Abstract
Purpose
BRCA1 and BRCA2 tumors exhibit different characteristics. This study aimed to assess and compare the ultrasound findings and pathologic features of BRCA1 and BRCA2 breast cancers. To our knowledge, this is the first study to examine the mass formation, vascularity, and elasticity in breast cancers of BRCA-positive Japanese women.
Methods
We identified patients with breast cancer harboring BRCA1 or BRCA2 mutations. After excluding patients who underwent chemotherapy or surgery before the ultrasound, we evaluated 89 cancers in BRCA1-positive and 83 in BRCA2-positive patients. The ultrasound images were reviewed by three radiologists in consensus. Imaging features, including vascularity and elasticity, were assessed. Pathological data, including tumor subtypes, were reviewed.
Results
Significant differences in tumor morphology, peripheral features, posterior echoes, echogenic foci, and vascularity were observed between BRCA1 and BRCA2 tumors. BRCA1 breast cancers tended to be posteriorly accentuating and hypervascular. In contrast, BRCA2 tumors were less likely to form masses. In cases where a tumor formed a mass, it tended to show posterior attenuation, indistinct margins, and echogenic foci. In pathological comparisons, BRCA1 cancers tended to be triple-negative subtypes. In contrast, BRCA2 cancers tended to be luminal or luminal-human epidermal growth factor receptor 2 subtypes.
Conclusion
In the surveillance of BRCA mutation carriers, radiologists should be aware that the morphological differences between tumors are quite different between BRCA1 and BRCA2 patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
BRCA mutations increase the risk of breast cancer; so, in BRCA mutation carriers, it is essential to perform different surveillance compared with women of average breast cancer risk to detect and treat breast cancers in the early stages. Since mammography is not suitable for breast cancer surveillance in BRCA patients, magnetic resonance imaging (MRI) is considered the standard surveillance modality for BRCA carriers [1].
BRCA1 and BRCA2 tumors have different characteristics. The triple-negative (TN) subtype is common in BRCA1 breast cancer. In contrast, the luminal subtype is a common subtype of breast cancer in BRCA2 mutation carriers, which has a similar frequency to non-BRCA breast cancers [2]. We hypothesized that due to their histological differences, BRCA1 and BRCA2 breast cancers demonstrate different imaging characteristics on ultrasound. Pathologic and ultrasound features of BRCA1 and BRCA2 breast cancers were previously assessed, although several essential variables, such as vascularity or elasticity, remain unknown [3]. Also, there are few studies assessing imaging features of BRCA breast cancers in the Japanese population.
Therefore, we aimed to assess and compare ultrasound image findings, including vascularity and elasticity, and pathologic features of BRCA1 and BRCA2 breast cancers in Japanese women based on the categories of the Japan Association of Breast and Thyroid Sonology (JABTS) guidelines. Our primary endpoint was to assess and compare the differences in ultrasonographic features between BRCA1 and BRCA2 breast cancers. Our secondary endpoint was the difference in clinicopathological characteristics between them.
Materials and methods
Study population
A flowchart of the patient selection process is shown in Fig. 1.
This retrospective cohort study was conducted at St. Luke’s Hospital. Patients with breast cancer harboring BRCA1 or BRCA2 mutations between July 2003 and December 2020 were included in the study.
At our institution, we recommend BRCA tests for breast cancer patients who have any of the following characteristics:
-
Under 45 years old
-
TN cancer and under 60 years old
-
Bilateral breast cancer
-
Male breast cancer
-
Family history of breast cancer
The following patients were excluded: patients who underwent preoperative chemotherapy before the ultrasound, patients without lesions that implied malignancy, patients with both BRCA1 and BRCA2 mutations, patients without pathological results, and male patients.
Our study was approved by the institutional review board of our hospital, and the requirement for informed consent was waived due to the retrospective nature of the study (Research number: 20-R238).
