Abstract
Endoscopic ultrasonography (EUS) is superior to other imaging modalities in the detection of pancreatic masses, although differentiating the types of pancreatic masses detected on EUS remains challenging. However, the value of contrast-enhanced harmonic EUS (CH-EUS) using ultrasound contrast agents for this differentiation has been reported. CH-EUS plays a pivotal role in analysis of small lesions that can only be detected with EUS. Recently, CH-EUS was used for staging and/or determining the resectability of pancreatic cancer in several clinical trials. In addition, it is used to estimate the response of pancreatic cancer to chemotherapy and to determine the prognosis in cases of pancreatic cancer and pancreatic neuroendocrine neoplasms. It is also postulated that CH-EUS improves the diagnostic performance of endoscopic ultrasound-guided fine-needle aspiration biopsy (EUS-FNAB) through complementary diagnoses using CH-EUS and EUS-FNAB, or CH-EUS-guided EUS-FNAB. Thus, CH-EUS has been employed for various qualitative diagnoses, including differentiation of pancreatic masses. Second-generation contrast agents such as Sonazoid are used clinically for ultrasound diagnostic imaging of liver and breast disease. The positioning of CH-EUS with Sonazoid as a test for the diagnosis of solid pancreatic tumors is an issue for further studies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The detection and characterization of pancreatic solid tumors are challenging because the pancreas is a retroperitoneal organ. Endoscopic ultrasonography (EUS) can depict the entire pancreatic parenchyma from the gastroduodenal wall and is useful for the detection of pancreatic tumors, with sensitivity in the range of 96.9–100% [1,2,3,4,5,6]. A meta-analysis evaluating the diagnostic performance of EUS for detection of pancreatic tumors that were negative or inconclusive on multi-detector computed tomography (CT) revealed an area under the receiver operating characteristics (ROC) curve of 0.80 (95% confidence interval CI 0.52–0.89) [7]. Thus, EUS is superior to other imaging modalities in the detection of pancreatic tumors, and is recommended for surveillance of patients at high risk for pancreatic cancer [8].
There are various types of substantial pancreatic solid tumors, including pancreatic cancer (i.e., pancreatic ductal adenocarcinoma), pancreatic neuroendocrine neoplasm (PanNEN), inflammatory masses, and localized autoimmune pancreatitis. Although EUS has limitations in the differential diagnosis of these tumors, contrast-enhanced harmonic EUS (CH-EUS) using an ultrasound contrast agent can be used to evaluate the blood flow in pancreatic tumors detected on EUS, and its utility for their characterization has been reported [9, 10]. In a meta-analysis evaluating the diagnostic performance of CH-EUS for discriminating pancreatic cancer from other pancreatic tumors, its sensitivity, specificity, and area under the ROC curve were 93%, 80,% and 0.97, respectively [11]. It is also reported that a combination of CH-EUS and endoscopic ultrasound-guided fine-needle aspiration biopsy (EUS-FNAB) can further improve diagnostic accuracy for pancreatic cancer [12,13,14].
After definite diagnosis of pancreatic cancers, staging and determination of their resectability are clinically required. Previous systematic reviews and meta-analyses showed the utility of EUS for staging pancreatic cancer [15, 16]. Recently, it was found that CH-EUS showed improved performance over EUS in the diagnosis of portal vein invasion of pancreatic cancer [17]. In addition, the potential of CH-EUS for estimating the effects of chemotherapy on pancreatic cancer and predicting the prognosis of pancreatic cancer or PanNEN was evaluated in clinical trials [18,19,20]. Thus, CH-EUS has been applied to the characterization of pancreatic solid tumors for purposes other than detection or differential diagnosis, and the paradigm shift in the use of CH-EUS has accelerated in recent years. In this review, we summarize previous studies on CH-EUS for diagnosing pancreatic solid tumors and discuss its future perspectives.
