Abstract
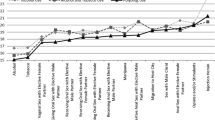
Stimulant drug use is associated with numerous health problems among men who have sex with men (MSM). This paper describes how stimulant drug use changes over a four and one-half year period from 2003 until 2008. Participants were 2,389 men (17,222 person-visits) from The Multicenter AIDS Cohort Study (MACS)—an ongoing, prospective study of HIV infection among MSM. Group-based trajectory analyses of data from these men over the study period yielded a four groups solution: consistent users (9.8%), men whose use increased (5.4%), men whose use declined (6.9%), and abstinent or rarely-using men (77.9%). There were significant differences between groups in terms of demographic, behavioral risk and HIV serostatus. Men who increased or decreased stimulant drug use over time reported congruent changes in sexual risk taking. The fact that sexual risk levels parallel stimulant drug use over time suggests that finding ways to lower rates of stimulant drug use among MSM could be a tool in HIV prevention.

Similar content being viewed by others
References
Page-Shafer K, Veugelers PJ, Moss AR, Strathdee S, Kaldor JM, van Griensven GJ. Sexual risk behavior and risk factors for HIV-1 seroconversion in homosexual men participating in the Tricontinental Seroconverter Study, 1982–1994. Am J Epidemiol. 1997;146(7):531–42.
Chesney MA, Barrett DC, Stall R. Histories of substance use and risk behavior: precursors to HIV seroconversion in homosexual men. Am J Public Health. 1998;88(1):113–6.
Buchacz K, McFarland W, Kellogg TA, et al. Amphetamine use is associated with increased HIV incidence among men who have sex with men in San Francisco. AIDS. 2005;19(13):1423–4.
Koblin BA, Husnik MJ, Colfax G, et al. Risk factors for HIV infection among men who have sex with men. AIDS. 2006;20(5):731–9.
Plankey MW, Ostrow DG, Stall R, et al. The relationship between methamphetamine and popper use and risk of HIV seroconversion in the Multicenter AIDS Cohort Study. J Acquir Immune Defic Syndr. 2007;45(1):85–92.
Molitor F, Truax SR, Ruiz JD, Sun RK. Association of methamphetamine use during sex with risky sexual behaviors and HIV infection among non-injection drug users. West J Med. 1998;168(2):93–7.
Diamond C, Thiede H, Perdue T, et al. Seroepidemiology of human herpesvirus 8 among young men who have sex with men. Sex Transm Dis. 2001;28(3):176–83.
Hirshfield S, Remien RH, Walavalkar I, Chiasson MA. Crystal methamphetamine use predicts incident STD infection among men who have sex with men recruited online: a nested case-control study. J Med Internet Res. 2004;6(4):e41.
Wong W, Chaw JK, Kent CK, Klausner JD. Risk factors for early syphilis among gay and bisexual men seen in an STD clinic: San Francisco, 2002–2003. Sex Transm Dis. 2005;32(7):458–63.
Reback CJ, Kamien JB, Amass L. Characteristics and HIV risk behaviors of homeless, substance-using men who have sex with men. Addict Behav. 2007;32(3):647–54.
Semple SJ, Patterson TL, Grant I. Binge use of methamphetamine among HIV-positive men who have sex with men: pilot data and HIV prevention implications. AIDS Educ Prev. 2003;15(2):133–47.
Klitzman RL, Greenberg JD, Pollack LM, et al. MDMA (‘ecstasy’) use, and its association with high risk behaviors, mental health, and other factors among gay/bisexual men in New York City. Drug Alcohol Depend. 2002;66(2):115–25.
Redfearn PJ, Agrawal N, Mair LH. An association between the regular use of 3,4 methylenedioxy-methamphetamine (ecstasy) and excessive wear of the teeth. Addiction. 1998;93(5):745–8.
Richards JR, Brofeldt BT. Patterns of tooth wear associated with methamphetamine use. J Periodontol. 2000;71(8):1371–4.