Imaging technique
Breast sonography was performed by radiologists and radiology technologists, and all images were assessed by radiologists specializing in breast imaging. Breast sonography was performed at our hospital using one of the following devices: HDI 5000 (Philips Medical Systems, Best, the Netherlands), LOGIQ7 (GE Healthcare, Chicago, IL, USA), EUB-7500 (FUJIFILM Healthcare Corporation, formerly called Hitachi Corporation, Tokyo, Japan), Aplio XG (Toshiba Medical Systems, Tochigi, Japan), HIVISION Preirus (Hitachi Healthcare Corporation, Tokyo, Japan), LOGIC E9 (GE Healthcare), and Aplio i800 (Canon Medical Systems Corporation, Tochigi, Japan). The details of the ultrasound equipment utilized for five patients could not be verified because the ultrasound examinations were performed at the referring hospital. The images were then reviewed and evaluated. Ultrasound findings were checked for B-mode, elastography, and flow imaging (color Doppler image) information.
Data analysis
We assessed and classified the image morphologies based on shape, margin, homogeneity, echo level, vascularity, and elasticity. Three radiologists (one with 4 years of experience in general radiology, one with 2 years of experience in breast radiology, and one with 30 years of experience in breast radiology) reviewed the ultrasound images and reports. Findings were recorded after reaching a consensus. If the assessment was different, we reviewed and discussed the images together and reached a consensus.
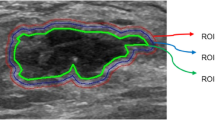
Imaging features were assessed based on the JABTS guidelines. Some terms in the JABTS guidelines are different from the terms in the ACR BIRADS 2013 Ultrasound (Supplementary information). The most significant difference is that the JABTS guidelines classify lesions that cannot be strictly traced as masses as “non-mass abnormalities, ” a category separate from masses. Regarding the classification of vascularity, we defined “high” when tumors were hypervascular and “low” when tumors were hypovascular or avascular. Elasticity was assessed using strain elastography. We used the scoring system introduced by Itoh et al. [4].
The imaging features analyzed in this study are shown in Tables 1 and 2. On B-mode imaging, we classified the tumor morphology as “mass only,” “non-mass abnormalities only,” and “mass with non-mass abnormalities.” We defined “non-mass abnormalities” as tumors in which a definite contour could not be identified. Shape, depth-width ratio, margin, echogenic halo, homogeneity, echo level, and posterior echoes were evaluated in lesions with mass abnormality only and in those with mass and non-mass abnormalities (BRCA1, n = 85; BRCA2, n = 62). The associated findings were evaluated in cases with non-mass abnormalities only and in those with mass and non-mass abnormalities (BRCA1, n = 56; BRCA2, n = 65). Echogenic foci, vascularity, and elasticity were evaluated in all cases. While counting the number of cases with echogenic foci, we did not distinguish whether the echogenic foci had hypoechoic areas or not. Moreover, we reviewed pathological data, including tumor histological classification, nuclear grade, and tumor subtype.
Breast cancer subtypes were categorized into the following four groups: hormone receptor-positive and human epidermal growth factor receptor 2 (HER-2) negative (luminal subtype), hormone receptor-positive and HER-2 positive (luminal-HER-2 subtype), hormone receptor-negative and HER-2 positive (HER-2 subtype), and hormone receptor-negative and HER-2 negative (TN subtype). Luminal tissue was classified as positive when the Allred score of either the estrogen receptor or progesterone receptor was higher than 2. HER-2 was classified as positive if the immunohistochemistry score was 3 or if the immunohistochemistry score was 2 and the fluorescence in situ hybridization test was positive.
Statistical analysis
Missing data from some patients were excluded from the analysis. Since some patients had two or more breast cancers, statistical analysis was performed based on the number of cancers. Data are presented as the mean ± standard deviation or median (range) for continuous variables, such as age and Ki-67, and as numbers (percentages) for categorical variables. We used the t-test and Mann–Whitney U test for continuous variables and the chi-squared and Fisher’s exact tests for categorical variables to compare the characteristics of participants with BRCA1 and BRCA2. Continuous variables were verified by Shapiro–Wilk statistics. A p value < 0.05 indicated a statistically significant difference between groups. If there were statistically significant differences for multiple comparisons, we performed Bonferroni correction as a post hoc analysis. Bonferroni correction is used to compare multiple comparisons. In multiple comparisons, the likelihood of incorrectly rejecting a null hypothesis (type I error) increases. In Bonferroni correction, the alpha value is divided by the number of comparisons to prevent a type I error.