CH-EUS for characterization of pancreatic solid tumors
The prognosis for pancreatic cancer remains poor, and early diagnosis and treatment are critical. However, the detection rate for pancreatic cancers smaller than 10 mm, which is expected to influence the long-term prognosis, remains low [21]. Therefore, it is clinically important to detect and diagnose small pancreatic lesions using EUS. The treatment strategy differs greatly depending on the type of pancreatic lesion, and qualitative diagnosis is, therefore, required. EUS can observe the whole pancreas through the gastroduodenal wall, and in this manner, any lesion at any site in the pancreas can be evaluated with CH-EUS. CH-EUS provides qualitative diagnosis of pancreatic masses through the use of ultrasound contrast agents. There are several types of ultrasound contrast agents, and second-generation ultrasound contrast agents such as SonoVue, Definity, and Sonazoid have been widely used in CH-EUS. These contrast agents resonate under low acoustic power and generate a second harmonic component, providing at least several minutes of contrast effect [4, 11]. Sonazoid is often used as an ultrasound contrast agent in Japan, and it facilitates early, late, and Kupffer phase contrast-enhanced ultrasonography. The early, late, and Kupffer phases are defined as 10–30 s, 30–120 s, and 10 min after the injection of Sonazoid, respectively [22]. Although other second-generation ultrasound contrast agents do not yield a Kupffer phase, this is not a drawback in the diagnosis of pancreatic masses, because Kupffer cells are not present in pancreatic parenchyma, and pancreatic tumors are evaluated using only the early and/or late phases.
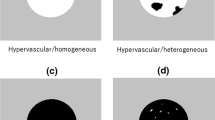
The contrast-enhancement effects on pancreatic masses on CH-EUS are often classified into the following four patterns: non-enhancement, hypo-enhancement, iso-enhancement, and hyper-enhancement (Fig. 1a–d) [10]. Hypo-, iso-, and hyper-enhancement are often observed in pancreatic adenocarcinoma, inflammatory masses, and PanNEN, respectively (Fig. 2a–c) [23]. A patient with a PanNEN that was incidentally detected as a 5-mm low-echoic mass in the pancreatic body on screening EUS at our institution is shown in Fig. 2b. This mass was not detected on contrast-enhanced computed tomography (CE-CT), and qualitative diagnosis with contrast was performed using CH-EUS. A patient with autoimmune pancreatitis (AIP) is shown in Fig. 2c. This case of AIP exhibited a pancreatic head mass that was accompanied with obstructive jaundice, and pancreatic cancer could not be ruled out based on imaging evaluations with conventional EUS and CE-CT. In this patient, CH-EUS revealed an iso-enhancement pattern (Fig. 2c), and no malignant cells were detected on EUS-FNAB, leading to the diagnosis of AIP after a steroid trial. Thus, it is suggested that CH-EUS is useful for the characterization of all pancreatic masses, as well as masses only visible on EUS.
Schema of the four enhancement patterns on CH-EUS. a Non-enhancement, b hypo-enhancement, c iso-enhancement, d hyper-enhancement. This figure is adapted and partially modified from a previous report (Kitano et al. [4])
The images on the left show monitor-mode, and the images on the right show CH-EUS. a A patient with pancreatic adenocarcinoma showing a hypo-enhancing mass (arrowheads). b A patient with G2 PanNEN showing a hyper-enhancing mass (arrowheads). c A patient with focal-type AIP showing an iso-enhancing mass (arrow heads)
Eight recent studies on the diagnosis of pancreatic cancers using CH-EUS include seven prospective studies and one retrospective study (Table 1) [9, 10, 24,25,26,27,28,29]. The number of patients in each of the eight studies ranged from 35 to 277. SonoVue or Sonazoid was used as the contrast agent, depending on the availability in each country. Most of the studies evaluated pancreatic masses in the early and late phases, and all of them agreed that hypo-enhancement was suggestive of pancreatic cancer, although there were some differences in terminology. For disease characterization, it may be better to consider early and late phases in CH-EUS; however, this point is controversial, even among experts. The sensitivity for diagnosing pancreatic cancer ranged from 79.0 to 96.0%, and the specificity ranged from 64.0 to 100%. Four studies compared the diagnostic performance of CH-EUS with that of other diagnostic procedures [9, 10, 24,25,26,27,28,29]. Bunganič et al. found significant differences in accuracy in comparison with conventional EUS [29], and Fusaroli et al. reported CH-EUS to have significantly better specificity [9]. Kitano et al. found no significant difference between CE-CT and CH-EUS in terms of overall diagnostic accuracy, but CH-EUS was