Abstract
The investigation of magnetohydrodynamic (MHD) blood flow within configurations that are pertinent to the human anatomy holds significant importance in the realm of scientific inquiry because of its practical implications within the medical field. This article presents an exhaustive appraisal of the diverse applications of magnetohydrodynamics and their computational modeling in biological contexts. These applications are classified into two categories: simple flow and pulsatile flow. An alternative approach of traditional CFD methods called Lattice Boltzmann Method (LBM), a mesoscopic method based on kinetic theory, is introduced to solve complex problems, such as hemodynamics. The results show that the flow velocity reduces considerably by increasing the magnetic field intensity, and the flow separation area is minimized by the increase of magnetic field strength. The LBM with BGK collision model has shown good results in terms of precision. Finally, this literature review has revealed a number of potential avenues for further research. Suggestions for future works are proposed accordingly.

(Figure reprinted from Shit and Majee [167])

(Figure reprinted from Javadzadegan et al. [170])


(Figure reprinted from Teimouri et al. [176])




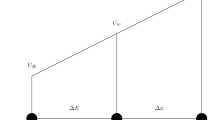
(Figure reprinted from Cherkaoui et al. [147])

(Figure reprinted from Cherkaoui et al. [147])

(Figure reprinted from Cherkaoui et al. [147])

(Figure reprinted from Cherkaoui et al. [147])

Similar content being viewed by others
References
World Health Organization. Cardiovascular diseases (CVDS). www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds)
Basu, D., and R. Kulkarni. Overview of blood components and their preparation. Indian J. Anaesth. 2014. https://doi.org/10.4103/0019-5049.144647.
Campinho, P., A. Vilfan, and J. Vermot. Blood flow forces in shaping the vascular system: a focus on endothelial cell behavior. Front. Physiol. 2020. https://doi.org/10.3389/fphys.2020.00552.
Arthur, M. D., C. Guyton, Ph. D. John, and E. Hall. Textbook of Medical Physiology. Elsevier, New York 2006.
Saqr, K. M., S. Tupin, S. Rashad, T. Endo, K. Niizuma, T. Tominaga, and M. Ohta. Physiologic blood flow is turbulent. Sci. Rep. 2020. https://doi.org/10.1038/s41598-020-72309-8.
Serrette, R. L. An introduction to the finite element method using basic programs. Mech. Mach. Theory. 1992. https://doi.org/10.1016/0094-114x(92)90073-q.
Turner, M. J., R. W. Clough, H. C. Martin, and L. J. Topp. Stiffness and deflection analysis of complex structures. J. Aeronaut. Sci. 23:805–823, 1956. https://doi.org/10.2514/8.3664.
Girault, V., and P. A. Raviart. An analysis of a mixed finite element method for the Navier-Stokes equations. Numer. Math. 33:235–271, 1979. https://doi.org/10.1007/bf01398643.
Johnson, C. Numerical solution of partial differential equations by the finite element method. Math. Comput. 1989. https://doi.org/10.2307/2008668.
Behr, M. A., L. P. Franca, and T. E. Tezduyar. Stabilized finite element methods for the velocity-pressure-stress formulation of incompressible flows. Comput. Methods Appl. Mech. Eng. 104:31–48, 1993. https://doi.org/10.1016/0045-7825(93)90205-c.
Lévêque, E. An introduction to turbulence in fluids, and modelling aspects. EAS Publ. Ser. 21:7–42, 2006. https://doi.org/10.1051/eas:2006105.
Baliga, B. R., and S. V. Patankar. A control volume finite-element method for two-dimensional fluid flow and heat transfer. Numer. Heat Transf. B 6:245–261, 1983. https://doi.org/10.1080/10407798308546969.
Patankar, S.V. Efficient numerical techniques for complex fluid flows—NASA Technical Reports Server (NTRS). Efficient Numerical Techniques for Complex Fluid Flows - NASA Technical Reports Server (NTRS). 2013. https://ntrs.nasa.gov/citations/19890003523.
Patankar, S. V., and D. B. Spalding. A calculation procedure for heat, mass and momentum transfer in three-dimensional parabolic flows. Int. J. Heat Mass Transf. 15:1787–1806, 1972. https://doi.org/10.1016/0017-9310(72)90054-3.
Mohamad, A. A. LBM: fundamentals and engineering applications with computer codes. 2011. https://doi.org/10.2514/1.J051744
Hardy, J., Y. Pomeau, and O. de Pazzis. Time evolution of a two-dimensional classical lattice system. Phys. Rev. Lett. 31:276–279, 1973. https://doi.org/10.1103/physrevlett.31.276.
Frisch, U., B. Hasslacher, and Y. Pomeau. Lattice-gas automata for the Navier-Stokes equation. Phys. Rev. Lett. 56:1505–1508, 1986. https://doi.org/10.1103/physrevlett.56.1505.
McNamara, G. R., and G. Zanetti. Use of the boltzmann equation to simulate lattice-gas automata. Phys. Rev. Lett. 61:2332–2335, 1988. https://doi.org/10.1103/physrevlett.61.2332.
Higuera, F. J., and J. Jiménez. Boltzmann approach to lattice gas simulations. Europhys. Lett. (EPL). 9:663–668, 1989. https://doi.org/10.1209/0295-5075/9/7/009.
Koelman, J. M. V. A. A simple lattice Boltzmann scheme for Navier-Stokes fluid flow. Europhys. Lett. (EPL). 15:603–607, 1991. https://doi.org/10.1209/0295-5075/15/6/007.
Chen, S., H. Chen, D. Martnez, and W. Matthaeus. Lattice Boltzmann model for simulation of magnetohydrodynamics. Phys. Rev. Lett. 67:3776–3779, 1991. https://doi.org/10.1103/physrevlett.67.3776.
Shu, C., Y. Peng, and Y. T. Chew. Simulation of natural convection in a square cavity by taylor series expansion- and least squares-based LBM. Int. J. Mod. Phys. C. 13:1399–1414, 2002. https://doi.org/10.1142/s0129183102003966.
D’Humières, D. Generalized Lattice Boltzmann equations, rarefied gas dynamics: theory and simulations. Prog. Astronaut. Aeronaut. 159:450–458, 1992.
d’Humières, D. Multiple-relaxation-time lattice Boltzmann models in three dimensions. Philos. Trans. R. Soc. Lond. Ser. A 360:437–451, 2002. https://doi.org/10.1098/rsta.2001.0955.
