Abstract
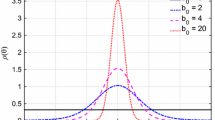
Pulse wave velocity (PWV) is a key, independent risk factor for future cardiovascular events. The Moens–Korteweg equation describes the relation between PWV and the stiffness of arterial tissue with an assumption of isotopic linear elastic property of the arterial wall. However, the arterial tissue exhibits highly nonlinear and anisotropic mechanical behaviors. There is a limited study regarding the effect of arterial nonlinear and anisotropic properties on the PWV. In this study, we investigated the impact of the arterial nonlinear hyperelastic properties on the PWV, based on our recently developed unified-fiber-distribution (UFD) model. The UFD model considers the fibers (embedded in the matrix of the tissue) as a unified distribution, which expects to be more physically consistent with the real fiber distribution than existing models that separate the fiber distribution into two/several fiber families. With the UFD model, we fitted the measured relation between the PWV and blood pressure which obtained a good accuracy. We also modeled the aging effect on the PWV based on observations that the stiffening of arterial tissue increases with aging, and the results agree well with experimental data. In addition, we did parameter studies on the dependence of the PWV on the arterial properties of fiber initial stiffness, fiber distribution, and matrix stiffness. The results indicate the PWV increases with increasing overall fiber component in the circumferential direction. The dependences of the PWV on the fiber initial stiffness, and matrix stiffness are not monotonic and change with different blood pressure. The results of this study could provide new insights into arterial property changes and disease information from the clinical measured PWV data.








Similar content being viewed by others
References
Nabeel, P., V. R. Kiran, J. Joseph, V. Abhidev, and M. Sivaprakasam. Local pulse wave velocity: Theory, methods, advancements, and clinical applications. IEEE Rev. Biomed. Eng. 13:74–112, 2019.
Mancia, G., R. Fagard, K. Narkiewicz, J. Redán, A. Zanchetti, M. Böhm, T. Christiaens, R. Cifkova, G. De Backer, and A. Dominiczak. 2013 Practice guidelines for the management of arterial hypertension of the European Society of Hypertension (ESH) and the European Society of Cardiology (ESC): ESH/ESC Task Force for the Management of Arterial Hypertension. J. Hypertension. 31(10):1925–1938, 2013.
Vlachopoulos, C., K. Aznaouridis, and C. Stefanadis. Prediction of cardiovascular events and all-cause mortality with arterial stiffness: A systematic review and meta-analysis. J. Am. College Cardiol. 55(13):1318–1327, 2010.
Yamashina, A., H. Tomiyama, T. Arai, K.-I. Hirose, Y. Koji, Y. Hirayama, Y. Yamamoto, and S. Hori. Brachial-ankle pulse wave velocity as a marker of atherosclerotic vascular damage and cardiovascular risk. Hypertension Res. 26(8):615–622, 2003.
Fung, Y.-C. Biomechanics: Circulation. New York: Springer, 2013.
Martin, C., W. Sun, T. Pham, and J. Elefteriades. Predictive biomechanical analysis of ascending aortic aneurysm rupture potential. Acta biomaterialia. 9(12):9392–9400, 2013.
Pham, T., C. Martin, J. Elefteriades, and W. Sun. Biomechanical characterization of ascending aortic aneurysm with concomitant bicuspid aortic valve and bovine aortic arch. Acta Biomater. 9(8):7927–7936, 2013.
Martin, C., W. Sun, and J. Elefteriades. Patient-specific finite element analysis of ascending aorta aneurysms. Am. J. Physiol.-Heart Circ. Physiol. 308(10):H1306–H1316, 2015.
Liu, M., H. Dong, X. Lou, G. Iannucci, E. P. Chen, B. G. Leshnower, and W. Sun. A novel anisotropic failure criterion with dispersed fiber orientations for aortic tissues. J. Biomech. Eng.142(11):111002, 2020.
Dong, H., M. Liu, X. Lou, B. G. Leshnower, W. Sun, B. A. Ziganshin, M. A. Zafar, and J. A. Elefteriades. Ultimate tensile strength and biaxial stress–strain responses of aortic tissues—A clinical-engineering correlation. Appl. Eng. Sci.10:100101, 2022.
