcohol use and HIV care continuum components using national Veterans Aging Cohort Study data for all patients with HIV and AUDIT-C screening (2/1/2008–9/30/2014). Poisson regression models evaluated associations between alcohol use levels (non-drinking, low-, medium-, high-, and very high-level drinking) and: (1) engagement with care (documented CD4 cells/µl or viral load copies/ml labs), (2) ART treatment (≥ 1 prescription), and (3) viral suppression (HIV RNA < 500 copies/ml) within one year. Among 33,224 patients, alcohol use level was inversely associated with all care continuum outcomes (all p < 0.001). Adjusted prevalence of care engagement ranged from 77.8% (95% CI 77.1–78.4%) for non-drinking to 69.1% (66.6–71.6%) for high-level drinking. The corresponding range for ART treatment was 74.0% (73.3–74.7%) to 60.1% (57.3–62.9%) and for viral suppression was 57.3% (56.5–58.1%) to 38.3% (35.6–41.1%). Greater alcohol use is associated with suboptimal HIV treatment across the HIV care continuum.


Similar content being viewed by others
References
Hall HI, Geduld J, Boulos D, et al. Epidemiology of HIV in the United States and Canada: current status and ongoing challenges. J Acquir Immune Defic Syndr. 2009;51(Suppl 1):S13–20.
Lansky A, Brooks JT, DiNenno E, Heffelfinger J, Hall HI, Mermin J. Epidemiology of HIV in the United States. J Acquir Immune Defic Syndr. 2010;55(Suppl 2):64–8.
Centers for Disease Control and Prevention. HIV Surveillance Report: diagnoses of HIV infection and AIDS in the United States and dependent areas, vol. 23; 2011.
Centers for Disease Control and Prevention. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 U.S. dependent areas—2010, vol. 17: HIV Surveillance Supplemental Report; 2012.
Taddei TH, Lo Re V III, Justice AC. HIV, aging, and viral coinfections: taking the long view. Curr HIV/AIDS Rep. 2016;13(5):269–78.
Centers for Disease Control and Prevention. Understanding the HIV Care Continuum. Atlanta, GA: CDC. 2017. https://www.cdc.gov/hiv/pdf/library/factsheets/cdc-hiv-care-continuum.pdf.
Joint United Nations Programme on HIV/AIDS. 90-90-90—an ambitious treatment target to help end the AIDS epidemic. 2014. http://www.unaids.org/en/resources/documents/2014/90-90-90.
Skarbinski J, Rosenberg E, Paz-Bailey G, et al. Human immunodeficiency virus transmission at each step of the care continuum in the United States. JAMA Intern Med. 2015;175(4):588–96.
Mugavero MJ, Amico KR, Horn T, Thompson MA. The state of engagement in HIV care in the United States: from cascade to continuum to control. Clin Infect Dis. 2013;57(8):1164–71.
Bor J, Geldsetzer P, Venkataramani A, Barnighausen T. Quasi-experiments to establish causal effects of HIV care and treatment and to improve the cascade of care. Curr Opin HIV AIDS. 2015;10(6):495–501.
Cohen SM, Hu X, Sweeney P, Johnson AS, Hall HI. HIV viral suppression among persons with varying levels of engagement in HIV medical care, 19 US jurisdictions. J Acquir Immune Defic Syndr. 2014;67(5):519–27.
Park WB, Choe PG, Kim SH, et al. One-year adherence to clinic visits after highly active antiretroviral therapy: a predictor of clinical progress in HIV patients. J Intern Med. 2007;261(3):268–75.
Williams EC, Joo YS, Lipira L, Glass JE. Psychosocial stressors and alcohol use, severity, and treatment receipt across human immunodeficiency virus (HIV) status in a nationally representative sample of US residents. Subst Abus. 2016;38(3):269–77.
Fatch R, Bellows B, Bagenda F, Mulogo E, Weiser S, Hahn JA. Alcohol consumption as a barrier to prior HIV testing in a population-based study in rural Uganda. AIDS Behav. 2013;17(5):1713–23.
Vagenas P, Ludford KT, Gonzales P, et al. Being unaware of being HIV-infected is associated with alcohol use disorders and high-risk sexual behaviors among men who have sex with men in Peru. AIDS Behav. 2014;18(1):120–7.
Bengtson AM, L’Engle K, Mwarogo P, King’ola N. Levels of alcohol use and history of HIV testing among female sex workers in Mombasa, Kenya. AIDS Care. 2014;26(12):1619–24.