Karlin, I. V., A. Ferrante, and H. C. Öttinger. Perfect entropy functions of the LBM. Europhys. Lett. (EPL). 47:182–188, 1999. https://doi.org/10.1209/epl/i1999-00370-1.
Atif, M., P. K. Kolluru, C. Thantanapally, and S. Ansumali. Essentially entropic lattice Boltzmann model. Phys. Rev. Lett. 2017. https://doi.org/10.1103/physrevlett.119.240602.
Ansumali, S., and I. V. Karlin. Single relaxation time model for entropic lattice Boltzmann methods. Phys. Rev. E. 2002. https://doi.org/10.1103/physreve.65.056312.
Ansumali, S., and I. V. Karlin. Entropy function approach to the lattice Boltzmann method. J. Stat. Phys. 107:291–308, 2002. https://doi.org/10.1023/A:1014575024265.
Ziegler, D. P. Boundary conditions for lattice Boltzmann simulations. J. Stat. Phys. 71:1171–1177, 1993. https://doi.org/10.1007/bf01049965.
Bouzidi, M., M. Firdaouss, and P. Lallemand. Momentum transfer of a Boltzmann-lattice fluid with boundaries. Phys. Fluids. 13:3452–3459, 2001. https://doi.org/10.1063/1.1399290.
Yu, D., R. Mei, and W. Shyy. A unified boundary treatment in lattice Boltzmann method. 41st Aerosp. Sci. Meet. Exhib. 2003. https://doi.org/10.2514/6.2003-953.
Gunstensen, A. K., D. H. Rothman, S. Zaleski, and G. Zanetti. Lattice Boltzmann model of immiscible fluids. Phys. Rev. A. 43:4320–4327, 1991. https://doi.org/10.1103/physreva.43.4320.
Grunau, D., S. Chen, and K. Eggert. A lattice Boltzmann model for multiphase fluid flows. Phys. Fluids A: Fluid Dyn. 5:2557–2562, 1993. https://doi.org/10.1063/1.858769.
Han-Taw, C., and L. Jae-Yuh. Numerical analysis for hyperbolic heat conduction. Int. J. Heat Mass Transf. 36:2891–2898, 1993. https://doi.org/10.1016/0017-9310(93)90108-i.
Ho, J.-R., C.-P. Kuo, W.-S. Jiaung, and C.-J. Twu. Lattice Boltzmann scheme for hyperbolic heat conduction equation. Numer. Heat Transf. B: Fundam. 41:591–607, 2002. https://doi.org/10.1080/10407790190053798.
Gupta, N., G. R. Chaitanya, and S. C. Mishra. Lattice Boltzmann method applied to variable thermal conductivity conduction and radiation problems. J. Thermophys. Heat Transf. 20:895–902, 2006. https://doi.org/10.2514/1.20557.
Bettaibi, S., F. Kuznik, and E. Sediki. Hybrid LBM-MRT model coupled with finite difference method for double-diffusive mixed convection in rectangular enclosure with insulated moving lid. Phys. A: Stat. Mech. Appl. 444:311–326, 2016. https://doi.org/10.1016/j.physa.2015.10.029.
Bettaibi, S., F. Kuznik, and E. Sediki. Hybrid lattice Boltzmann finite difference simulation of mixed convection flows in a lid-driven square cavity. Phys. Lett. A. 378:2429–2435, 2014. https://doi.org/10.1016/j.physleta.2014.06.032.
Mhamdi, B., S. Bettaibi, O. Jellouli, and M. Chafra. MRT-lattice Boltzmann hybrid model for the double diffusive mixed convection with thermodiffusion effect. Nat. Comput. 21:393–405, 2022. https://doi.org/10.1007/s11047-022-09884-4.
Bettaibi, S., E. Sediki, F. Kuznik, and S. Succi. Lattice Boltzmann simulation of mixed convection heat transfer in a driven cavity with non-uniform heating of the Bottom Wall. Commun. Theor. Phys. 63:91–100, 2015. https://doi.org/10.1088/0253-6102/63/1/15.
Bettaibi, S., F. Kuznik, E. Sediki, and S. Succi. Numerical study of thermal diffusion and diffusion thermo effects in a differentially heated and salted driven cavity using MRT-Lattice Boltzmann finite difference model. Int. J. Appl. Mech. 2021. https://doi.org/10.1142/s1758825121500496.
Succi, S. Applied lattice Boltzmann method for transport phenomena, momentum, heat and mass transfer. Can. J. Chem. Eng. 85:946–947, 2008. https://doi.org/10.1002/cjce.5450850617.
Jahanshaloo, L., N. A. C. Sidik, A. Fazeli, H. A, and M. P. An overview of boundary implementation in lattice Boltzmann method for computational heat and mass transfer. Int. Commun. Heat Mass Transf. 78:1–12, 2016. https://doi.org/10.1016/j.icheatmasstransfer.2016.08.014.
Luo, Z., and H. Xu. Numerical simulation of heat and mass transfer through microporous media with lattice Boltzmann method. Therm. Sci. Eng. Prog. 9:44–51, 2019. https://doi.org/10.1016/j.tsep.2018.10.006.
Chen, S., Z. Wang, X. Shan, and G. D. Doolen. Lattice Boltzmann computational fluid dynamics in three dimensions. J. Stat. Phys. 68:379–400, 1992. https://doi.org/10.1007/bf01341754.
Martínez, D. O., S. Chen, and W. H. Matthaeus. Lattice Boltzmann magnetohydrodynamics. Phys. Plasmas. 1:1850–1867, 1994. https://doi.org/10.1063/1.870640.
Bernsdorf, J., G. Brenner, and F. Durst. Numerical analysis of the pressure drop in porous media flow with lattice Boltzmann (BGK) automata. Comput. Phys. Commun. 129:247–255, 2000. https://doi.org/10.1016/s0010-4655(00)00111-9.
Freed, D. M. Lattice-Boltzmann method for macroscopic porous media modeling. Int. J. Mod. Phys. C. 09:1491–1503, 1998. https://doi.org/10.1142/s0129183198001357.
Zhao, Y. Lattice Boltzmann based PDE solver on the GPU. Visual Comput. 24:323–333, 2007. https://doi.org/10.1007/s00371-007-0191-y.
Körner, C., T. Pohl, U. Rüde, N. Thürey, and T. Zeiser. Parallel Lattice Boltzmann methods for CFD applications. Lect. Notes Comput. Sci. Eng. 2006. https://doi.org/10.1007/3-540-31619-1_13.