Mansergh G, Purcell DW, Stall R, et al. CDC consultation on methamphetamine use and sexual risk behavior for HIV/STD infection: summary and suggestions. Public Health Rep. 2006;121(2):127–32.
Colfax G, Coates TJ, Husnik MJ, et al. Longitudinal patterns of methamphetamine, popper (amyl nitrite), and cocaine use and high-risk sexual behavior among a cohort of San Francisco men who have sex with men. J Urban Health. 2005;82(11):62–70.
Jacobs A. In clubs, a potent drug stirs fear of an epidemic. The New York Times. 2002 Jan 29; Sect. B:1.
Kurtz SP. Post-circuit blues: motivations and consequences of crystal meth use among gay men in Miami. AIDS Behav. 2005;9(1):63–72.
O’Bryan W. Crystal and the community: a grassroots alliance gains momentum in its fight against methamphetamines. Metro Weekly-Washington 2005. http://www.metroweekly.com/feature/?ak=1672. Cited Oct 25 2009.
Kaslow RA, Ostrow DG, Detels R, Phair JP, Polk BF, Rinaldo CR Jr. The Multicenter AIDS Cohort Study: rationale, organization, and selected characteristics of the participants. Am J Epidemiol. 1987;126(2):310–8.
Detels R, Phair JP, Saah AJ, et al. Recent scientific contributions to understanding HIV/AIDS from the Multicenter AIDS Cohort Study. J Epidemiol. 1992;2:S11–9.
Dudley J, Jin S, Hoover D, Metz S, Thackeray R, Chmiel J. The Multicenter AIDS Cohort Study: retention after 9 1/2 years. Am J Epidemiol. 1995;142(3):323–30.
Ostrow DG. The role of drugs in the sexual lives of men who have sex with men: continuing barriers to researching this question. AIDS Behav. 2000;4(2):205–19.
Ostrow DG, Plankey MW, Cox C, et al. Specific sex drug combinations contribute to the majority of recent HIV seroconversions among MSM in the MACS. J Acquir Immune Defic Syndr. 2009;51(3):349–55.
Gribble JN, Miller HG, Cooley PC, et al. The impact of T-ACASI interviewing on reported drug use among men who have sex with men. Subst Use Misuse. 2000;35(6–8):869–90.
Nagin D. Analyzing developmental trajectories: a semi-parametric group-based approach. Psychol Methods. 1999;4:139–57.
Nagin D. Group-based modeling of development. Cambridge, MA: Harvard University Press; 2005.
Raudenbush SW, Bryk AS. Hierarchical linear models: applications and data analysis methods. 2nd ed. Advanced quantitative techniques in the social sciences series 1. Thousand Oaks, CA: Sage Publications; 2002.
Singer JD. Using SAS proc mixed to fit multilevel models, hierarchical models, and individual growth models. J Educ Behav Stat. 1998;23(4):323–55.
Substance Abuse and Mental Health Services Administration, Office of Applied Studies. National Household Survey on Drug Abuse: summary of findings from 1999. Department of Health and Human Services: Rockville, MD; 2000.
Grov C, Parsons JT, Bimbi DS. In the shadows of a prevention campaign: sexual risk behavior in the absence of crystal methamphetamine. AIDS Educ Prev. 2008;20(1):42–55.
Acknowledgments
Support for this study was provided by National Institute of Drug Abuse grant R01 DA022936. We would also sincerely like to thank the men who have participated in the MACS since its inception for their immense contribution to HIV research. This article is dedicated to the memory of Keith Bussy, a man whose tireless advocacy for HIV infected men improved the lives of countless people. His dedication and constant smile were an inspiration to all who knew him.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lim, S.H., Ostrow, D., Stall, R. et al. Changes in Stimulant Drug Use Over Time in the MACS: Evidence for Resilience Against Stimulant Drug Use Among Men Who Have Sex with Men. AIDS Behav 16, 151–158 (2012). https://doi.org/10.1007/s10461-010-9866-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-010-9866-x