superior to CE-CT for small lesions of 2 cm or less [10]. Gincul et al. found comparable diagnostic performance between EUS-FNAB and CH-EUS [26]. It is believed that EUS-FNAB and CH-EUS are complementary in the diagnosis of pancreatic cancer [10]. More recently, elastography, which uses ultrasound to measure tissue stiffness, has also been available for EUS, and several studies attempted to improve the diagnostic performance for pancreatic masses by combining EUS elastography and CH-EUS [30,31,32]. Tanyaporn et al. evaluated 136 patients with pancreatic masses using EUS elastography and CH-EUS, and showed diagnostic sensitivity, specificity, and accuracy of 68.4, 65.4, and 75.7%, respectively, for pancreatic cancers; 83.8, 82.4, and 86.8%, respectively, for PanNENs; and 80.1, 78.7, and 81.6%, respectively, for inflammatory tumors [30]. However, the benefit of combining EUS elastography and CH-EUS for the differential diagnosis of pancreatic masses was not determined in this study. Iglesias-Garcia et al. assessed 62 patients with pancreatic masses using EUS elastography and CH-EUS, and found that for discriminating malignant from benign lesions, the accuracy of EUS elastography, CH-EUS, and the two methods combined was 98.4, 85.5, and 91.9%, respectively, with the differences not being statistically significant [31]. Costache et al. studied EUS elastography with mean strain histogram (SH) analysis in 97 patients with pancreatic masses [32]. They found that if an SH value less than 80 was considered to be a sign of malignancy, the sensitivity, specificity, and accuracy were 100, 29.6, and 80.4%, respectively. When CH-EUS diagnosis was combined with these EUS elastography results, CH-EUS improved the specificity and accuracy of EUS elastography to 81.5 and 93.8%, respectively [31]. Thus, future research is needed on the combined use of EUS elastography and CH-EUS for the diagnosis of pancreatic tumors.
To distinguish localized AIP from pancreatic cancer using CH-EUS is still challenging. Two studies reported that AIP exhibited iso or hyper-enhancement on CH-EUS in 90% of cases [26, 28]. One study, which evaluated the time intensity curve of CH-EUS, showed that peak and maximum intensity gains of AIP were higher than those of pancreatic cancer [32]. In the other study, the echo intensity reduction rate from the peak at 1 min in cases with AIP was lower in cases with pancreatic cancer [33]. Evaluations of endoscopic images, including CH-EUS, are largely subjective, and significant differences in diagnostic performance can occur between beginners and experts. Artificial intelligence (AI) has the potential to solve this problem, and several studies on AI-assisted EUS imaging for the diagnosis of pancreatic cancer have been reported [34,35,36]. Tang et al. investigated the diagnostic performance of AI-assisted CH-EUS for malignant pancreatic tumors, comparing it with subjective diagnosis of CH-EUS in 39 patients [36]. In this study, the sensitivity, specificity, and accuracy of subjective diagnosis of CH-EUS were 88.5, 84.6, and 87.2%, respectively, while the corresponding values for AI-assisted CH-EUS were 92.3, 92.3, and 92.3%, respectively, with the differences being statistically significant (P < 0.05).
CH-EUS for staging of pancreatic cancer
In pancreatic cancer treatment, identification of the clinical stage is important for determining the treatment strategy and prognosis. In a systematic review published in 2006, the accuracy rates of CE-CT and conventional EUS for T-staging of pancreatic cancer were 68%–85% and 23%–75%, respectively [15]. In a 2014 meta-analysis evaluating the diagnostic performance of conventional EUS for T-staging of pancreatic cancers, the sensitivity, specificity, and odds ratio for differentiation between T1/T2 and T3/T4 were 72%, 90%, and 24.69, respectively [16]. In a 2020 meta-analysis, the sensitivity, specificity, odds ratio, and area under the curve of conventional EUS for determining the resectability of pancreatic cancers were 87%, 63%, 11.51, and 0.75, respectively, while those of CE-CT were 87%, 70%, 15.91, and 0.78, respectively [37]. These results indicate that the diagnostic performance of CE-CT and EUS is comparable in terms of T-staging of pancreatic cancers. There are a few reports on CH-EUS for T- and N-staging of pancreaticobiliary cancer (Table 2) [17, 38,39,40]. Imazu et al. examined pancreatic and biliary malignancies using CH-EUS, and showed that CH-EUS had a high accuracy of 92.4% for T-staging [38]. In addition, this study also examined the diagnosis of portal vein involvement, reporting sensitivity and specificity of 100% and 100% for CH-EUS, and 100% and 82.6%, respectively, for conventional EUS, although the differences were not statistically significant (Table 2).