Iliopoulos, D. C., R. P. Deveja, E. P. Kritharis, D. Perrea, G. D. Sionis, K. Toutouzas, C. Stefanadis, and D. P. Sokolis. Regional and directional variations in the mechanical properties of ascending thoracic aortic aneurysms. Med. Eng. Phys. 31(1):1–9, 2009.
Sokolis, D. P. Layer-specific tensile strength of the human aorta: segmental variations. J. Biomech. Eng.145(6):064502, 2023.
Horný, L., and J. Kužma. Pressure pulse wave velocity and axial prestretch in arteries. World Congr. Med. Phys. Biomed. Eng. 2019:665–669, 2018.
Ma, Y., J. Choi, A. Hourlier-Fargette, Y. Xue, H. U. Chung, J. Y. Lee, X. Wang, Z. Xie, D. Kang, and H. Wang. Relation between blood pressure and pulse wave velocity for human arteries. Proc. Natl. Acad. Sci. 115(44):11144–11149, 2018.
Ferruzzi, J., D. Madziva, A. Caulk, G. Tellides, and J. Humphrey. Compromised mechanical homeostasis in arterial aging and associated cardiovascular consequences. Biomech. Model Mechanobiol. 17(5):1281–1295, 2018.
O’rourke, M. F., and J. Hashimoto. Mechanical factors in arterial aging: a clinical perspective. J. Am. College Cardiol. 50(1):1–13, 2007.
Holzapfel, G. A., T. C. Gasser, and R. W. Ogden. A new constitutive framework for arterial wall mechanics and a comparative study of material models. J. Elast. Phys. Sci. Solids. 61(1):1–48, 2000.
Pejcic, S., S. M. A. Hassan, D. E. Rival, and G. Bisleri. Characterizing the Mechanical Properties of the Aortic Wall. Vessel Plus: Alhambra, 2019.
Liu, M., L. Liang, Y. Ismail, H. Dong, X. Lou, G. Iannucci, E. P. Chen, B. G. Leshnower, J. A. Elefteriades, and W. Sun. Computation of a probabilistic and anisotropic failure metric on the aortic wall using a machine learning-based surrogate model. Comput. Biol. Med. 137:104794, 2021.
Puck, A., and H. Schürmann. Failure Analysis of FRP Laminates by Means of Physically Based Phenomenological Models, Failure Criteria in Fibre-Reinforced-Polymer Composites. Amsterdam: Elsevier, pp. 832–876, 2004.
Dong, H., J. Wang, and B. Karihaloo. An improved Puck’s failure theory for fibre-reinforced composite laminates including the in situ strength effect. Compos. Sci. Technol. 98:86–92, 2014.
Dong, H., and J. Wang. A criterion for failure mode prediction of angle-ply composite laminates under in-plane tension. Composite Struct. 128:234–240, 2015.
Dong, H., Z. Li, J. Wang, and B. Karihaloo. A new fatigue failure theory for multidirectional fiber-reinforced composite laminates with arbitrary stacking sequence. Int. J. Fatigue. 87:294–300, 2016.
Häsä, R., and S. Pinho. Failure mechanisms of biological crossed-lamellar microstructures applied to synthetic high-performance fibre-reinforced composites. J. Mech. Phys. Solids. 125:53–73, 2019.
Li, S., and Z. Ma. Strength analysis of multidirectional fiber-reinforced composite laminates with uncertainty in macromechanical properties. Phys. Mesomech. 24(3):311–318, 2021.
Li, S., Z. Ma, and Q. Yang. Progressive failure analysis of composite laminates subjected to transverse loading with augmented finite element method. Int. J. Appl. Mech. 14(4):2250038, 2022.
Li, S., and J. Wang. The stress intensity factor and propagation of an inclined crack in the central layer of a composite laminate under tension. Theor. Appl. Fract. Mech. 93:128–136, 2018.
Schriefl, A. J., G. Zeindlinger, D. M. Pierce, P. Regitnig, and G. A. Holzapfel. Determination of the layer-specific distributed collagen fibre orientations in human thoracic and abdominal aortas and common iliac arteries. J. R. Soc. Interface. 9(71):1275–1286, 2012.
Gasser, T. C., R. W. Ogden, and G. A. Holzapfel. Hyperelastic modelling of arterial layers with distributed collagen fibre orientations. J. R. Soc. Interface. 3(6):15–35, 2006.
Dong, H., and W. Sun. A novel hyperelastic model for biological tissues with planar distributed fibers and a second kind of Poisson effect. J. Mech. Phys. Solids.151:104377, 2021.
