Abstract
Aim
Grounded in Andersen’s Behavioral Model (ABM), this study aims to explore the network of causal relationships between those factors influencing oral health self-management behavior during the COVID-19 pandemic in Australia.
Subject and methods
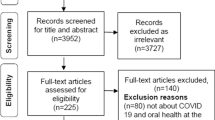
Data were obtained from the Australian population. Participants (N = 565) aged between 19 and 91 years (M = 54.50, SD = 16.16) provided online responses between June 2021 and May 2022. The majority of participants were female (60.9%), employed either full-time (37.65%) or part-time (22.02%), and had completed an undergraduate degree or higher (70.1%). We implemented a triangulated approach, utilizing multiple modeling methodologies including the Gaussian graphical model (GGM), directed acyclic graph (DAG), and structural equation modeling (SEM). These methodologies were employed in three predetermined stages using a single cross-sectional dataset.
Results
A causal model elucidating the influence of the COVID-19 pandemic on oral health self-management behavior was uncovered. The resulting GGM displayed an acceptable fit to the observed data. The DAG structure conformed to that expected by ABM, with all directed edges being also present as edges in the GGM. The subsequent SEM model specified by the DAG provided excellent fit to the data.
Conclusion
Our study offers empirical evidence that factors such as appointment availability, dental care affordability, and the opportunity to engage in oral health discussions with individuals other than dentists during the pandemic directly contributed to inadequate oral health self-care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
After COVID-19 was declared a global pandemic by the World Health Organization (WHO) on March 11, 2020, several countries implemented a range of public policies to mitigate its impact on public health. These measures included lockdowns, travel restrictions, social distancing, testing and contact tracing, and vaccination programs. In addition, there was a significant impact to oral health services, with many countries, including Australia, suspending nonemergency dental care services. This suspension impacted oral health programs in schools and care homes and led to changes in guidelines limiting the provision of oral health services. While these public policies helped limit the introduction of cases from other countries and delayed the widespread transmission of the COVID-19 virus, they likely had long-term negative impacts on oral health (Hopcraft and Farmer 2021). For example, without early diagnosis and management, the progression of conditions such as dental caries and periodontitis was not only inevitable (Coulthard et al. 2020), but also potentially irreversible. Access to routine dental appointments also plays an important factor in promoting good oral health self-management practices, such as tooth brushing and interdental cleaning. However, our understanding of how the COVID-19 pandemic impacted population oral health practices is ambiguous, with some studies indicating a decrease in oral health habits due to lower motivation levels (e.g., Peloso and Pinzan 2021), while others suggest an increase due to a fear of COVID-19 motivating these behaviors (Sari and Bilmez 2021) or no meaningful change at all (Cărămidă et al. 2022).
Understanding the causes of poorer oral health self-management behaviors at a population level during the COVID-19 pandemic is cruical for establishing evidence-based guidelines to promote oral health in future pandemics. To address this research gap, our study aimed to understand the causal structure (see Keyes and Galea 2017), which is the network of causes established between factors present during the COVID-19 pandemic that influenced individual oral health self-management behavior among Australian adults. Given that only cross-sectional data were available during the COVID-19 pandemic, we adopted a triangulated approach to causal discovery (Ryan et al. 2022a). This involved applying multiple modeling methodologies to a single dataset and assessing them for theoretical alignment, structural convergence, and fit. Unlike structural equation modeling (SEM), this approach does not assume the presence of latent variables, nor does it assume the causal structure a priori. Instead, causal discovery approaches employ a variety of computational algorithms to learn the causal structure from the observed data (Scutari et al. 2019). The investigation of causal structures, at a observational rather than latent variable level, has been referred to as the network approach (Briganti et al. 2022b). Several empirical studies have used both directed and undirected graphical modeling to gain further insight into processes such as obsessive–compulsive disorder and depression (McNally et al. 2017), and quality of life (Zhou et al. 2022).