Heimer R, Usacheva N, Barbour R, Niccolai LM, Uuskula A, Levina OS. Engagement in HIV care and its correlates among people who inject drugs in St Petersburg, Russian Federation and Kohtla-Jarve, Estonia. Addiction. 2017;112(8):1421–31.
Samet JH, Freedberg KA, Stein MD, et al. Trillion virion delay: time from testing positive for HIV to presentation for primary care. Arch Intern Med. 1998;158(7):734–40.
Korthuis PT, Fiellin DA, McGinnis KA, et al. Unhealthy alcohol and illicit drug use are associated with decreased quality of HIV care. J Acquir Immune Defic Syndr. 2012;61(2):171–8.
Samet JH, Freedberg KA, Savetsky JB, Sullivan LM, Stein MD. Understanding delay to medical care for HIV infection: the long-term non-presenter. AIDS. 2001;15(1):77–85.
Giordano TP, Visnegarwala F, White AC Jr, et al. Patients referred to an urban HIV clinic frequently fail to establish care: factors predicting failure. AIDS Care. 2005;17(6):773–83.
Samet JH, Freedberg KA, Savetsky JB, Sullivan LM, Padmanabhan L, Stein MD. Discontinuation from HIV medical care: squandering treatment opportunities. J Health Care Poor Underserved. 2003;14(2):244–55.
Monroe AK, Lau B, Mugavero MJ, et al. Heavy alcohol use is associated with worse retention in HIV care. J Acquir Immune Defic Syndr. 2016;73(4):419–25.
Wechsberg WM, van der Horst C, Ndirangu J, et al. Seek, test, treat: substance-using women in the HIV treatment cascade in South Africa. Addict Sci Clin Pract. 2017;12(1):12.
Jean K, Puren A, Cutler E, et al. Level of viral suppression and the cascade of HIV care in a South African semi-urban setting in 2012. AIDS. 2016;30(13):2107–16.
Deiss RG, Mesner O, Agan BK, et al. Characterizing the association between alcohol and HIV virologic failure in a military cohort on antiretroviral therapy. Alcohol Clin Exp Res. 2016;40(3):529–35.
Amirkhanian YA, Kelly JA, DiFranceisco WJ, et al. Predictors of HIV care engagement, antiretroviral medication adherence, and viral suppression among people living with HIV infection in St. Petersburg, Russia. AIDS Behav. 2016;22(3):791–9.
Williams EC, Hahn JA, Saitz R, Bryant K, Lira MC, Samet JH. Alcohol use and human immunodeficiency virus (HIV) infection: current knowledge, implications, and future directions. Alcohol Clin Exp Res. 2016;4(10):2056–72.
Metsch LR, Pugh T, Colfax G. An HIV behavioral intervention gets it right—and shows we must do even better. JAMA Intern Med. 2018;178(4):553–5.
Samet JH, Cheng DM, Libman H, Nunes DP, Alperen JK, Saitz R. Alcohol consumption and HIV disease progression. J Acquir Immune Defic Syndr. 2007;46(2):194–9.
Samet JH, Horton NJ, Meli S, Freedberg KA, Palepu A. Alcohol consumption and antiretroviral adherence among HIV-infected persons with alcohol problems. Alcohol Clin Exp Res. 2004;28(4):572–7.
Fultz SL, Skanderson M, Mole LA, et al. Development and verification of a “virtual” cohort using the National VA Health Information System. Med Care. 2006;44(8 Suppl 2):S25–30.
Department of Veterans Affairs. HIV/hepatitis C QUERI strategic plan. Washington, DC: U.S. Department of Veterans Affairs. 2010. http://www.queri.research.va.gov/about/strategic_plans/hiv.pdf.
Bradley KA, Williams EC, Achtmeyer CE, Volpp B, Collins BJ, Kivlahan DR. Implementation of evidence-based alcohol screening in the Veterans Health Administration. Am J Manag Care. 2006;12(10):597–606.
Bradley KA, DeBenedetti AF, Volk RJ, Williams EC, Frank D, Kivlahan DR. AUDIT-C as a brief screen for alcohol misuse in primary care. Alcohol Clin Exp Res. 2007;31(7):1208–17.
Rubinsky AD, Dawson DA, Williams EC, Kivlahan DR, Bradley KA. AUDIT-C scores as a scaled marker of mean daily drinking, alcohol use disorder severity, and probability of alcohol dependence in a U.S. general population sample of drinkers. Alcohol Clin Exp Res. 2013;37(8):1380–90.
Justice AC, Dombrowski E, Conigliaro J, et al. Veterans Aging Cohort Study (VACS): overview and description. Med Care. 2006;44(8 Suppl 2):S13–24.