Dong, H., M. Liu, T. Qin, L. Liang, B. Ziganshin, H. Ellauzi, M. Zafar, S. Jang, J. Elefteriades, W. Sun, and R. L. Gleason. A novel computational growth framework for biological tissues: Application to growth of aortic root aneurysm repaired by the V-shape surgery. J. Mech. Behav. Biomed. Mater.127:105081, 2022.
Liu, M., L. Liang, H. Dong, W. Sun, and R. L. Gleason. Constructing growth evolution laws of arteries via reinforcement learning. J. Mech. Phys. Solids.168:105044, 2022.
Omojola, V. O., Z. Hardnett, H. Song, H. Dong, D. J. Alexander, A. O. A. Michael, R. L. Gleason Jr., and M. O. Platt. Comparative analysis of arterial compliance in mice genetically null for cathepsins K, L or S. J. Biomech.143:111266, 2022.
Holzapfel, G. A. Nonlinear Solid Mechanics: A Continuum Approach for Engineering Science. Hoboken: Wiley, 2000.
Dong, H., J. Wang, and M. Rubin. A nonlinear cosserat interphase model for residual stresses in an inclusion and the interphase that bonds it to an infinite matrix. Int. J. Solids Struct. 62:186–206, 2015.
Dong, H., Z. Wang, T. C. O’Connor, A. Azoug, M. O. Robbins, and T. D. Nguyen. Micromechanical models for the stiffness and strength of UHMWPE macrofibrils. J. Mech. Phys. Solids. 116:70–98, 2018.
Dong, H., M. Liu, C. Martin, and W. Sun. A residual stiffness-based model for the fatigue damage of biological soft tissues. J. Mech. Phys. Solids.143:104074, 2020.
Dong, H., and Y. Hu. Harnessing fluid pre-pressure to tune the properties of phononic crystals. Extreme Mech. Lett.34:100582, 2020.
Ogden, R. W. Non-linear Elastic Deformations. North Chelmsford: Courier Corporation, 1997.
Chen, Y., C. Wen, G. Tao, and M. Bi. Continuous and noninvasive measurement of systolic and diastolic blood pressure by one mathematical model with the same model parameters and two separate pulse wave velocities. Ann. Biomed. Eng. 40(4):871–882, 2012.
Rogers, W. J., Y.-L. Hu, D. Coast, D. A. Vido, C. M. Kramer, R. E. Pyeritz, and N. Reichek. Age-associated changes in regional aortic pulse wave velocity. Journal of the American College of Cardiology. 38(4):1123–1129, 2001.
Learoyd, B. M., and M. G. Taylor. Alterations with age in the viscoelastic properties of human arterial walls. Circ. Res. 18(3):278–292, 1966.
Sokolis, D. P., G. D. Savva, S. A. Papadodima, and S. K. Kourkoulis. Regional distribution of circumferential residual strains in the human aorta according to age and gender. J. Mech. Behav. Biomed. Mater. 67:87–100, 2017.
Milkovich, N., A. Gkousioudi, F. Seta, B. Suki, and K. Y. Zhang. Harmonic distortion of blood pressure waveform as a measure of arterial stiffness. Front. Bioeng. Biotechnol. 10:842754, 2022.
Hughes, D., C. F. Babbs, L. Geddes, and J. Bourland. Measurements of Young’s modulus of elasticity of the canine aorta with ultrasound. Ultrason. Imaging. 1(4):356–367, 1979.
Liu, M., L. Liang, F. Sulejmani, X. Lou, G. Iannucci, E. Chen, B. Leshnower, and W. Sun. Identification of in vivo nonlinear anisotropic mechanical properties of ascending thoracic aortic aneurysm from patient-specific CT scans. Sci. Rep. 9(1):1–13, 2019.
Liu, M., L. Liang, and W. Sun. Estimation of in vivo mechanical properties of the aortic wall: A multi-resolution direct search approach. J. Mech. Behav. Biomed. Mater. 77:649–659, 2018.
Wittek, A., W. Derwich, K. Karatolios, C. P. Fritzen, S. Vogt, T. Schmitz-Rixen, and C. Blase. A finite element updating approach for identification of the anisotropic hyperelastic properties of normal and diseased aortic walls from 4D ultrasound strain imaging. J. Mech. Behav. Biomed. Mater. 58:122–138, 2016.
