Abstract
The purpose of this study was to determine the incidence of pelvic adhesion formation at second-look surgery after laparoscopic excision of the pelvic peritoneum for pelvic endometriosis. The setting was a district hospital in the UK with a specialised unit for laparoscopic surgical treatment of endometriosis; this was a retrospective study. We used data from the hospital computer database to identify patients who had undergone laparoscopic excision of pelvic endometriosis from April 1998 to March 2004. All subsequent admissions for surgery (laparoscopic or open) were reviewed for the presence of pelvic adhesions as documented in the records and collaborated with photographs from surgery. Forty-eight cases were identified from a cohort of 236 patients who initially had laparoscopic excision of pelvic peritoneum affected with endometriosis. Forty-six had laparoscopic surgery and two had open surgery. At second look surgery, 44 patients (91.7%) had no de-novo pelvic adhesions in the areas where the initial excision was performed. Four patients (8.3%) had filmy adhesions in the pelvis; these patients had other surgical procedures (two had LAVH) or on-going disease (one with recto-vaginal endometriosis nodule and the other with ovarian endometrioma at initial surgery). There were no dense or significant pelvic adhesions. Laparoscopic excision of the pelvic peritoneum as a treatment for pelvic peritoneal endometriosis is not associated with significant pelvic adhesion formation.
Similar content being viewed by others
Introduction
The role of surgery in the treatment for pelvic peritoneal endometriosis has been validated by several studies [1–7]. Surgical treatment by laparoscopic excision of pelvic peritoneal endometriosis is effective in relieving dysmenorrhoea, dyspareunia, chronic pelvic pain and dyschezia [2]. The Cochrane systematic review also agreed that surgical treatment has a beneficial effect on pelvic pain and infertility in women with mild to moderate endometriosis [3]. However this benefit has to be balanced with the risk of pelvic adhesion formation after surgery.
Adhesion formation is common and occurs after almost every abdominal surgery [8]. It is difficult to ascertain the true incidence of peritoneal adhesion formation after surgery because adhesions may vary from minimal asymptomatic scarring to dense adhesions and none of the scoring systems for adhesions has been validated [9]. The reported incidence of postoperative peritoneal adhesion formation after surgery has been reported to be as high as 60%–95% in patients at subsequent surgery [9, 10]. Recent epidemiological data have demonstrated that one-third of patients who had open surgery were readmitted with adhesion-related complications within 10 years [11]. A subsequent analysis (SCAR-2) of women who had gynaecological operation-laparoscopy or laparotomy-also showed an increased risk of adhesion-related admission [12]. It also confirms that certain open surgical procedures (e.g., ovarian, tubal and adhesiolysis) have a higher risk of adhesion formation.
Although the majority of adhesions has no detrimental effect on women, a proportion suffers serious short- and long-term consequences including fertility-related problems, chronic pelvic pain, and bowel obstruction [8]. The impact on the quality of life of these women is difficult to calculate. However, one could infer it from the increased number of claims against gynaecologists by these women. Between 1994 and 1999, the UK Medical Defence Union received 77 adhesion-related claims that resulted in 14 out-of-court settlements in 11 years, averaging £50,765 per case [8]. Its impact on the healthcare system is also enormous. The estimated cost for the UK population, as extrapolated from the SCAR study in 1994, is about 67 million pounds [8].
In this paper, we set out to look specifically at the incidence of adhesion formation in patients who had total or partial laparoscopic excision of the pelvic peritoneum for pelvic endometriosis between 1988 and 2004. This paper to our knowledge is the first of its kind to look into the incidence of adhesion formation after total or partial peritoneal excision.
Method
This is a retrospective survey. It included all patients who had either a total or partial laparoscopic excision of pelvic peritoneum for pelvic endometriosis from April 1988 to March 2004 under the care of Mr Trehan at the Dewsbury District Hospital.
We obtained data from the hospital computer database to identify all patients who had laparoscopic excision of pelvic peritoneum endometriosis during the study period.