Evaluation of vascular invasion by pancreatic cancer is particularly crucial for determining resectability, and according to a systematic review, the correct diagnosis rates of conventional EUS and CE-CT range from 68 to 100% and 41 to 83%, respectively [15]. Although it was unclear whether CH-EUS was superior to conventional EUS for T-staging of pancreatic cancer, the vascular invasion from pancreatic cancer was visualized more clearly on CH-EUS [39]. Nakai et al. examined 88 patients with pancreatic cancer who underwent surgical resection and found that the portal vein wall was depicted as a single-layer avascular line on CH-EUS (Fig. 3a) [17]. It is presumed that this is because the nutrient vessels in the wall of large blood vessels are too thin to allow contrast agents to flow into them, and they, therefore, appear as a single-layer avascular line on CH-EUS. When disruption of this avascular line was defined as portal vein invasion (Fig. 3b), the accuracy of CH-EUS for the presence of portal vein involvement was 93.2%, which was significantly higher than that of conventional EUS (P = 0.0022) or CE-CT (P = 0.0094) [17]. Miyata et al. evaluated the utility of CH-EUS for N-staging of pancreatobiliary malignancies in 103 patients, including 67 pancreatic cancers and 36 biliary cancers [40]. When heterogeneous enhancement on CH-EUS was considered to be a sign of a malignant lymph node, the diagnostic accuracy of CH-EUS was superior to the morphological diagnostic capability of EUS (Table 2). Although EUS-FNAB is useful for the diagnosis of lymph node metastasis from pancreaticobiliary cancers, it is not practical to perform EUS-FNAB on all lesions when many enlarged lymph nodes are observed on EUS [40]. CH-EUS is likely to solve this problem because it allows selection of the lymph node most likely to be malignant among those that are enlarged. There is little evidence that CH-EUS is useful for staging or diagnosis of local invasion in patients with pancreatic cancer, and further prospective studies with large numbers of patients are required.
The images on the left show monitor-mode, and the images on the right show CH-EUS. a:A patient with pancreatic adenocarcinoma without portal vein invasion showing a hypo-enhancing mass (arrow). The intact portal vein wall is depicted as a single-layer avascular line on CH-EUS (arrowheads). b A patient with pancreatic adenocarcinoma with portal vein invasion showing a hypo-enhancing mass (arrow). The continuity of the single-layer avascular line is disrupted (arrowheads)
CH-EUS for determining the prognosis and effectiveness of treatment
The usefulness of CH-EUS for determining the prognosis and efficacy of chemotherapy in patients with pancreatic tumors has been reported [19, 20]. As mentioned above, the enhancement patterns of CH-EUS within the same type of pancreatic tumor are generally consistent [23]. However, there are slight differences in enhancement pattern according to their malignancy or treatment status. The response of patients with advanced pancreatic cancer to chemotherapy varies from one patient to another. Appropriate assessment of the response to chemotherapy can be an indicator of whether a change in regimen is warranted. Tanaka et al. evaluated 23 patients with pancreatic cancer and focused on appearance of an avascular area in the tumor on CH-EUS after chemotherapy [20]. They reported that an avascular area appeared in 77.8% of the patients who showed a good response to chemotherapy, but in only 28.6% of those who showed a poor response, with the difference being statistically significant. It was reported that avascular areas within pancreatic cancers reflect areas showing fibrosis and necrosis on histological analysis [41]. Therefore, it is assumed that the appearance of an avascular area after chemotherapy reflects tumor necrosis caused by chemotherapy, and that CH-EUS might be useful for determining the efficacy of chemotherapy.