Pohl, T., M. Kowarschik, J. Wilke, K. Iglberger, and U. Rüde. Optimization and profiling of the cache performance of parallel lattice Boltzmann codes. Parallel Process. Lett. 13:549–560, 2003. https://doi.org/10.1142/s0129626403001501.
Zeiser, T., G. Wellein, A. Nitsure, K. Iglberger, U. Rude, and G. Hager. Introducing a parallel cache oblivious blocking approach for the lattice Boltzmann method. Prog. Comput. Fluid Dyn., Int. J. 8, 2008. https://doi.org/10.1504/pcfd.2008.018088.
Xiong, Q., B. Li, J. Xu, X. Fang, X. Wang, L. Wang, X. He, and W. Ge. Efficient parallel implementation of the lattice Boltzmann method on large clusters of graphic processing units. Chin. Sci. Bull. 57:707–715, 2012. https://doi.org/10.1007/s11434-011-4908-y.
Kabinejadian, F., D. N. Ghista, B. Su, M. Kaabi Nezhadian, L. P. Chua, J. H. Yeo, and H. L. Leo. In vitro measurements of velocity and wall shear stress in a novel sequential anastomotic graft design model under pulsatile flow conditions. Med. Eng. Phys. 36:1233–1245, 2014. https://doi.org/10.1016/j.medengphy.2014.06.024.
Hewlin, R. L., and J. P. Kizito. Development of an experimental and digital cardiovascular arterial model for transient hemodynamic and postural change studies: “a preliminary framework analysis’’. Cardiovasc. Eng. Technol. 9:1–31, 2017. https://doi.org/10.1007/s13239-017-0332-z.
Park, S. M., Y. U. Min, M. J. Kang, K. C. Kim, and H. S. Ji. In vitrohemodynamic study on the stenotic right coronary artery using experimental and numerical analysis. J. Mech. Med. Biol. 10:695–712, 2010. https://doi.org/10.1142/s0219519410003812.
Souza, A., M. S. Souza, D. Pinho, R. Agujetas, C. Ferrera, R. Lima, H. Puga, and J. Ribeiro. 3D manufacturing of intracranial aneurysm biomodels for flow visualizations: low cost fabrication processes. Mech. Res. Commun. 2020. https://doi.org/10.1016/j.mechrescom.2020.103535.
Bento, D., S. Lopes, I. Maia, R. Lima, and J. M. Miranda. Bubbles moving in blood flow in a microchannel network: the effect on the local hematocrit. Micromachines. 2020. https://doi.org/10.3390/mi11040344.
Pinho, D., V. Carvalho, I. M. Gonçalves, S. Teixeira, and R. Lima. Visualization and measurements of blood cells flowing in microfluidic systems and blood rheology: a personalized medicine perspective. J. Pers. Med. 2020. https://doi.org/10.3390/jpm10040249.
Carvalho, V., N. Rodrigues, R. Ribeiro, P. F. Costa, J. C. F. Teixeira, R. A. Lima, and S. F. C. F. Teixeira. Hemodynamic study in 3D printed stenotic coronary artery models: experimental validation and transient simulation. Comput. Methods Biomech. Biomed. Eng. 24:623–636, 2020. https://doi.org/10.1080/10255842.2020.1842377.
Stepniak, K., A. Ursani, N. Paul, and H. Naguib. Development of a phantom network for optimization of coronary artery disease imaging using computed tomography. Biomed. Phys. Eng. Express. 2019. https://doi.org/10.1088/2057-1976/ab2696.
Sjostrand, S., A. Widerstrom, A. R. Ahlgren, and M. Cinthio. Design and fabrication of a conceptual arterial ultrasound phantom capable of exhibiting longitudinal wall movement. IEEE Trans. Ultrason. Ferroelectr. Freq. Control. 64:11–18, 2017. https://doi.org/10.1109/tuffc.2016.2597246.
Papathanasopoulou, P., S. Zhao, U. Köhler, M. B. Robertson, Q. Long, P. Hoskins, X. Yun Xu, and I. Marshall. MRI measurement of time-resolved wall shear stress vectors in a carotid bifurcation model, and comparison with CFD predictions. J. Magn. Reson. Imaging. 17:153–162, 2003. https://doi.org/10.1002/jmri.10243.
Chayer, B., M. van den Hoven, M.-H.R. Cardinal, H. Li, A. Swillens, R. Lopata, and G. Cloutier. Atherosclerotic carotid bifurcation phantoms with stenotic soft inclusions for ultrasound flow and vessel wall elastography imaging. Phys. Med. Biol. 2019. https://doi.org/10.1088/1361-6560/ab1145.
Goudot, G., J. Poree, O. Pedreira, L. Khider, P. Julia, J.-M. Alsac, E. Laborie, T. Mirault, M. Tanter, M. Messas, and M. Pernot. Wall shear stress measurement by ultrafast vector flow imaging for atherosclerotic carotid stenosis. Ultraschall in Der Medizin - Europ. J. Ultrasound. 42:297–305, 2019. https://doi.org/10.1055/a-1060-0529.
Karimi, A., M. Navidbakhsh, A. Shojaei, and S. Faghihi. Measurement of the uniaxial mechanical properties of healthy and atherosclerotic human coronary arteries. Mater. Sci. Eng.: C. 33:2550–2554, 2013. https://doi.org/10.1016/j.msec.2013.02.016.
Karimi, A., M. Navidbakhsh, A. Shojaei, K. Hassani, and S. Faghihi. Study of plaque vulnerability in coronary artery using Mooney-Rivlin model: a combination of finite element and experimental method. Biomed. Eng. Appl. Basis Commun. 2014. https://doi.org/10.4015/s1016237214500136.
Santamore, W. P., P. Walinsky, A. A. Bove, R. H. Cox, R. A. Carey, and J. F. Spann. The effects of vasoconstriction on experimental coronary artery stenosis. Am. Heart J. 100:852–858, 1980. https://doi.org/10.1016/0002-8703(80)90066-6.
Carvalho, V., I. Maia, A. Souza, J. Ribeiro, P. Costa, H. Puga, S. Teixeira, and R. A. Lima. In vitro biomodels in stenotic arteries to perform blood analogues flow visualizations and measurements: a review. Open Biomed. Eng. J. 14:87–102, 2020. https://doi.org/10.2174/1874120702014010087.
Friedman, M. H., and D. P. Giddens. Blood flow in major blood vessels-modeling and experiments. Ann. Biomed. Eng. 33:1710–1713, 2005. https://doi.org/10.1007/s10439-005-8773-1.