Operative technique
All patients were admitted the day prior to surgery and had systemic bowel preparation. A three-port surgical procedure is performed, with a 10-mm port at the umbilicus, and the side ports were 12 mm and 5 mm. Scissors dissection of the pelvic peritoneum and endometriotic implants was performed. The use of diathermy was usually minimal. Intra-abdominal pressure at operation was 12 mmHg with saline and heparin irrigation (5,000 in of heparin in 1,000 ml of saline). All patients had intravenous antibiotics (cefuroxime 750 mg and metronidazole 500 mg) and adhesion prevention solution instilled (see Table 2) into the pelvic and abdominal cavity at the end of operation. The diagnosis was confirmed by histological examination of tissues removed at surgery. The majority of patients were discharged home the next day.
It is the usual practice in the unit and by the surgeon, Mr Trehan, to obtain photographs of the abdominal cavity and pelvis during laparoscopic operations in addition to written documentation in the patient’s case records. See Fig. 1.
All subsequent admissions for abdominal surgery were reviewed for the presence of pelvic adhesions as documented in the case records and collaborated with photographs from surgery. The presence of adhesion was deducted by comparing the pictures from the first laparoscopic surgery to the pictures at the second operation.
The classification of adhesions we used was the operative laparoscopic study group (OLSG) classification [13]. Adhesions were placed as: 0, none; 1, filmy and avascular; 2, dense and vascular; and 3, binding and cohesive.
Result
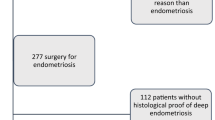
Two hundred thirty-six patients were identified who had laparoscopic excision of pelvic peritoneum for pelvic endometriosis from April 1998 to March 2004. Forty-eight patients from the initial cohort returned to the unit for a second abdominal operation, either diagnostic or therapeutic.
The age range of patients was 20–42 years, with an average age of 32.39 years. Twenty-four patients were nulliparous; 7 were para 1; 12 were para 2; 7 were para 3 or more. The primary surgery for the cohort of patients who went on to have a second operation is shown in Table 1.
At surgery, 25/48 (52.08%) patients had stage 1, 14/48(29.16%) had stage 2, 5/48(10.42%) had stage 3 and 4/48(8.33%) had stage 4 endometriosis according to the revised American Fertility Society classification (rAFS).
All patients had post-operation adhesion prevention solution, albeit different brands (Table 2). In the study group, a majority 23/48 (47.92%) of patients had no post-operative medical treatment; 22/48 (45.83%) of patients had post-operative gonadotrophin-releasing hormone analogue treatment for 3 months, and 3/48 (6.25%) had Danazol treatment for 3 months.
The surgical procedure at subsequent second-look surgery is shown in Table 3.
The time interval between first operation and subsequent surgery is shown in Table 4.
The presence and type of pelvic adhesions in the patients who had a subsequent abdominal surgical procedure according to the OLSG classification [13] is shown in Table 5.
Discussion
In our series, 44 patients (91.7%) had no adhesions in the pelvis. Four patients had class 2 or filmy pelvic adhesions, that is, an incidence of 8.3%. In the four patients with adhesions, one had rAFS* stage IV disease with a recto-vaginal endometriotic nodule that was treated at second operation, one had rAFS stage III disease with an ovarian endometrioma and two had rAFS stage I disease had laparoscopic-assisted vaginal hysterectomy at primary surgery. We would deduce from our result that the presence of on-going endometriosis and additional major surgical procedure at the time of peritoneum excision increases the risk of adhesion formation.
The reasons for this good outcome, i.e., low incidence of adhesion could be due to a combination of the following factors.
-
1.
Operator experience
-
2.
Operator technique
-
3.
Use of adhesion prevention adjuvant.
One surgeon, who had been trained in advanced laparoscopic surgery and practiced the same for over a decade, performed all operations. The role of good training in endoscopic surgery is not questionable. However there is currently an unresolved debate on the way forward in training-an apprenticeship model or modular training [14].
Adhesion formation starts after localised injury to the mesothelial layer of the peritoneum. The interaction between post-traumatic inflammatory proteins and fibrin deposits at the injury sites finally leads to adhesion formation [8]. Surgical technique is important to prevent adhesion formation after pelvic surgery [9]. Laparoscopic surgery is associated with less risk of adhesion formation as compared to laparotomy [12, 15–17]. Our surgical technique of laparoscopic excision with scissors dissection, minimal use of diathermy, gentle tissue handling, meticulous haemostasis and copious irrigation prevents charring of tissues due to thermal injury. This leads to a reduced stimulus for an inflammatory cascade reaction following tissue trauma and therefore less adhesion formation post surgery.