In the causal discovery approach employed in our study, the Gaussian graphical model (GGM) is first estimated. The GGM is a special case of a pairwise Markov random field, which is an undirected graphical model indicating the conditional associations established between variables (Borsboom et al. 2021). We then estimated the causal structure as a directed acyclic graph (DAG) via the Peter and Clark (PC)-stable causal discovery algorithm following Colombo and Maathuis (2014). The PC-stable algorithm operates under three assumptions: (1) that each variable is conditionally independent of its non-descendants, given its parents (causal Markov condition); (2) that conditional dependencies between variables are consistent with the DAG that generated the data (faithfulness); and (3) that all common-cause variables of a variable pair within the causal structure are also included in the causal structure (causal sufficiency). Essentially, the algorithm initially considers all undirected edges between variables and then removes edges according to conditional dependencies, with the directions of edges being determined based on collider structures and the rules of orientation propagation.Footnote 1
When the underlying causal structure is a DAG, the GGM provides a representation of the moral graph, which is the equivalent undirected form of a DAG. For example, the presence of an edge between two variables within the GGM is indicative of either a direct causal relationship or the presence of a collider structure (see Fig. 1). As a result, the GGM includes all edges present within the DAG in addition to edges representing a collider structure. This means that by comparing the resulting estimated DAG structure against the GGM moral structure, the validity of the DAG may be tested. For example, in the GGM, the absence of an edge is “more informative because it confirms that two variables are causally independent” (Ryan et al. 2022b, p. 957). Thus, when the GGM and DAG agree, the validity of the DAG is strengthened, providing evidence towards the robustness of the causal structure.
Directed acyclic graph (DAG) and the Gaussian graphical model (GGM) it generates. Edges A → C and B → C represent causal effects forming a collider structure within the DAG. In the corresponding GGM, edges A–C, B–C, and A–B represent partial correlations between node pairs. Edges A–C and B–C are generated by the causal effects, and edge A–B is generated instead by the collider structure (under the rules of d-separation). In the GGM, edge widths represent the magnitude of the partial correlation coefficients.
Finally, considering that DAGs are non-parametric structural equation models (SEMs) (Hernán and Robins 2006), we specified a SEM using the causal pathways present in the estimated DAG. Under the assumption of linearity, it was possible to estimate the causal effects and test the model's fit (VanderWeele 2012). Our aim was to identify the potential causal structure and estimate the causal effects, both direct and/or indirect, influencing oral health self-management behavior during the COVID-19 pandemic in Australia and evaluate whether this causal structure is congruent with existing health behavior theory.
Methods
Participants and procedure
For the purpose of this study, N = 565 online responses collected from the National Dental Telephone Interview Survey (NDTIS) 2021 Follow-up Questionnaire (between June 22, 2021, and May 13, 2022) were included. Participants were aged between 19 and 91 years (M = 54.50, SD = 16.16), the majority of which were female (60.9%), employed either full-time (37.65%) or part-time (22.02%), and had completed an undergraduate degree or higher (70.1%). The NDTIS 2021 was a national survey conducted by the Australian Research Centre for Population Oral Health (ARCPOH) that aimed to obtain information about the frequency of oral health problems among the Australian general population, as well as the psychosocial factors associated with oral health problems. These included the impact of the COVID-19 pandemic, socioeconomic position, quality of life, among others. NDTIS 2021 participants were randomly selected as a representative sample of Australian adults aged 18 years and over. Following completion of the primary survey (conducted either by telephone interview or online), participants were invited to respond to the follow-up questionnaire and given the option to provide their answers over the phone or by completing a paper or online version. The NDTIS 2021 was approved by the Human Research Ethics Committee at the The University of Adelaide (approval number H-2020–153). All participants provided verbal consent to participate in the survey, and datasets were de-identified to ensure anonymity.
Theoretical framework and the selection of variables
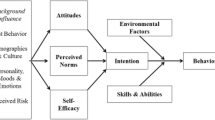
The theoretical framework applied to this study was grounded in Andersen’s (1995) Behavioral Model (ABM, see Fig. 2), which proposes that health behaviors, such as personal health practices and the use of health services, are influenced by both environmental factors (e.g., health care system and the external environment) and population characteristic factors (e.g., predisposing characteristics, enabling resources, and need). The ABM has been widely used in healthcare research and continues to be an important framework for understanding healthcare utilization patterns across populations and health conditions, including preventive dental visiting (Harris et al. 2017).