Emori et al. investigated the relationship between enhancement patterns on CH-EUS and life prognosis in patients with pancreatic cancer [19]. They evaluated 145 CH-EUS images obtained before chemotherapy with gemcitabine and nab-paclitaxel, and found that a group with more tumor blood flow in both the early and late phases of CH-EUS had significantly longer progression-free survival and a better response to chemotherapy. It was reported that lesions with low blood flow in the early phase of CH-EUS reflect tumors with necrosis, fibrosis, and few blood vessels on histological analysis, but the mechanism by which this finding affects the prognosis is unclear [28].
PanNENs are usually graded using the Ki67 index, which does not always correlate with clinical aggressiveness [42, 43]. Ishikawa et al. reported on CH-EUS evaluation and clinical grading of 47 patients with PanNENs [18]. In their study, an aggressive PanNEN was defined as neuroendocrine carcinoma, mixed neuroendocrine non-neuroendocrine neoplasm, and PanNENs of any grade with distant metastasis. They found that CH-EUS was useful for differentiating between aggressive and non-aggressive PanNENs, with sensitivity, specificity, and accuracy for diagnosing aggressive PanNENs of 94.7%, 100%, and 97.9%, respectively. Furthermore, it was indicated that CH-EUS has potential for estimating the prognosis of patients with PanNENs.
CH-EUS-FNAB
EUS-FNAB is commonly used for pathological diagnosis of pancreatic masses. According to meta-analyses evaluating the diagnostic performance of EUS-FNAB for pancreatic cancers, its sensitivity, specificity, and accuracy ranged between 84 and 92%, 96 and 98%, and 86 and 91%, respectively [44]. Diagnoses made based on EUS-FNAB findings are subject to a small number of false-positives and false-negatives. Recently, several studies have attempted to improve the diagnostic performance of EUS-FNAB by performing contrast-enhanced harmonic endoscopic ultrasound-guided fine-needle aspiration biopsy (CH-EUS-FNAB), and these studies are summarized in Table 3 [12,13,14, 24, 26, 45,46,47].
The advantages of CH-EUS-FNAB are that the margin of the tumor is clarified by CH-EUS, making it easier to identify the puncture target, and that hot spots can be sampled, avoiding necrosis inside the tumor, which is depicted as non-enhancing areas (Fig. 4). The procedure for EUS-FNAB requires a certain amount of time, and therefore, second-generation ultrasound contrast agents such as Sonovue, Definity, or Sonazoid, which have a prolonged contrast period [4, 11], are preferable for use during CH-EUS-FNAB. Numata et al. compared enhancement patterns on transabdominal contrast-enhanced ultrasonography with pathological findings of surgically resected specimens, and found that pancreatic tumors with poor contrast enhancement had more necrotic and fibrotic cells [41]. Kamata et al. found that the sensitivity of EUS-FNAB for diagnosing pancreatic adenocarcinoma was significantly lower in patients with lesions showing non-enhancing areas on CH-EUS than in those without them (72.9% vs. 94.3%) [48]. Thus, the presence of a non-enhancing area within the tumor has a significant negative impact on EUS-FNAB performance.
Several studies have evaluated the utility of EUS-FNAB under CH-EUS guidance (i.e., CH-EUS-FNAB) [12,13,14, 24, 26, 45,46,47]. These studies, which are summarized in Table 3, consist of six prospective and two retrospective trials, and six are comparative studies. Two studies provide information on the number of patients with non-enhancing areas [14, 47]. Sugimoto et al. found that CH-EUS detected non-enhancing areas in 20 out of 40 consecutive patients with pancreatic cancer [47], while Itonaga et al. noted that 34 out of 93 patients had a non-enhancing area [14]. The importance of avoiding non-enhancing areas when performing the puncture was raised in four studies [13, 14, 46, 47], while three studies described targeting the hypo-enhancing area during CH-EUS-FNAB [12, 26, 45]. In summary, the sensitivities of EUS-FNAB and CH-EUS-FNAB ranged from 68.8 to 85.5% and 79.0 to 96.0%, respectively, and the specificities were 100% (all studies) and 94–100%, respectively (Table 3). Eight studies showed that the sensitivity of CH-EUS-FNAB was higher than that of EUS-FNAB [12,13,14, 24, 26, 45,46,47], but only one study showed a statistically significant difference [14]. The technique used for EUS-FNAB depends on the skill of the endosonographer, and therefore, the degree to which CH-EUS improves EUS-FNAB performance might differ between beginners and experts, and further studies are required to clarify the significance of CH-EUS.