Williams EC, Lapham GT, Shortreed SM, et al. Among patients with unhealthy alcohol use, those with HIV are less likely than those without to receive evidence-based alcohol-related care: a national VA study. Drug Alcohol Depend. 2017;174:113–20.
Bradley KA, Bush KR, Epler AJ, et al. Two brief alcohol-screening tests from the Alcohol Use Disorders Identification Test (AUDIT): validation in a female Veterans Affairs patient population. Arch Intern Med. 2003;163(7):821–9.
Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med. 1998;158(16):1789–95.
Rubinsky AD, Kivlahan DR, Volk RJ, Maynard C, Bradley KA. Estimating risk of alcohol dependence using alcohol screening scores. Drug Alcohol Depend. 2010;108(1–2):29–36.
Williams EC, Bryson CL, Sun H, et al. Association between alcohol screening results and hospitalizations for trauma in Veterans Affairs outpatients. Am J Drug Alcohol Abuse. 2012;38(1):73–80.
Williams EC, Bradley KA, Gupta S, Harris AH. Association between alcohol screening scores and mortality in black, Hispanic, and white male veterans. Alcohol Clin Exp Res. 2012;36(12):2132–40.
Williams EC, Bradley KA, Balderson BH, et al. Alcohol and associated characteristics among older persons living with HIV on antiretroviral therapy. Subst Abus. 2014;35(3):245–53.
Au DH, Kivlahan DR, Bryson CL, Blough D, Bradley KA. Alcohol screening scores and risk of hospitalizations for GI conditions in men. Alcohol Clin Exp Res. 2007;31(3):443–51.
Bryson CL, Au DH, Sun H, Williams EC, Kivlahan DR, Bradley KA. Alcohol screening scores and medication nonadherence. Ann Intern Med. 2008;149(11):795–804.
Williams EC, Bryson CL, Sun H, Au DH, Bradley KA. Association between alcohol use and angina symptoms among outpatients from the Veterans Health Administration. J Addict Med. 2018;12(2):143–9.
Justice AC, McGinnis KA, Tate JP, et al. Risk of mortality and physiologic injury evident with lower alcohol exposure among HIV infected compared with uninfected men. Drug Alcohol Depend. 2016;161:95–103.
Harris AH, Bradley KA, Bowe T, Henderson P, Moos R. Associations between AUDIT-C and mortality vary by age and sex. Popul Health Manag. 2010;13(5):263–8.
Harris AH, Bryson CL, Sun H, Blough D, Bradley KA. Alcohol screening scores predict risk of subsequent fractures. Subst Use Misuse. 2009;44(8):1055–69.
Rittmueller SE, Frey MS, Williams EC, Sun H, Bryson CL, Bradley KA. Association between alcohol use and cardiovascular self-care behaviors among male hypertensive Veterans Affairs outpatients: a cross-sectional study. Subst Abus. 2015;36(1):6–12.
Thomas RM, Francis GPA, Williams EC, et al. Association between alcohol screening scores and diabetic self-care behaviors. Fam Med. 2012;44(8):555–63.
Chavez LJ, Williams EC, Lapham G, Bradley KA. Association between alcohol screening scores and alcohol-related risks among female Veterans affairs patients. J Stud Alcohol Drugs. 2012;73(3):391–400.
Chavez LJ, Liu CF, Tefft N, et al. Unhealthy alcohol use in older adults: association with readmissions and emergency department use in the 30 days after hospital discharge. Drug Alcohol Depend. 2016;158:94–101.
Rubinsky AD, Sun H, Blough DK, et al. AUDIT-C alcohol screening results and postoperative inpatient health care use. J Am Coll Surg. 2012;214(3):296–305.e1.
Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–6.
Shaper AG, Wannamethee G, Walker M. Alcohol and mortality in British men: explaining the U-shaped curve. Lancet. 1988;2(8623):1267–73.
StataCorp. Stata Statistical Software: Release 14, College Station, TX: StataCorp LP. 2015.
Cunningham WE, Sohler NL, Tobias C, et al. Health services utilization for people with HIV infection: comparison of a population targeted for outreach with the U.S. population in care. Med Care. 2006;44(11):1038–47.
Hahn JA, Samet JH. Alcohol and HIV disease progression: weighing the evidence. Curr HIV/AIDS Rep. 2010;7(4):226–33.
Hendershot CS, Stoner SA, Pantalone DW, Simoni JM. Alcohol use and antiretroviral adherence: review and meta-analysis. J Acquir Immune Defic Syndr. 2009;52(2):180–202.