Wittek, A., K. Karatolios, P. Bihari, T. Schmitz-Rixen, R. Moosdorf, S. Vogt, and C. Blase. In vivo determination of elastic properties of the human aorta based on 4D ultrasound data. J. Mech. Behav. Biomed. Mater. 27:167–183, 2013.
Dong, H., M. Liu, T. Qin, L. Liang, B. Ziganshin, H. Ellauzi, M. Zafar, S. Jang, J. Elefteriades, and W. Sun. Engineering analysis of aortic wall stress and root dilatation in the V-shape surgery for treatment of ascending aortic aneurysms. Interactive Cardiovasc. Thorac. Surg. 2022. https://doi.org/10.1093/icvts/ivac004.
Liu, M., L. Liang, and W. Sun. A new inverse method for estimation of in vivo mechanical properties of the aortic wall. J. Mech. Behav. Biomed. Mater. 72:148–158, 2017.
Liu, M., L. Liang, and W. Sun. Estimation of in vivo constitutive parameters of the aortic wall using a machine learning approach. Comput. Methods Appl. Mech. Eng. 347:201–217, 2019.
Qin, T., A. Caballero, W. Mao, B. Barrett, N. Kamioka, S. Lerakis, and W. Sun. Patient-specific analysis of bicuspid aortic valve hemodynamics using a fully coupled fluid-structure interaction (FSI) model. medRxiv. 153:S52, 2021.
Mao, W., A. Caballero, R. McKay, C. Primiano, and W. Sun. Fully-coupled fluid-structure interaction simulation of the aortic and mitral valves in a realistic 3D left ventricle model. PLoS ONE.12(9):e0184729, 2017.
Mao, W., K. Li, and W. Sun. Fluid–structure interaction study of transcatheter aortic valve dynamics using smoothed particle hydrodynamics. Cardiovasc. Eng. Technol. 7(4):374–388, 2016.
Qin, T., A. Caballero, R. T. Hahn, R. McKay, and W. Sun. Computational analysis of virtual echocardiographic assessment of functional mitral regurgitation for validation of proximal isovelocity surface area methods. J. Am. Soc. Echocardiogr. 34(11):1211–1223, 2021.
Han, D., G. Liu, and S. Abdallah. An Eulerian–Lagrangian–Lagrangian method for 2D fluid-structure interaction problem with a thin flexible structure immersed in fluids. Comput. Struct.228:106179, 2020.
Han, D., G. Liu, and S. Abdallah. An Eulerian–Lagrangian–Lagrangian method for solving fluid-structure interaction problems with bulk solids. J. Comput. Phys.405:109164, 2020.
Han, D., G. Liu, and S. Abdallah. ELL for 3D FSI problems with thin flexible structures based on the continuum-based shell element. J. Fluids Struct.103:103281, 2021.
Acknowledgments
This study is supported by NIH (R01HL155537 and R01HL142036).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Associate Editor Jane Grande-Allen oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix: Stress Calculation
Appendix: Stress Calculation
The Cauchy stress of the arterial tissue can be expressed as [34]
where p is a Lagrange contribution to the hydrostatic pressure, and
where
Substituting Eqs. (1)–(3) into Eq. (24), we have
For the cylindrical artery tube under inner pressure with fixed axial pre-stretch, the deformation gradient can be expressed as \(\varvec{F}=\mathrm{diag}[1/({\lambda }_{\theta }{\lambda }_{z}),{\lambda }_{\theta },{\lambda }_{z}]\). Then we have \({\overline{I} }_{4\theta }={\lambda }_{\theta }^{2}\) and \({\overline{I} }_{4z}={\lambda }_{z}^{2}\). Substituting \({\overline{I} }_{4\theta }\) and \({\overline{I} }_{4z}\) into Eq. (25) and then into Eqs. (22)–(24), together with the condition of \({\sigma }_{rr}=0\), the non-zero components of the Cauchy stress can be expressed as
Further, the non-zero components of the 2nd P–K stress can be expressed as
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dong, H., Liu, M., Woodall, J. et al. Effect of Nonlinear Hyperelastic Property of Arterial Tissues on the Pulse Wave Velocity Based on the Unified-Fiber-Distribution (UFD) Model. Ann Biomed Eng 51, 2441–2452 (2023). https://doi.org/10.1007/s10439-023-03275-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-023-03275-1