All statistical analyses were performed using EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria) [5].
Results
A total of 289 patients (156 BRCA1 positive, 123 BRCA2 positive, and 10 who were both BRCA1 and BRCA2 positive) were identified. Seventy-three BRCA1-positive patients and 49 BRCA2-positive patients were excluded due to the absence of ultrasound images before chemotherapy or surgery. After excluding ineligible patients, a total of 89 cancers in 81 patients with BRCA1-positive mutations and 83 cancers in 71 patients with BRCA2-positive mutations were included.
Table 3 summarizes the clinicopathological characteristics of the patients. Continuous variables such as age and Ki-67 were refuted, and the Mann–Whitney U test was used for their analysis. Since there were significant differences in tumor type, tumor subtype, and nuclear grade, we performed Bonferroni corrections. The median patient age was 40 (28–70) years in BRCA1 mutation carriers and 42 (28–73) years in BRCA2 mutation carriers. Thus, there was no significant difference in patient age between the two groups (p = 0.288). However, there was a significant difference in the tumor histological classification and subtype (p < 0.001). After Bonferroni correction, BRCA1 tumors were most frequently associated with invasive ductal carcinoma, whereas BRCA2 tumors were more frequently associated with ductal carcinoma in situ (p < 0.001). BRCA1 tumors were associated with the TN subtype (p < 0.001). In contrast, the most common type of BRCA2 breast cancer was luminal-type breast cancer, and the luminal-HER2 type was more frequent in BRCA2 than BRCA1 tumors (p < 0.001). The nuclear grade (p < 0.001) and Ki-67 status (p < 0.001) of BRCA1 tumors were significantly higher than those of BRCA2 tumors.
Table 4 summarizes the imaging characteristics of the patients. Since there were significant differences in tumor morphology, margin, and posterior features, we performed Bonferroni corrections. There was a significant difference in tumor morphology between BRCA1 and BRCA2 tumors (p < 0.001). After Bonferroni correction, BRCA2 tumors were significantly more likely to show non-mass abnormalities only (p < 0.001 vs. mass abnormality only, p = 0.002 vs. mass abnormality with no mass abnormalities) (Fig. 2).
A 46-year-old woman with a BRCA2 mutation and ductal carcinoma in situ (luminal-HER2 subtype). Breast ultrasound demonstrates a hypoechoic area with calcifications. We defined this morphology as no mass. The hypoechoic area shows high vascularity and score 5 elasticity (no strain in the entire lesion or surrounding area). HER2 human epidermal growth factor receptor 2
Among the cases with mass formation, there were no significant differences in shape (p = 0.27), depth-width ratio (p = 0.63), presence or absence of echogenic halo (p = 0.43), homogeneity (p = 0.44), or level of internal echoes (p = 0.12). There was a significant difference in the peripheral features (p = 0.035). BRCA2 tumors were more likely to show indistinct margins compared with BRCA1 tumors. Additionally, there was a significant difference in the posterior acoustic enhancement; after Bonferroni correction, BRCA1 tumors significantly tended to show accentuating posterior echoes (p = 0.001 vs. attenuating, p = 0.002 vs. not changing) (Fig. 3).
Additionally, there was no significant difference in the features of non-mass abnormalities, including abnormality of the ducts (p = 0.20), hypoechoic areas in the mammary gland (p = 0.080), architectural distortion (p = 0.48), and multiple small cysts (no cases).
With regard to flow imaging, BRCA1 tumors tended to show higher vascularity than BRCA2 tumors (p = 0.031). On elastography, BRCA1 tended to have a score of 4 more often. However, the number of patients with a score of 4 or higher, which is considered indicative of malignancy, was almost the same, at 55/68 (80.9%) for BRCA1 and 48/61 (78.7%) for BRCA2.
We detected eight cancer cases with the luminal-HER2 subtype in BRCA2 tumors, but none in BRCA1. Of these luminal-HER2 tumors, five cases did not form masses, four of which had echogenic foci. Moreover, BRCA2 tumors were significantly more likely than BRCA1 tumors to show echogenic foci (p = 0.043).