Rezvan, A., C.-W. Ni, N. Alberts-Grill, and H. Jo. Animal, In Vitro, andEx VivoModels of Flow-Dependent Atherosclerosis: Role of Oxidative Stress. Antioxid. Redox. Signal. 15:1433–1448, 2011. https://doi.org/10.1089/ars.2010.3365.
Yazdi, S. G., P. H. Geoghegan, P. D. Docherty, M. Jermy, and A. Khanafer. A review of arterial phantom fabrication methods for flow measurement using PIV techniques. Ann. Biomed. Eng. 46:1697–1721, 2018. https://doi.org/10.1007/s10439-018-2085-8.
Fröhlich, E., and S. Salar-Behzadi. Toxicological assessment of inhaled nanoparticles: role of in vivo, ex vivo, in vitro, and in silico studies. Int. J. Mol. Sci. 15:4795–4822, 2014. https://doi.org/10.3390/ijms15034795.
Rodrigues, R. O., P. C. Sousa, J. Gaspar, M. Bañobre-López, R. Lima, and G. Minas. Organ-on-a-chip: a preclinical microfluidic platform for the progress of nanomedicine. Small. 2020. https://doi.org/10.1002/smll.202003517.
Lodi Rizzini, M., D. Gallo, G. De Nisco, F. D’Ascenzo, C. Chiastra, P. P. Bocchino, F. Piroli, G. M. De Ferrari, and U. Morbiducci. Does the inflow velocity profile influence physiologically relevant flow patterns in computational hemodynamic models of left anterior descending coronary artery? Med. Eng. Phys. 82:58–69, 2020. https://doi.org/10.1016/j.medengphy.2020.07.001.
Pedley, T. J., and Y. C. Fung. The fluid mechanics of large blood vessels. J. Biomech. Eng. 102:345–346, 1980. https://doi.org/10.1115/1.3138235.
Berger, S. A., and L.-D. Jou. Flows in stenotic vessels. Annu. Rev. Fluid Mech. 32:347–382, 2000. https://doi.org/10.1146/annurev.fluid.32.1.347.
Quarteroni, A., M. Tuveri, and A. Veneziani. Computational vascular fluid dynamics: problems, models and methods. Comput. Vis. Sci. 2:163–197, 2000. https://doi.org/10.1007/s007910050039.
Fung, Y. C. Biomechanics: Circulation. Springer, New York, 2013.
Perktold, K., M. Resch, and H. Florian. Pulsatile non-Newtonian flow characteristics in a three-dimensional human carotid bifurcation model. J. Biomech. Eng. 113:464–475, 1991. https://doi.org/10.1115/1.2895428.
Rodkiewicz, C. M., P. Sinha, and J. S. Kennedy. On the application of a constitutive equation for whole human blood. J. Biomech. Eng. 112:198–206, 1990. https://doi.org/10.1115/1.2891172.
Tu, C., and M. Deville. Pulsatile flow of non-Newtonian fluids through arterial stenoses. J. Biomech. 29:899–908, 1996. https://doi.org/10.1016/0021-9290(95)00151-4.
Gijsen, F. J. H., E. Allanic, F. N. van de Vosse, and J. D. Janssen. The influence of the non-Newtonian properties of blood on the flow in large arteries: unsteady flow in a \(90^{\circ }\) curved tube. J. Biomech. 32:705–713, 1999. https://doi.org/10.1016/s0021-9290(99)00014-7.
Perktold, K., R. Peter, and M. Resch. Pulsatile non-Newtonian blood flow simulation through a bifurcation with an aneurysm. Biorheology. 26:1011–1030, 1989. https://doi.org/10.3233/bir-1989-26605.
Ballyk, P. D., D. A. Steinman, and C. R. Ethier. Simulation of non-Newtonian blood flow in an end-to-side anastomosis. Biorheology. 31:565–586, 1994. https://doi.org/10.3233/bir-1994-31505.
Chaichana, T., Z. Sun, and J. Jewkes. Computational fluid dynamics analysis of the effect of plaques in the left coronary artery. Comput. Math. Methods Med. 2012. https://doi.org/10.1155/2012/504367.
Cebral, J. R., M. A. Castro, S. Appanaboyina, C. M. Putman, D. Millan, and A. F. Frangi. Efficient pipeline for image-based patient-specific analysis of cerebral aneurysm hemodynamics: technique and sensitivity. IEEE Trans. Med. Imaging. 24:457–467, 2005. https://doi.org/10.1109/tmi.2005.844159.
Soares, A. A., S. Gonzaga, C. Oliveira, A. Simões, and A. I. Rouboa. Computational fluid dynamics in abdominal aorta bifurcation: non-Newtonian versus Newtonian blood flow in a real case study. Comput. Methods Biomech. Biomed. 20:822–831, 2017. https://doi.org/10.1080/10255842.2017.1302433.
Liu, X., Y. Fan, X. Deng, and F. Zhan. Effect of non-Newtonian and pulsatile blood flow on mass transport in the human aorta. J. Biomech. 44:1123–1131, 2011. https://doi.org/10.1016/j.jbiomech.2011.01.024.
Lou, Z., and W.-J. Yang. A computer simulation of the non-Newtonian blood flow at the aortic bifurcation. J. Biomech. 26:37–49, 1993. https://doi.org/10.1016/0021-9290(93)90611-h.
Chen, J., X.-Y. Lu, and W. Wang. Non-Newtonian effects of blood flow on hemodynamics in distal vascular graft anastomoses. J. Biomech. 39:1983–1995, 2006. https://doi.org/10.1016/j.jbiomech.2005.06.012.
Gaudio, L. T., M. V. Caruso, S. De Rosa, C. Indolfi, and G. Fragomeni. Different blood flow models in coronary artery diseases: effects on hemodynamic parameters. 40th Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. (EMBC). IEEE 2018.
Carvalho, V., N. Rodrigues, R. A. Lima, and S. Teixeira. Modeling blood pulsatile turbulent flow in stenotic coronary arteries. Int. J. Biol. Biomed. Eng. 14:1998–4510, 2020.
Cho, Y. I., and K. R. Kensey. Effects of the non-Newtonian viscosity of blood on flows in a diseased arterial vessel. Part 1: steady flows. Biorheology. 28:241–262, 1991. https://doi.org/10.3233/bir-1991-283-415.