Andersen’s Behavioral Model (ABM). Adapted from “Revisiting the Behavioral Model and Access to Medical Care: Does it Matter?” by R. M. Andersen 1995, Journal of Health and Social Behavior, 36, p. 8. The model proposes causes between the environment, population characteristics, health behaviors, and outcomes
We identified six domains specific to the COVID-19 pandemic influencing oral health self-management behavior, each of which aligned with components of the ABM (i.e., external environment, enabling factors, and predisposing factors). Fear of COVID-19 disease was identified as the major external environmental factor impacting dental visitation during the pandemic, driven by concerns over infection risks in dental settings. In addition, fear and anxiety associated with the pandemic may have disrupted routines or led to increased stress levels, which can affect both oral hygiene habits and dental visitation negatively (Sari and Bilmez 2021). Three enabling factors, including accessibility to dental appointments, availability of transportation to dental appointments, and affordability of dental care (Beck et al. 2021; Burgette et al. 2021; Cook et al. 2020) were identified as possible barriers to oral health behaviors, potentially preventing individuals from seeking timely preventive or therapeutic oral health interventions. According to Cook et al. (2020), during the COVID-19 pandemic, Australians experienced limited access to both dental services and transportation due to restrictions imposed during lockdown periods, and were also more likely to be negatively affected by the high costs associated with dental care due to higher levels of unemployment. Finally, the ability to discuss oral health issues was identified as a predisposing factor, since openly discussing oral health concerns with peers, family members, and/or non-dental healthcare professionals can lead to increased awareness, motivation, and adherence to oral health self-management practices (Cohen et al. 2000).
Fear of COVID-19 Scale
Fear of COVID-19 disease was measured using three items from the Fear of COVID-19 Scale (Ahorsu et al. 2022). These included "I am most afraid of COVID-19" (Afr), "I am afraid of losing my life because of COVID-19" (Dth), and "I cannot sleep because I’m worried about getting COVID-19" (Ins). Participants responded on a five-point response Likert scale (1 = strongly disagree, 2 = disagree, 3 = neither disagree nor agree, 4 = agree and 5 = strongly agree). This scale displayed good internal consistency reliability (ω = 0.80).
Oral health impacts related to COVID-19
Oral health impacts related to COVID-19 were measured by asking participants the following: "During the COVID-19 pandemic, were you able to …” (a) “discuss your dental or oral health with non-dental professionals during the pandemic?” (Discuss), (b) “make an appointment with a dentist or oral health practitioner for any dental or oral health needs?" (Access), (c) “afford dental care?" (Afford), (d) “find transport required to attend for a dental appointment?" (Transp), and (e) “find the energy to manage your dental or oral health?” (OHSM). These oral health-specific survey items were responded to on a five-point response Likert scale (1 = unable to do so, 2 = with a lot of difficulty, 3 = with some difficulty, 4 = with a little bit of difficulty, and 5 = without difficulty). This scale also displayed good internal consistency reliability (ω = 0.82).
Statistical analysis
Software packages
All statistical analyses were conducted using R packages EGAnet (Golino and Christensen 2022), bnlearn (Scutari 2019), NCT (van Borkulo et al. 2022), lavaan (Rosseel 2012), and caret (Kuhn 2008).
Data preparation
All items measuring population characteristics were reverse scaled as they were written with a positive valence. For example, while the item “afford dental care?” was reverse scaled, the item “I am most afraid of COVID-19” was not, since it was written with the required negative valence. In this way, higher scores across all items indicated stronger negative impacts of the pandemic (being less able to afford dental care, stronger fear of COVID-19, etc.).
To understand the nature of missing data, missingness was first summarized by item and then demographic factors (i.e., sex, education achievement, and employment status). Complete cases made up 75% (426/565) of the observed data, with the remaining 15% (86/565) of cases missing one item, 2% (14/565) missing two items, 3% (18/565) missing three items, 2% (9/565) missing four items, and 2% (10/565) of cases missing five items. The item Discuss (“…discuss your dental or oral health with people other than a dentist?”) displayed a comparatively high level of missingness at 18% (103/565) and was more likely missing from older respondents (i.e., > 50 years) than from younger respondents (i.e., ≤ 50 years), χ2 (5) = 18.6, p = 0.002.
Because rates of item missingness were > 5% and found to be distributed non-randomly across demographic factors, missing values were imputed using a single imputation method, the “bagged-tree” model. In bagged tree imputation, for each variable with missing data, a tree model is trained based on all other variables in the set, including demographic variables, and then the missing values are imputed using a regression function. This robust imputation model has been shown to outperform other imputation methods (e.g., k-nearest-neighbor imputation and median imputation), as measured by root mean square error (RMSE) between imputed and true values. Following Kuhn and Johnson (2019), the bagged-tree imputation method was utilized with n = 25 trees. The imputation model included OHSM as the outcome variable and all other survey items as predictors.