In our unit, all patients undergoing laparoscopic excision of endometriosis have intra-operative irrigation with saline mixed with heparin in addition to adhesion prevention solution at the end of surgery. The use of adhesion prevention solution has been extensively studied in the last decade. The general consensus from published data is that an adhesion prevention solution or barrier significantly reduces the incidence of post-operative adhesion formation [18–23]. The safety profile of the patients treated with adhesion prevention solution was comparable to those treated with lactated Ringer’s solution [22, 23].
However several reports suggest that the use of gonadotrophin-releasing hormone angonist reduces pelvic adhesion after surgery [24–26]. The use of medical treatment after surgery is not routine in our unit and some patients decline to have this treatment after counselling because of the side effects. The effect on our result is limited because a majority of our patients did not have this treatment.
Our paper is the first to report on the incidence of adhesion formation after laparoscopic excision of the total or partial pelvic peritoneum with scissors dissection and post-operative use of adjuvant adhesion prevention solution. Our study suggests that laparoscopic excision of the pelvic peritoneum is a safe and effective treatment approach for women with pelvic peritoneum endometriosis. Also, if surgery is carried out in trained hands and with adherence to good surgical practice, it does not cause dense adhesion in the pelvis.
We accept there are limitations to this paper. It is a retrospective study, with a small sample population. However, it offers a snapshot on laparoscopic excision of pelvic peritoneum and pelvic adhesion formation.
References
Garry R, Clayton R, Hawe J (2000) The effect of endometriosis and its radical laparoscopic excision on quality of life indicators. BJOG 107(1):44–54, Jan
Abbott J, Hawe J, Hunter D, Holmes M, Finn P (2004) Garry laparoscopic excision of endometriosis: a randomized, placebo-controlled trial. Fertil Steril 82(4):878–884, Oct
Jacobson TZ, Barlow DH, Garry R, Koninckx P (2001) Laparoscopic surgery for pelvic pain associated with endometriosis. Cochrane Database Syst Rev 2(4):CD001300
Jacobson TZ, Barlow DH, Koninckx PR, Olive D, Farquhar C (2002) Laparoscopic surgery for subfertility associated with endometriosis. Cochrane Database Syst Rev 2(4):CD001398
Keye WR Jr, Hansen LW, Astin M, Poulson AM Jr (1987) Argon laser therapy of endometriosis: a review of 92 consecutive patients. Fertil Steril 47(2):208–212, Feb
Sutton CJ, Ewen SP, Whitelaw N, Haines P (1994) Prospective, randomized, double-blind, controlled trial of laser laparoscopy in the treatment of pelvic pain associated with minimal, mild, and moderate endometriosis. Fertil Steril 62(4):696–700, Oct
Sutton CJ, Pooley AS, Ewen SP, Haines P (1997) Follow-up report on a randomized controlled trial of laser laparoscopy in the treatment of pelvic pain associated with minimal to moderate endometriosis. Fertil Steril 68(6):1070–1074, Dec
Trew G (2004) Consensus in adhesion reduction management. Obstetr Gynaecol Suppl 6(2):1
Monk BJ, Berman ML, Montz FJ (1994) Adhesions after extensive gynecologic surgery: clinical significance, etiology, and prevention. Am J Obstet Gynecol 170(5 Pt 1):1396–1403, May
Menzies D, Ellis H (1990) Intestinal obstruction from adhesions-how big is the problem? Ann R Coll Surg Engl 72(1):60–63, Jan
Ellis H, Moran BJ, Thompson JN, Parker MC, Wilson MS, Menzies D, McGuire A, Lower AM, Hawthorn RJ, O’Brien F, Buchan S, Crowe AM (1999) Adhesion-related hospital readmissions after abdominal and pelvic surgery: a retrospective cohort study. Lancet 353(9163):1476–1480, May 1