Ternik, P. Symmetry breaking phenomena of purely viscous shear-thinning fluid flow in a locally constricted channel. Int. J. Simul. Model. 7:186–197, 2008. https://doi.org/10.2507/ijsimm07(4)3.107.
Fung, Y.C. Biomechanics: Mechanical Properties of Living Tissues. Springer, New York, 2013.
Mendieta, J. B., D. Fontanarosa, J. Wang, P. K. Paritala, T. McGahan, T. Lloyd, and Z. Li. The importance of blood rheology in patient-specific computational fluid dynamics simulation of stenotic carotid arteries. Biomech. Model. Mechanobiol. 19:1477–1490, 2020. https://doi.org/10.1007/s10237-019-01282-7.
Šeta, B., M. Torlak, and A. Vila. Numerical simulation of blood flow through the aortic arch. CMBEBIH 2017: Proceedings International Conference Medical & Biological Engineering. Springer, Singapore, 2017.
Xu, L., T. Yang, L. Yin, Y. Kong, Y. Vassilevski, and F. Liang. Numerical simulation of blood flow in aorta with dilation: a comparisonbetween laminar and LES modeling methods. Comput. Model. Eng. Sci. 124:509–526, 2020. https://doi.org/10.32604/cmes.2020.010719.
Andersson, M., T. Ebbers, and M. Karlsson. Characterization and estimation of turbulence-related wall shear stress in patient-specific pulsatile blood flow. J. Biomech. 85:108–117, 2019. https://doi.org/10.1016/j.jbiomech.2019.01.016.
Li, C., J. Jiang, H. Dong, and K. Zhao. Computational modeling and validation of human nasal airflow under various breathing conditions. J. Biomech. 64:59–68, 2017. https://doi.org/10.1016/j.jbiomech.2017.08.031.
Molla, M. M., and M. C. Paul. LES of non-Newtonian physiological blood flow in a model of arterial stenosis. Med. Eng. Phys. 34:1079–1087, 2012. https://doi.org/10.1016/j.medengphy.2011.11.013.
Mittal, R., S. P. Simmons, and F. Najjar. Numerical study of pulsatile flow in a constricted channel. J. Fluid Mech. 485:337–378, 2003. https://doi.org/10.1017/s002211200300449x.
Zhu, C., J.-H. Seo, and R. Mittal. Computational modelling and analysis of haemodynamics in a simple model of aortic stenosis. J. Fluid Mech. 851:23–49, 2018. https://doi.org/10.1017/jfm.2018.463.
Dobroserdova, T., F. Liang, G. Panasenko, and Y. Vassilevski. Multiscale models of blood flow in the compliant aortic bifurcation. Appl. Math. Lett. 93:98–104, 2019. https://doi.org/10.1016/j.aml.2019.01.037.
Liang, F., S. Takagi, R. Himeno, and H. Liu. Multi-scale modeling of the human cardiovascular system with applications to aortic valvular and arterial stenoses. Med. Biol. Eng. Comput. 47:743–755, 2009. https://doi.org/10.1007/s11517-009-0449-9.
Alimohammadi, M., J. M. Sherwood, Karimpour M. Agu, O. Balabani, S. Díaz-Zuccarini, and V. Aortic dissection simulation models for clinical support: fluid-structure interaction vs. rigid wall models. Biomed. Eng. Online. 14, 2015. https://doi.org/10.1186/s12938-015-0032-6.
Bonfanti, M., S. Balabani, M. Alimohammadi, O. Agu, S. Homer-Vanniasinkam, and V. Díaz-Zuccarini. A simplified method to account for wall motion in patient-specific blood flow simulations of aortic dissection: comparison with fluid-structure interaction. Med. Eng. Phys. 58:72–79, 2018. https://doi.org/10.1016/j.medengphy.2018.04.014.
Alishahi, M., M. M. Alishahi, and H. Emdad. Numerical simulation of blood flow in a flexible stenosed abdominal real aorta. Sci. Iran. 18:1297–1305, 2011. https://doi.org/10.1016/j.scient.2011.11.021.
Xiong, G., C. A. Figueroa, N. Xiao, and C. A. Taylor. Simulation of blood flow in deformable vessels using subject-specific geometry and spatially varying wall properties. Int. J. Numer. Methods Biomed. Eng. 27:1000–1016, 2010. https://doi.org/10.1002/cnm.1404.
Lopes, D., H. Puga, J. C. Teixeira, and S. F. Teixeira. Fluid-structure Interaction study of carotid blood flow: comparison between viscosity models. Eur. J. Mech. - B/Fluids. 83:226–234, 2020. https://doi.org/10.1016/j.euromechflu.2020.05.010.
Saeedi, M., A. Shamloo, and A. Mohammadi. Fluid-structure interaction simulation of blood flow and cerebral aneurysm: effect of partly blocked vessel. J. Vasc. Res. 56:296–307, 2019. https://doi.org/10.1159/000503786.
Zhao, Y., J. Ping, X. Yu, R. Wu, C. Sun, and M. Zhang. Fractional flow reserve-based 4D hemodynamic simulation of time-resolved blood flow in left anterior descending coronary artery. Clin. Biomech. 70:164–169, 2019. https://doi.org/10.1016/j.clinbiomech.2019.09.003.
Torii, R., N. B. Wood, N. Hadjiloizou, A. W. Dowsey, A. R. Wright, A. D. Hughes, J. Davies, D. P. Francis, J. Mayet, G.-Z. Yang, S. AMc. G. Thom, and X. Y. Xu. Fluid-structure interaction analysis of a patient-specific right coronary artery with physiological velocity and pressure waveforms. Commun. numer. methods eng. 25:565–580, 2009. https://doi.org/10.1002/cnm.1231.
Thomas, B., and K. S. Sumam. Blood flow in human arterial system—a review. Proc. Technol. 24:339–346, 2016. https://doi.org/10.1016/j.protcy.2016.05.045.
Long, Q., X. Y. Xu, M. Bourne, and T. M. Griffith. Numerical study of blood flow in an anatomically realistic aorto-iliac bifurcation generated from MRI data. Magn. Reson. Med. 43:565–576, 2000. https://doi.org/10.1002/(sici)1522-2594(200004)43:4<565::aid-mrm11>3.0.co;2-l.
Oshima, M., R. Torii, T. Kobayashi, N. Taniguchi, and K. Takagi. Finite element simulation of blood flow in the cerebral artery. Comput. Methods Appl. Mech. Eng. 191:661–671, 2001. https://doi.org/10.1016/s0045-7825(01)00307-3.