Moore RD, Bartlett JG. Dramatic decline in the HIV-1 RNA level over calendar time in a large urban HIV practice. Clin Infect Dis. 2011;53(6):600–4.
Gordon LL, Gharibian D, Chong K, Chun H. Comparison of HIV virologic failure rates between patients with variable adherence to three antiretroviral regimen types. AIDS Patient Care STDS. 2015;29(7):384–8.
Bangsberg DR. Less than 95% adherence to nonnucleoside reverse-transcriptase inhibitor therapy can lead to viral suppression. Clin Infect Dis. 2006;43(7):939–41.
Justice AC, Lasky E, McGinnis KA, et al. Medical disease and alcohol use among veterans with human immunodeficiency infection: a comparison of disease measurement strategies. Med Care. 2006;44(8 Suppl 2):S52–60.
McGinnis KA, Tate JP, Williams EC, et al. Comparison of AUDIT-C collected via electronic medical record and self-administered research survey in HIV infected and uninfected patients. Drug Alcohol Depend. 2016;168:196–202.
Williams EC, Achtmeyer CE, Thomas RM, et al. Factors underlying quality problems with alcohol screening prompted by a clinical reminder in primary care: a Multi-site Qualitative Study. J Gen Intern Med. 2015;30(8):1125–32.
Bradley KA, Lapham GT, Hawkins EJ, et al. Quality concerns with routine alcohol screening in VA clinical settings. J Gen Intern Med. 2011;26(3):299–306.
Funding
This study was funded by a grant from the National Institute on Alcohol Abuse and Alcoholism (R21AA022866-01; Williams/Bradley PIs) and by COMpAAAS/Veterans Aging Cohort Study (U24-AA020794, U01-AA020790, U01-AA020795,U01-AA020799; U10 AA013566). Dr. Williams is supported by a Career Development Award from VA Health Services Research & Development (CDA 12-276); Dr. Bradley is supported by a mid-career mentoring award from the National Institute on Alcohol Abuse and Alcoholism (K24-AA022128). The funders of this study had no role in study design, data collection, analysis, interpretation and presentation, or in the decision to submit the manuscript for publication. Views presented in the manuscript are those of the authors and do not reflect those of the University of Washington, the Department of Veterans Affairs, or the United States Government.
Author information
Authors and Affiliations
Contributions
Data for this study were obtained from the Veterans Aging Cohort Study (PI: Amy Justice, MD, PhD). All authors contributed to study design, protocol development, and data interpretation.
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Bradley owns stock in Pfizer Pharmaceuticals. All other authors declare no potential conflicts of interest. Preliminary findings of this research study were presented at the Addictions Health Services Research (AHSR) Conference in Madison, WI in September 2017.
Ethical Approval
For this type of study, formal consent is not required. The study, including waivers of written consent and HIPAA authorization, was approved by Internal Review Boards at VA Connecticut Healthcare System and VA Puget Sound.
Appendices
Appendix 1: List of Antiretroviral Medications
Zidovudine |
Didanosine |
Zalcitabine |
Stavudine |
Lamivudine |
Lamivudine/zidovudine |
Abacavir |
Indinavir |
Ritonavir |
Saquinavir |
Nelfinavir |
Amprenavir |
Nevirapine |
Delavirdine |
Efavirenz |
Lopinavir/ritonavir |
Tenofovir |
Abacavir/lamivudine/zidovudine |
Emtricitabine |
Atazanavir |
Fosamprenavir |
Lopinavir |
Emtricibine/tenofovir |
Abacavir/lamividine |
Enfuvirtide |
Adefovir |
Tipranavir |
Darunavir |
Efavirenz/emtricitabine/tenofovir |
Etravirine |
Maraviroc |
Raltegravir |
Elvitegravir/cobicistat/emtricitabine/tenofovir |
Rilpivirine |
Emtricitabine/rilpivirine/tenofovir |
Dolutegravir |
Elvitegravir |
Abacavir/dolutegravir/lamivudine |
Cobicistat |
Cobicistat/darunavir |
Atazanavir/cobicistat |
Cobicistat/elvitegravir/emtricitabine/tenofovir |
Appendix 2
See Fig. 3.
Rights and permissions
About this article
Cite this article
Williams, E.C., McGinnis, K.A., Edelman, E.J. et al. Level of Alcohol Use Associated with HIV Care Continuum Targets in a National U.S. Sample of Persons Living with HIV Receiving Healthcare. AIDS Behav 23, 140–151 (2019). https://doi.org/10.1007/s10461-018-2210-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-018-2210-6