Discussion
To our knowledge, this is the first study summarizing ultrasound findings of breast cancer in BRCA-positive patients in the Japanese population. BRCA is known to be a high-risk factor for breast cancer, and the frequency of encountering BRCA-positive patients in daily clinical practice has increased since BRCA testing for some individuals started being covered by insurance in Japan. The indication of BRCA testing in Japan includes patients with breast cancer who have any of the following characteristics: < 45 years, TN cancer and < 60 years, two or more breast cancers, male breast cancer, family history of breast cancer within the third-degree relatives. Therefore, it is vital to understand the imaging characteristics of BRCA-positive breast cancer cases.
There is an international consensus that MRI is useful for the surveillance of BRCA-positive patients, and many articles on the imaging characteristics of MRI have already been published [1, 6,7,8]. However, few papers have been published on the imaging features of ultrasound, particularly color Doppler imaging or elastography, especially in Japanese women.
The Japanese guidelines were used in this study because some of the breast ultrasound images could not be described as masses; the Japanese guidelines treat these as “non-mass abnormalities.” Non-mass abnormalities are not introduced in the ACR BIRADS 2013 Ultrasound (Supplementary information). The history of breast ultrasound in Japan is long; thus, the Japanese guidelines are considered to be the default in routine clinical settings.
In the current study, we found that BRCA1 tumors were more likely to show distinct or well-defined and rough margins, accentuating posterior echoes, and high vascularity. BRCA2 tumors were less likely to form masses and had more echogenic foci. BRCA1-associated breast cancers are known to frequently present with benign features, such as round shape, circumscribed margins, and a homogeneous internal structure [9]. Ha et al. compared the clinicopathological and imaging findings of BRCA1 and BRCA2 mutations. They revealed that BRCA1 tumors exhibited posterior acoustic enhancement (p < 0.001) [3], which is in agreement with our findings. Regarding tumor subtypes, BRCA1 breast cancers were associated with a TN subtype, whereas BRCA2 breast cancers were associated with a luminal subtype. These results are consistent with those of a previous study [2]. TN breast cancers are known to be associated with an increased likelihood of distant recurrence and death [10]. The TN breast cancer subtype tends to be a circumscribed tumor with posterior acoustic enhancement [11, 12], which sometimes mimics benign lesions like fibroadenoma. However, in our study, BRCA1 tumors tended to have well-defined and rough margins, high depth-width ratio, and hypervascularization, which are uncommon features of benign tumors like fibroadenoma. If these findings are assessed carefully, we could avoid the misidentification of BRCA1 breast cancers. In contrast, BRCA2 tumors tend to be luminal subtypes, which tend to be non-circumscribed tumors with posterior attenuation or shadowing [12]. These morphological differences suggest that patients with BRCA1 and BRCA2 mutations should be assessed differently.
The rates of echogenic foci, usually representing microcalcifications, and non-mass abnormalities were significantly higher in BRCA2 than in BRCA1 patients. This result may also be attributed to tumor histological differences, where ductal carcinoma in situ is more common in BRCA2. NCC guidelines recommend that surveillance of breast cancer should be conducted with both mammography and MRI in BRCA patients. Although we did not compare the findings of mammography between BRCA1 and BRCA2 patients, the higher rate of echogenic foci in BRCA2 cancers might suggest the importance of mammography in BRCA2 patients. However, not even half of the BRCA2 tumors had echogenic foci, indicating that ultrasound could be a good option in situations where MRI cannot be used. We assessed several important variables in our study, including vascularity and elasticity. We hypothesized that BRCA1 tumors have score 4 elasticity (no strain in the entire lesion) rather than scores 1, 2, 3, or 5 because TN subtype (which is common in BRCA1 cancers) tumors are likely to have well-circumscribed margins. Our results showed that BRCA1 breast cancers tended to demonstrate score 4 elasticity; however, there was no significant difference between BRCA1 and BRCA2 breast cancers. This result might be due to the low number of cancers assessed or the excessively granular subdivision of the scale. BRCA1 tumors were significantly hypervascular compared with BRCA2 tumors. This result reflects the TN subtype tendency of BRCA1 breast cancer.