Morris, L., P. Delassus, A. Callanan, M. Walsh, F. Wallis, P. Grace, and T. McGloughlin. 3-D numerical simulation of blood flow through models of the human Aorta. J. Biomech. Eng. 127:767–775, 2005. https://doi.org/10.1115/1.1992521.
Kim, H. J., I. E. Vignon-Clementel, C. A. Figueroa, K. E. Jansen, and C. A. Taylor. Developing computational methods for three-dimensional finite element simulations of coronary blood flow. Finite Elem. Anal. Des. 46:514–525, 2010. https://doi.org/10.1016/j.finel.2010.01.007.
Lee, S. H., H. G. Choi, and J. Y. Yool. Finite element simulation of blood flow in a flexible carotid artery bifurcation. J. Mech. Sci. Technol. 26:1355–1361, 2012. https://doi.org/10.1007/s12206-012-0331-9.
Suito, H., T. Ueda, and D. Sze. Numerical simulation of blood flow in the thoracic aorta using a centerline-fitted finite difference approach. Jpn. J. Ind. Appl. Math. 30:701–710, 2013. https://doi.org/10.1007/s13160-013-0123-3.
Mulani, S. S., and P. I. Jagad. Analysis of the effects of plaque deposits on the blood flow through human artery. Int. Eng. Res. 41:2319–3182, 2015.
Boghi, A., and F. Gori. Numerical simulation of blood flow through different stents in stenosed and non-stenosed vessels. Numer. Heat Transf.; A: Appl. 68:225–242, 2015. https://doi.org/10.1080/10407782.2014.977151.
Jabir, E., and S. A. Lal. Numerical analysis of blood flow through an elliptic stenosis using large eddy simulation. Proc. Inst. Mech. Eng. H P I MECH. ENG. H. 230:709–726, 2016. https://doi.org/10.1177/0954411916644474.
Oliveira, C., A. A. Soares, A. Simões, S. Gonzaga, and A. Rouboa. Numerical study of non-Newtonian blood behavior in the abdominal aortic bifurcation of a patient-specific at rest. Open Sports Sci. J. 10:279–285, 2017. https://doi.org/10.2174/1875399x01710010279.
Abbas, S. S., M. S. Nasif, M. A. M. Said, and R. Al-Waked. Numerical simulation of the non-Newtonian blood flow through aortic Bileaflet mechanical heart valve using fluid-structure interaction approach. AIP Conf. Proc. 2018. https://doi.org/10.1063/1.5075593.
Kaewbumrung, M., S. Orankitjaroen, P. Boonkrong, B. Nuntadilok, and B. Wiwatanapataphee. Numerical simulation of dispersed particle-blood flow in the stenosed coronary arteries: Int. J. Differ. Equ. 2018. https://doi.org/10.1155/2018/2593425.
Kabir, M. A., M. F. Alam, and M. A. Uddin. A numerical study on the effects of reynolds number on blood flow with spiral velocity through regular arterial stenosis. Chiang Mai J. Sci. 45:2515–2527, 2018.
Malota, Z., J. Glowacki, W. Sadowski, and M. Kostur. Numerical analysis of the impact of flow rate, heart rate, vessel geometry, and degree of stenosis on coronary hemodynamic indices. BMC Cardiovasc. Disord. 2018. https://doi.org/10.1186/s12872-018-0865-6.
Elhanafy, A., A. Guaily, and A. Elsaid. Numerical simulation of blood flow in abdominal aortic aneurysms: effects of blood shear-thinning and viscoelastic properties. Math. Comput. Simul. 160:55–71, 2019. https://doi.org/10.1016/j.matcom.2018.12.002.
Selmi, M., H. Belmabrouk, and A. Bajahzar. Numerical study of the blood flow in a deformable human aorta. Appl. Sci. 2019. https://doi.org/10.3390/app9061216.
Lo, E., L. Menezes, and R. Torii. Impact of inflow boundary conditions on the calculation of CT-based FFR. Fluids. 2019. https://doi.org/10.3390/fluids4020060.
Jahromi, R., H. A. Pakravan, M. S. Saidi, and B. Firoozabadi. Primary stenosis progression versus secondary stenosis formation in the left coronary bifurcation: a mechanical point of view. Biocybern. Biomed. Eng. 39:188–198, 2019. https://doi.org/10.1016/j.bbe.2018.11.006.
Yan, S.-R., S. Sedeh, D. Toghraie, M. Afrand, and L. K. Foong. Analysis and manegement of laminar blood flow inside a cerebral blood vessel using a finite volume software program for biomedical engineering. Comput. Methods Programs Biomed. 2020. https://doi.org/10.1016/j.cmpb.2020.105384.
Kashyap, V., B. B. Arora, and S. Bhattacharjee. A computational study of branch-wise curvature in idealized coronary artery bifurcations. Appl. Eng. Sci. 2020. https://doi.org/10.1016/j.apples.2020.100027.
Gabbanelli, S., G. Drazer, and J. Koplik. Lattice Boltzmann method for non-Newtonian (power-law) fluids. Phys. Rev. E. 2005. https://doi.org/10.1103/physreve.72.046312.
Velivelli, A. C., and K. M. Bryden. Parallel performance and accuracy of lattice Boltzmann and traditional finite difference methods for solving the unsteady two-dimensional Burger’s equation. Physics A 362:139–145, 2006. https://doi.org/10.1016/j.physa.2005.09.031.
Fang, H., Z. Wang, Z. Lin, and M. Liu. Lattice Boltzmann method for simulating the viscous flow in large distensible blood vessels. Phys. Rev. E. 2002. https://doi.org/10.1103/physreve.65.051925.
Tamagawa, M., H. Kaneda, M. Hiramoto, and S. Nagahama. Simulation of thrombus formation in shear flows using lattice Boltzmann method. Artif. Organs. 33:604–610, 2009. https://doi.org/10.1111/j.1525-1594.2009.00782.x.
Artoli, A. M., D. Kandhai, H. C. J. Hoefsloot, A. G. Hoekstra, and P. M. A. Sloot. Lattice BGK simulations of flow in a symmetric bifurcation. Future Gener. Comput. Syst. 20:909–916, 2004. https://doi.org/10.1016/j.future.2003.12.002.
Boyd, J., J. Buick, J. A. Cosgrove, and P. Stansell. Application of the lattice Boltzmann model to simulated stenosis growth in a two-dimensional carotid artery. Phys. Med. Biol. 50:4783–4796, 2005. https://doi.org/10.1088/0031-9155/50/20/003.