Change history
14 March 2024
A Correction to this paper has been published: https://doi.org/10.1007/s10396-024-01435-x
References
Yasuda K, Mukai H, Nakajima M, et al. Staging of pancreatic carcinoma by endoscopic ultrasonography. Endoscopy. 1993;25:151–5.
Akahoshi K, Chijiiwa Y, Nakano I, et al. Diagnosis and staging of pancreatic cancer by endoscopic ultrasound. Br J Radiol. 1998;71:492–6.
DeWitt J, Devereaux B, Chriswell M, et al. Comparison of endoscopic ultrasonography and multidetector computed tomography for detecting and staging pancreatic cancer. Ann Intern Med. 2004;141:753–63.
Kitano M, Kudo M, Maekawa K, et al. Dynamic imaging of pancreatic diseases by contrast enhanced coded phase inversion harmonic ultrasonography. Gut. 2004;53:854–9.
Sakamoto H, Kitano M, Suetomi Y, et al. Utility of contrast-enhanced endoscopic ultrasonography for diagnosis of small pancreatic carcinomas. Ultrasound Med Biol. 2008;34:525–32.
Jemaa Y, Houissa F, Trabelsi S, et al. Endoscopic ultrasonography versus helical CT in diagnosis and staging of pancreatic cancer. Tunis Med. 2008;86:346–9.
Krishna SG, Rao BB, Ugbarugba E, et al. Diagnostic performance of endoscopic ultrasound for detection of pancreatic malignancy following an indeterminate multidetector CT scan: a systemic review and meta-analysis. Surg Endosc. 2017;31:4558–67.
Canto MI, Hruban RH, Fishman EK, et al. Frequent detection of pancreatic lesions in asymptomatic high-risk individuals. Gastroenterology. 2012;142:796–804 (quiz e14-5).
Fusaroli P, Spada A, Mancino MG, et al. Contrast harmonic echo-endoscopic ultrasound improves accuracy in diagnosis of solid pancreatic masses. Clin Gastroenterol Hepatol. 2010;8:629-634.e1-2.
Kitano M, Kudo M, Yamao K, et al. Characterization of small solid tumors in the pancreas: the value of contrast-enhanced harmonic endoscopic ultrasonography. Am J Gastroenterol. 2012;107:303–10.
Yamashita Y, Shimokawa T, Napoléon B, et al. Value of contrast-enhanced harmonic endoscopic ultrasonography with enhancement pattern for diagnosis of pancreatic cancer: a meta-analysis. Dig Endosc. 2019;31:125–33.
Facciorusso A, Cotsoglou C, Chierici A, et al. Contrast-enhanced harmonic endoscopic ultrasound-guided fine-needle aspiration versus standard fine-needle aspiration in pancreatic masses: a propensity score analysis. Diagnostics (Basel). 2020;10:792.
Seicean A, Samarghitan A, Bolboacă SD, et al. Contrast-enhanced harmonic versus standard endoscopic ultrasound-guided fine-needle aspiration in solid pancreatic lesions: a single-center prospective randomized trial. Endoscopy. 2020;52:1084–90.
Itonaga M, Kitano M, Kojima F, et al. The usefulness of EUS-FNA with contrast-enhanced harmonic imaging of solid pancreatic lesions: a prospective study. J Gastroenterol Hepatol. 2020;35:2273–80.
Dewitt J, Devereaux BM, Lehman GA, et al. Comparison of endoscopic ultrasound and computed tomography for the preoperative evaluation of pancreatic cancer: a systematic review. Clin Gastroenterol Hepatol. 2006;4:717–25 (quiz 664).
Li JH, He R, Li YM, et al. Endoscopic ultrasonography for tumor node staging and vascular invasion in pancreatic cancer: a meta-analysis. Dig Surg. 2014;31:297–305.