This study had several limitations. First, it was a retrospective study where radiologists gathered data regarding the presence of cancer. Second, there were several missing data points in some patients, especially in the vascularity and elasticity scores. Third, although some cases were reviewed by several radiologists, most cases were assessed and reviewed by a single radiologist. Finally, this study was performed at a single hospital. A large multicenter study is required to verify our findings.
Conclusion
Our results suggest that BRCA1 breast cancers tend to be masses, posteriorly accentuating, and hypervascular. In contrast, BRCA2 tumors are less likely to form masses. In cases where a tumor forms a mass, it tends to show posterior attenuation, indistinct margins, and echogenic foci. In the surveillance of BRCA mutation carriers, radiologists should be aware that the morphological differences between tumors are quite different between BRCA1 and BRCA2 patients.
Data availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Change history
25 May 2023
A Correction to this paper has been published: https://doi.org/10.1007/s10396-023-01325-8
References
Saslow D, Boetes C, Burke W, et al. American Cancer Society guidelines for breast screening with MRI as an adjunct to mammography. CA Cancer J Clin. 2007;57:75–89.
Nakamura S, Takahashi M, Tozaki M, et al. Prevalence and differentiation of hereditary breast and ovarian cancers in Japan. Breast Cancer. 2015;22:462–8.
Ha SM, Chae EY, Cha JH, et al. Association of BRCA mutation types, imaging features, and pathologic findings in patients with breast cancer with BRCA1 and BRCA2 mutations. AJR Am J Roentgenol. 2017;209:920–8.
Itoh A, Ueno E, Tohno E, et al. Breast disease: clinical application of US elastography for diagnosis. Radiology. 2006;239:341–50.
Kanda Y. Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
Riedl CC, Luft N, Bernhart C, et al. Triple-modality screening trial for familial breast cancer underlines the importance of magnetic resonance imaging and questions the role of mammography and ultrasound regardless of patient mutation status, age, and breast density. J Clin Oncol. 2015;33:1128–35.
Warner E, Plewes DB, Hill KA, et al. Surveillance of BRCA1 and BRCA2 mutation carriers with magnetic resonance imaging, ultrasound, mammography, and clinical breast examination. JAMA. 2004;292:1317–25.
Warner E, Hill K, Causer P, et al. Prospective study of breast cancer incidence in women with a BRCA1 or BRCA2 mutation under surveillance with and without magnetic resonance imaging. J Clin Oncol. 2011;29:1664–9.
Rhiem K, Flucke U, Schmutzler RK. BRCA1-associated breast carcinomas frequently present with benign sonographic features. AJR Am J Roentgenol. 2006;186:E11–2 (author reply E12–3).
Dent R, Trudeau M, Pritchard KI, et al. Triple-negative breast cancer: clinical features and patterns of recurrence. Clin Cancer Res. 2007;13:4429–34.
Rashmi S, Kamala S, Murthy SS, et al. Predicting the molecular subtype of breast cancer based on mammography and ultrasound findings. Indian J Radiol Imaging. 2018;28:354–61.
Cho N. Molecular subtypes and imaging phenotypes of breast cancer. Ultrasonography. 2016;35:281–8.
Watanabe T, Yamaguchi T, Tsunoda H, et al. Ultrasound image classification of ductal carcinoma in situ (DCIS) of the breast: analysis of 705 DCIS lesions. Ultrasound Med Biol. 2017;43:918–25.
Funding
None.
Author information
Authors and Affiliations
Contributions
Conceptualization: HT; Methodology: KI; Formal analysis and investigation: KI; Writing—original draft preparation: KI and HT; Writing—review and editing: ST, KY, YK, NK, HY, and YK; Supervision: HT. All authors have approved the submitted version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Hideko Yamauchi received contracted research funds from AstraZeneca. Other authors have no conflicts of interest to declare.
Ethical statement
This study was approved by the institutional review board of our hospital, and the requirement for informed consent was waived due to the retrospective nature of the study (Research number: 20-R238).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised due to a retrospective open access order.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Ikejima, K., Tokioka, S., Yagishita, K. et al. Clinicopathological and ultrasound characteristics of breast cancer in BRCA1 and BRCA2 mutation carriers. J Med Ultrasonics 50, 213–220 (2023). https://doi.org/10.1007/s10396-023-01296-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10396-023-01296-w