Lower AM, Hawthorn RJ, Clark D, Boyd JH, Finlayson AR, Knight AD, Crowe AM, Surgical and Clinical Research (SCAR) Group (2004) Adhesion-related readmissions following gynaecological laparoscopy or laparotomy in Scotland: an epidemiological study of 24,046 patients. Hum Reprod 19(8):1877–1885, Aug. Epub (2004), Jun 3
Chapron C, Guibert J, Fauconnier A, Viera M, Dubuisson JB (2001) Adhesion formation after laparoscopic resection of uterosacral ligaments in women with endometriosis. J Am Assoc Gynecol Laparosc 8(3):368–373, August
Wright J (2005) Training in minimal access gynaecological surgery. Gynecol Surg 2:1–2
Lundorff P, Hahlin M, Kallfelt B, Thorburn J, Lindblom B (1991) Adhesion formation after laparoscopic surgery in tubal pregnancy: a randomized trial versus laparotomy. Fertil Steril 55(5):911–915, May
Takeuchi H, Kinoshita K (2002) Evaluation of adhesion formation after laparoscopic myomectomy by systematic second-look microlaparoscopy. Am Assoc Gynecol Laparosc 9(4):442–446, Nov
Gutt CN, Oniu T, Schemmer P, Mehrabi A, Buchler MW (2004) Fewer adhesions induced by laparoscopic surgery? Surg Endosc 18(6):898–906, Jun, Epub (2004), Apr 27
Farquhar C, Vandekerckhove P, Watson A, Vail A, Wiseman D (2000) Barrier agents for preventing adhesions after surgery for subfertility. Cochrane Database Syst Rev (2):CD000475
Azziz R (1993) Microsurgery alone or with INTERCEED Absorbable Adhesion Barrier for pelvic sidewall adhesion re-formation. The INTERCEED (TC7) Adhesion Barrier Study Group II. Surg Gynecol Obstet 177(2):135–139, Aug
diZerega GS (1996) Use of adhesion prevention barriers in ovarian surgery, tubalplasty, ectopic pregnancy, endometriosis, adhesiolysis, and myomectomy. Curr Opin Obstet Gynecol 8(3):230–237, Jun
Diamond MP (1998) Reduction of de novo postsurgical adhesions by intraoperative precoating with Sepracoat (HAL-C) solution: a prospective, randomized, blinded, placebo-controlled multicenter study. The Sepracoat Adhesion Study Group. Fertil Steril 69(6):1067–1074, Jun
Johns DB, Keyport GM, Hoehler F, diZerega GS, Intergel Adhesion Prevention Study Group (2001) Reduction of postsurgical adhesions with Intergel adhesion prevention solution: a multicenter study of safety and efficacy after conservative gynecologic surgery. Fertil Steril 76(3):595–604, Sep
diZerega GS, Verco SJ, Young P, Kettel M, Kobak W, Martin D, Sanfilippo J, Peers EM, Scrimgeour A, Brown CB (2002) A randomized, controlled pilot study of the safety and efficacy of 4% icodextrin solution in the reduction of adhesions following laparoscopic gynaecological surgery. Hum Reprod 17(4):1031–1038, Apr
Schindler AE (2004) Gonadotropin-releasing hormone agonists for prevention of postoperative adhesions: an overview. Gynecol Endocrinol 19(1):51–55, Jul
Wright JA, Sharpe-Timms KL (1995) Gonadotropin-releasing hormone agonist therapy reduces postoperative adhesion formation and reformation after adhesiolysis in rat models for adhesion formation and endometriosis. Fertil Steril 63(5):1094–1100, May
Sharpe-Timms KL, Zimmer RL, Jolliff WJ, Wright JA, Nothnick WB, Curry TE (1998) Gonadotropin-releasing hormone agonist (GnRH-a) therapy alters activity of plasminogen activators, matrix metalloproteinases, and their inhibitors in rat models for adhesion formation and endometriosis: potential GnRH-a-regulated mechanisms reducing adhesion formation. Fertil Steril 69(5):916–923, May
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Oboh, A., Trehan, A.K. Pelvic adhesion formation at second-look surgery after laparoscopic partial and total peritoneal excision for women with endometriosis. Gynecol Surg 4, 261–265 (2007). https://doi.org/10.1007/s10397-007-0299-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10397-007-0299-0