Nakai A, Kamata K, Hyodo T, et al. Utility of contrast-enhanced harmonic EUS for diagnosis of portal vein invasion by pancreatic cancer. Endosc Ultrasound. 2022;11:401–6.
Ishikawa R, Kamata K, Hara A, et al. Utility of contrast-enhanced harmonic endoscopic ultrasonography for predicting the prognosis of pancreatic neuroendocrine neoplasms. Dig Endosc. 2021;33:829–39.
Emori T, Ashida R, Tamura T, et al. Contrast-enhanced harmonic endoscopic ultrasonography for predicting the efficacy of first-line gemcitabine and nab-paclitaxel chemotherapy in pancreatic cancer. Pancreatology. 2022;22:525–33.
Tanaka H, Kamata K, Takenaka M, et al. Contrast-enhanced harmonic endoscopic ultrasonography for evaluating the response to chemotherapy in pancreatic cancer. Dig Liver Dis. 2019;51:1130–4.
Egawa S, Toma H, Ohigashi H, et al. Japan pancreatic cancer registry; 30th year anniversary: Japan pancreas society. Pancreas. 2012;41:985–92.
Kitano M, Yamashita Y, Kamata K, et al. The asian federation of societies for ultrasound in medicine and biology (AFSUMB) Guidelines for Contrast-Enhanced Endoscopic Ultrasound. Ultrasound Med Biol. 2021;47:1433–47.
Kitano M, Kudo M, Sakamoto H, et al. Preliminary study of contrast-enhanced harmonic endosonography with second-generation contrast agents. J Med Ultrason. 2008;35:11–8.
Napoleon B, Alvarez-Sanchez MV, Gincoul R, et al. Contrast-enhanced harmonic endoscopic ultrasound in solid lesions of the pancreas: results of a pilot study. Endoscopy. 2010;42:564–70.
Lee TY, Cheon YK, Shim CS. Clinical role of contrast-enhanced harmonic endoscopic ultrasound in differentiating solid lesions of the pancreas: a single-center experience in Korea. Gut Liver. 2013;7:599–604.
Gincul R, Palazzo M, Pujol B, et al. Contrast-harmonic endoscopic ultrasound for the diagnosis of pancreatic adenocarcinoma: a prospective multicenter trial. Endoscopy. 2014;46:373–9.
Park JS, Kim HK, Bang BW, et al. Effectiveness of contrast-enhanced harmonic endoscopic ultrasound for the evaluation of solid pancreatic masses. World J Gastroenterol. 2014;20:518–24.
Yamashita Y, Kato J, Ueda K, et al. Contrast-enhanced endoscopic ultrasonography for pancreatic tumors. Biomed Res Int. 2015;2015: 491782.
Bunganič B, Laclav M, Dvořáková T, et al. Accuracy of EUS and CEH EUS for the diagnosis of pancreatic tumours. Scand J Gastroenterol. 2018;53:1411–7.
Chantarojanasiri T, Hirooka Y, Kawashima H, et al. Endoscopic ultrasound in diagnosis of solid pancreatic lesions: elastography or contrast-enhanced harmonic alone versus the combination. Endosc Int Open. 2017;5:E1136–43.
Costache MI, Cazacu IM, Dietrich CF, et al. Clinical impact of strain histogram EUS elastography and contrast-enhanced EUS for the differential diagnosis of focal pancreatic masses: a prospective multicentric study. Endosc Ultrasound. 2020;9:116–21.
Imazu H, Kanazawa K, Mori N, et al. Novel quantitative perfusion analysis with contrast-enhanced harmonic EUS for differentiation of autoimmune pancreatitis from pancreatic carcinoma. Scand J Gastroenterol. 2012;47:853–60.
Matsubara H, Itoh A, Kawashima H, et al. Dynamic quantitative evaluation of contrast-enhanced endoscopic ultrasonography in the diagnosis of pancreatic diseases. Pancreas. 2011;40:1073–9.
Ozkan M, Cakiroglu M, Kocaman O, et al. Age-based computer-aided diagnosis approach for pancreatic cancer on endoscopic ultrasound images. Endosc Ultrasound. 2016;5:101–7.