Boyd, J., J. Buick, and S. Green. A second-order accurate lattice Boltzmann non-Newtonian flow model. J. Phys. A Math. Gen. 39:14241–14247, 2006. https://doi.org/10.1088/0305-4470/39/46/001.
Boyd, J., J. M. Buick, and S. Green. Analysis of the Casson and Carreau-Yasuda non-Newtonian blood models in steady and oscillatory flows using the lattice Boltzmann method. Phys. Fluids. 2007. https://doi.org/10.1063/1.2772250.
Bernsdorf, J., and D. Wang. Non-Newtonian blood flow simulation in cerebral aneurysms. Comput. Math. with Appl. 58:1024–1029, 2009. https://doi.org/10.1016/j.camwa.2009.02.019.
Ashrafizaadeh, M., and H. Bakhshaei. A comparison of non-Newtonian models for lattice Boltzmann blood flow simulations. Comput. Math. with Appl. 58:1045–1054, 2009. https://doi.org/10.1016/j.camwa.2009.02.021.
Chopard, B., D. Lagrava, O. Malaspinas, R. Ouared, J. Latt, K. O. Lovblad, and V. Pereira-Mendes. A lattice Boltzmann modeling of bloodflow in cerebral aneurysms. V. Eur. Conf. Comput. Fluid Dyn. ECCOMAS CFD 2010.
Cherkaoui, I., S. Bettaibi, A. Barkaoui, and F. Kuznik. Magnetohydrodynamic blood flow study in stenotic coronary artery using lattice Boltzmann method. Comput. Methods Programs Biomed. 2022. https://doi.org/10.1016/j.cmpb.2022.106850.
Cherkaoui, I., S. Bettaibi, and A. Barkaoui. Double population lattice Boltzmann model for magneto-hydrodynamic blood flow in stenotic artery. Cellular automata: 15th International Conference on Cellular Automata for Research and Industry, ACRI 2022, Geneva, Switzerland, September 12–15, 2022, Proceedings. Springer International Publishing, Cham, 2022.
Shahzad, H., X. Wang, I. Sarris, K. Iqbal, M. B. Hafeez, and M. Krawczuk. Study of Non-Newtonian biomagnetic blood flow in a stenosed bifurcated artery having elastic walls. Sci. Rep. 2021. https://doi.org/10.1038/s41598-021-03426-1.
Anwar, M. A., K. Iqbal, and M. Razzaq. Analysis of biomagnetic blood flow in a stenosed bifurcation artery amidst elastic walls. Phys. Scr. 2021. https://doi.org/10.1088/1402-4896/abf67b.
Misra, J. C., A. Sinha, and G. C. Shit. Flow of a biomagnetic viscoelastic fluid: application to estimation of blood flow in arteries during electromagnetic hyperthermia, a therapeutic procedure for cancer treatment. Appl. Math. Mech. 31:1405–1420, 2010. https://doi.org/10.1007/s10483-010-1371-6.
Tzirtzilakis, E. E. Biomagnetic fluid flow in a channel with stenosis. Physics D 237:66–81, 2008. https://doi.org/10.1016/j.physd.2007.08.006.
Akar, S., J. A. Esfahani, and S. A. Mousavi Shaegh. A numerical investigation of magnetic field effect on blood flow as biomagnetic fluid in a bend vessel. J. Magn. Magn. Mater. 482:336–349, 2019. https://doi.org/10.1016/j.jmmm.2019.03.043.
Tenforde, T. S. Magnetically induced electric fields and currents in the circulatory system. Prog. Biophys. Mol. Biol. 87:279–288, 2005. https://doi.org/10.1016/j.pbiomolbio.2004.08.003.
Higashi, T., A. Yamagishi, T. Takeuchi, N. Kawaguchi, S. Sagawa, S. Onishi, and M. Date. Orientation of erythrocytes in a strong static magnetic field. Blood. 82:1328–1334, 1993. https://doi.org/10.1182/blood.v82.4.1328.bloodjournal8241328.
Haik, Y., V. Pai, and C.-J. Chen. Apparent viscosity of human blood in a high static magnetic field. J. Magn. Magn. Mater. 225:180–186, 2001. https://doi.org/10.1016/s0304-8853(00)01249-x.
Korchevskii, E. M., and L. S. Marochnik. Magnetohydrodynamic version of movement of blood. Biophysics. 10(2):411–414, 1965.
Gold, R. R. Magnetohydrodynamic pipe flow. Part 1. J. Fluid Mech. 13:505–512, 1962. https://doi.org/10.1017/s0022112062000889.
Sud, V. K., P. K. Suri, and R. K. Mishra. Effect of magnetic field on oscillating blood flow in arteries. Stud. Biophys. 46(3):163–171, 1974.
Abi-Abdallah, D., V. Robin, O. Fokapu, and A. Drochon. Pulsed magnetohydrodynamic blood flow in a rigid vessel. Comput. Methods Biomech. Biomed. 10:159–160, 2007. https://doi.org/10.1080/10255840701479636.
Shit, G. C., and M. Roy. Pulsatile flow and heat transfer of a magneto-micropolar fluid through a stenosed artery under the influence of body acceleration. J. Mech. Med. Biol. 11:643–661, 2011.
Loukopoulos, V. C., and E. E. Tzirtzilakis. Biomagnetic channel flow in spatially varying magnetic field. Int. J. Eng. Sci. 42:571–590, 2004.
Kenjereš, S. Numerical analysis of blood flow in realistic arteries subjected to strong non-uniform magnetic fields. Int. J. Heat Fluid Flow. 29:752–764, 2008.
Ikbal, M. A., S. Chakravarty, K. L. Wong, J. Mazumdar, and P. K. Mandal. Unsteady response of non-Newtonian blood flow through a stenosed artery in magnetic field. J. Comput. Appl. Math. 230:243–259, 2009.
Mustapha, N., N. Amin, M. Chakravarty, and P. K. Mandal. Unsteady magnetohydrodynamic blood flow through irregular multi-stenosed arteries. Comput. Biol. Med. 39:896–906, 2009.
Türk, Ö., C. Bozkaya, and M. Tezer-Sezgin. A FEM approach to biomagnetic fluid flow in multiple stenosed channels. Comput. Fluids. 97:40–51, 2014.