Goyal H, Sherazi SAA, Gupta S, et al. Application of artificial intelligence in diagnosis of pancreatic malignancies by endoscopic ultrasound: a systemic review. Therap Adv Gastroenterol. 2022;15:17562848221093872.
Tang A, Tian L, Gao K, et al. Contrast-enhanced harmonic endoscopic ultrasound (CH-EUS) MASTER: a novel deep learning-based system in pancreatic mass diagnosis. Cancer Med. 2023;12:7962–73.
Rahman MIO, Chan BPH, Far PM, et al. Endoscopic ultrasound versus computed tomography in determining the resectability of pancreatic cancer: a diagnostic test accuracy meta-analysis. Saudi J Gastroenterol. 2020;26:113–9.
Imazu H, Uchiyama Y, Matsunaga K, et al. Contrast-enhanced harmonic EUS with novel ultrasonographic contrast (Sonazoid) in the preoperative T-staging for pancreaticobiliary malignancies. Scand J Gastroenterol. 2010;45:732–8.
Seicean A, Badea R, Stan-Iuga R, et al. Quantitative contrast-enhanced harmonic endoscopic ultrasonography for the discrimination of solid pancreatic masses. Ultraschall Med. 2010;31:571–6.
Miyata T, Kitano M, Omoto S, et al. Contrast-enhanced harmonic endoscopic ultrasonography for assessment of lymph node metastases in pancreatobiliary carcinoma. World J Gastroenterol. 2016;22:3381–91.
Numata K, Ozawa Y, Kobayashi N, et al. Contrast-enhanced sonography of pancreatic carcinoma: correlations with pathological findings. J Gastroenterol. 2005;40:631–40.
Palazzo M, Napoléon B, Gincul R, et al. Contrast harmonic EUS for the prediction of pancreatic neuroendocrine tumor aggressiveness (with videos). Gastrointest Endosc. 2018;87:1481–8.
Rinke A, Müller HH, Schade-Brittinger C, et al. Placebo-controlled, double-blind, prospective, randomized study on the effect of octreotide LAR in the control of tumor growth in patients with metastatic neuroendocrine midgut tumors: a report from the PROMID Study Group. J Clin Oncol. 2009;27:4656–63.
Yang Y, Li L, Qu C, Liang S, et al. Endoscopic ultrasound-guided fine needle core biopsy for the diagnosis of pancreatic malignant lesions: a systematic review and Meta-Analysis. Sci Rep. 2016;6:22978.
Hou X, Jin Z, Xu C, Zhang M, et al. Contrast-enhanced harmonic endoscopic ultrasound-guided fine-needle aspiration in the diagnosis of solid pancreatic lesions: a retrospective study. PLoS One. 2015;10: e0121236.
Seicean A, Badea R, Moldovan-Pop A, et al. Harmonic contrast-enhanced endoscopic ultrasonography for the guidance of fine-needle aspiration in solid pancreatic masses. Ultraschall Med. 2017;38:174–82.
Sugimoto M, Takagi T, Hikichi T, et al. Conventional versus contrast-enhanced harmonic endoscopic ultrasonography-guided fine-needle aspiration for diagnosis of solid pancreatic lesions: a prospective randomized trial. Pancreatology. 2015;15:538–41.
Kamata K, Takenaka M, Omoto S, et al. Impact of avascular areas, as measured by contrast-enhanced harmonic EUS, on the accuracy of FNA for pancreatic adenocarcinoma. Gastrointest Endosc. 2018;87:158–63.
Funding
This work was supported by Grants-in-Aid from Japan Research Foundation for Clinical Pharmacology.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethical approval
The research related to human use complied with all the relevant national regulations and institutional policies was conducted in accordance with the tenets of the Helsinki Declaration, and was approved by the author’s institutional review board or equivalent committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised due to a retrospective open access order.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Otsuka, Y., Kamata, K. A review of contrast-enhanced harmonic endoscopic ultrasonography for pancreatic solid tumors. J Med Ultrasonics (2023). https://doi.org/10.1007/s10396-023-01346-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10396-023-01346-3