Shit, G. C., and S. Majee. Magnetic field interaction with blood flow and heat transfer through diseased artery having Abdominal Aortic Aneurysm. Eur. J. Mech. B/Fluids. 71:1–14, 2018. https://doi.org/10.1016/j.euromechflu.2018.03.010.
Tzirtzilakis, E. E. Biomagnetic fluid flow in an aneurysm using ferrohydrodynamics principles. Phys. Fluids.27:061902, 2015. https://doi.org/10.1063/1.4922757.
Sharifi, A., S. Yekani Motlagh, and H. Badfar. Investigation of the effects of two parallel wires’ non-uniform magnetic field on heat and biomagnetic fluid flow in an aneurysm. Int. J. Comput. Fluid Dyn. 32:248–259, 2018. https://doi.org/10.1080/10618562.2018.1490413.
Javadzadegan, A., A. Moshfegh, H. H. Afrouzi, and M. Omidi. Magnetohydrodynamic blood flow in patients with coronary artery disease. Comput. Methods Programs Biomed. 163:111–122, 2018. https://doi.org/10.1016/j.cmpb.2018.06.007.
Chi, Q., X. Li, S. Chang, L. Mu, Y. He, and H. Gao. In-vitro experimental study on the fluid-structure interaction in an image-based flexible model with a lateral cerebral aneurysm. Med. Novel Technol. Devices. 2019. https://doi.org/10.1016/j.medntd.2019.100019.
Shit, G. C., and S. Majee. Pulsatile flow of blood and heat transfer with variable viscosity under magnetic and vibration environment. J. Magn. Magn. Mater. 388:106–115, 2015.
Bandyopadhyay, S., and G. C. Layek. Study of Magnetohydrodynamic pulsatile flow in a constricted channel. Commun. Nonlinear Sci. Numer. 17:2434–2446, 2012.
Alimohamadi, H., and M. Imani. Transient non-Newtonian blood flow under magnetic targeting drug delivery in an aneurysm blood vessel with porous walls. Int. J. Comput. Methods Eng. Sci. Mech. 2014.
Sadeghi, M. R., M. Jahangiri, and M. Saghafian. The impact of uniform magnetic field on the pulsatile non-Newtonian blood flow in an elastic stenosed artery. J. Braz. Soc. Mech. Sci. Eng. 2020. https://doi.org/10.1007/s40430-020-02651-5.
Teimouri, K., M. R. Tavakoli, A. Ghafari, and K. C. Kim. Investigation of the plaque morphology effect on changes of pulsatile blood flow in a stenosed curved artery induced by an external magnetic field. Comput. Biol. Med. 2021. https://doi.org/10.1016/j.compbiomed.2021.104600.
Ali, A., M. Umar, Z. Abbas, G. Shahzadi, Z. Bukhari, and A. Saleem. Numerical Investigation of MHD pulsatile flow of micropolar fluid in a channel with symmetrically constricted walls. Mathematics. 2021. https://doi.org/10.3390/math9091000.
Aharonov, E., and D. H. Rothman. Non-Newtonian flow (through porous media): a lattice-Boltzmann method. Geophys. Res. Lett. 20:679–682, 1993. https://doi.org/10.1029/93gl00473.
Yoshino, M., Y. Hotta, T. Hirozane, and M. Endo. A numerical method for incompressible non-Newtonian fluid flows based on the lattice Boltzmann method. J. Non-Newton. Fluid Mech. 147:69–78, 2007. https://doi.org/10.1016/j.jnnfm.2007.07.007.
Vikhansky, A. Lattice-Boltzmann method for yield-stress liquids. J. Non-Newton. Fluid Mech. 155:95–100, 2008. https://doi.org/10.1016/j.jnnfm.2007.09.001.
Stahl, B., B. Chopard, and J. Latt. Measurements of wall shear stress with the lattice Boltzmann method and staircase approximation of boundaries. Comput. Fluids. 39:1625–1633, 2010. https://doi.org/10.1016/j.compfluid.2010.05.015.
Maier, R. S., R. S. Bernard, and D. W. Grunau. Boundary conditions for the lattice Boltzmann method. Phys. Fluids. 8:1788–1801, 1996. https://doi.org/10.1063/1.868961.
Noble, D. R., S. Chen, J. G. Georgiadis, and R. O. Buckius. A consistent hydrodynamic boundary condition for the lattice Boltzmann method. Phys. Fluids. 7:203–209, 1995. https://doi.org/10.1063/1.868767.
Inamuro, T., M. Yoshino, and F. Ogino. A non-slip boundary condition for lattice Boltzmann simulations. Phys. Fluids. 7:2928–2930, 1995. https://doi.org/10.1063/1.868766.
Chen, S., D. Martínez, and R. Mei. On boundary conditions in lattice Boltzmann methods. Phys. Fluids. 8:2527–2536, 1996. https://doi.org/10.1063/1.869035.
Filippova, O., and D. Hänel. Grid refinement for lattice-BGK models. J. Comput. Phys. 147:219–228, 1998. https://doi.org/10.1006/jcph.1998.6089.
Mei, R., L.-S. Luo, and W. Shyy. An accurate curved boundary treatment in the lattice Boltzmann method. J. Comput. Phys. 155:307–330, 1999. https://doi.org/10.1006/jcph.1999.6334.
Yu, D., R. Mei, W. Shyy. A unified boundary treatment in lattice Boltzmann method. 41st Aerosp. Sci. Meet. Exhib. 2003. https://doi.org/10.2514/6.2003-953.
Succi, S. The lattice Boltzmann equation for fluid dynamics and beyond. 2001. https://doi.org/10.1604/9780198503989.
Banerjee, M. K., R. Ganguly, and A. Datta. Effect of pulsatile flow waveform and womersley number on the flow in stenosed arterial geometry. ISRN Biomath. 2012. https://doi.org/10.5402/2012/853056.
Cherkaoui, I., S. Bettaibi, A. Barkaoui, and F. Kuznik. Numerical study of pulsatile thermal magnetohydrodynamic blood flow in an artery with aneurysm using Lattice Boltzmann Method. Commun. Nonlinear Sci. Numer. Simul. 2023. https://doi.org/10.1016/j.cnsns.2023.107281.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Associate Editor Stefan M. Duma oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cherkaoui, I., Bettaibi, S., Barkaoui, A. et al. Toward a Mesoscopic Modeling Approach of Magnetohydrodynamic Blood Flow in Pathological Vessels: A Comprehensive Review. Ann Biomed Eng 51, 2415–2440 (2023). https://doi.org/10.1007/s10439-023-03350-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-023-03350-7