Gaussian graphical model (GGM)
The GGM (also known as the undirected graphical model) was estimated under the assumption of Gaussian distributions and models the conditional associations between variables (Christensen et al. 2020). Due to the ordinal nature of item scales, the polychoric correlation matrix was used as input. The GGM was estimated across N = 10,000 non-parametric bootstrapped samples using the graphical least absolute shrinkage and selector operator (GLASSO) based on minimization of the extended Bayesian information criterion (see Epskamp and Fried 2018). This method estimates the typical network structure formed by the mean partial correlations across the bootstrap samples. The model fit was evaluated with the root mean squared error of approximation (RMSEA) and comparative fit index (CFI). Following Kline (2015), values of CFI ≥ 0.95 and RMSEA < 0.05 were used to indicate good model fit. Metric, network, and global invariance were assessed across two demographic groups: sex (males vs. females) and median age (younger ≤ 57 years vs. older > 57 years). Metric invariance was assessed by comparing the strength of item network loadings, while network and global strength invariance were assessed by comparing network edge weights and the absolute sum of network edge weights, respectively (van Borkulo et al. 2022). All comparisons were based on 1,000 permutations. To ensure correct identification of statistical differences, two types of p-values were examined: uncorrected and those corrected using the Benjamini–Hochberg procedure (Benjamini and Hochberg 1995). According to Jamison et al. (2022), if both types of p-values pointed to a network loading difference being statistically significant across groups, then that item is considered non-invariant.
Directed acyclic graphical (DAG) model
The DAG model was estimated by employing the PC-stable algorithm across N = 10,000 non-parametric bootstrap samples (following Colombo and Maathuis 2014). Only directed edges appearing in 70% of bootstrap samples (i.e., strength ratio ≥ 0.70) were included in the model, and the directionality of the edge was established according to the direction that was observed in more than 50% of samples (i.e., direction ratio ≥ 0.50) (as suggested by Briganti et al. 2022b). The structure of estimated DAG was then assessed against the theoretical structure described by Andersen’s Behavioral Model (ABM).
Structural equation modeling (SEM)
The SEM was specified by including the causal pathways present in the estimated DAG. Due to the non-normal distribution of the survey data, the specified SEM was estimated using a maximum likelihood estimation with robust standard errors and a Satorra–Bentler scaled test statistic. Robust incremental (CFI) and absolute (χ2, RMSEA) fit indices were calculated and assessed, with values of CFI ≥ 0.95 and RMSEA < 0.05 applied to indicate acceptable model fit (Kline 2015).
Results
Descriptive statistics
Participants were predominantly female (60.5%), aged between 19 and 91 years (M = 54.49, SD = 16.16), employed either full-time (37.7%) or part-time (22.0%), and had completed an undergraduate degree or higher (> level 5, Australian Qualifications Framework; 66.1%). The polychoric correlations, covariances, and distributions of the (imputed) survey items are summarized in Table 1.
Estimated GGM
The GGM estimated from the bootstrap samples is displayed in Fig. 3 (panel A), with nonzero edge weights also reported in Table 2. The GGM displayed an acceptable fit to the observed data (χ2 (8) = 32.1, p = .001, CFI = 0.99, RMSEA = 0.073, 95% CI = [0.48, 0.10], p = .060), thus providing an adequate representation of the structure of conditional associations between variables. Metric invariance across both sex and age held for all eight items (see Table 3). There were also no statistically significant differences observed between networks based on either sex (M = 0.206, p = .523 with S = 0.110, p = .645) or age (M = 0.280, p = .094 with S = 0.204, p = .374), suggesting that the relationships between all items in the GGM remained consistent across demographic groups.
Network models of COVID-19 impacts on oral health in Australia. (A) The average estimated bootstrapped (N = 10,000) Gaussian graphical model (GGM). (B) The estimated bootstrapped (N = 10,000) directed acyclic graph (DAG). (C). The DAG-specified structural equation model (SEM). Abbreviations: Appt = accessibility to dental appointments, Afford = affordability of dental care, Transp = availability of transportation to dental appointments, Discuss = ability to discuss oral health issues, Afr = most afraid of COVID-19, Dth = most afraid dying because of COVID-19, Ins = insomnia due to worry about getting COVID-19, OHSM = oral health self-management behavior
Estimated DAG
The estimated DAG is displayed in Fig. 3 (panel B), with strength ratios, direction ratios, and retention decisions for each directed path given in Table 2. All directed edges present within the DAG were present as edges in the GGM, providing further evidence that these edges might capture, even more than conditional associations, causal effects established between the variables. Generally, all pathways within the DAG conformed to those expected by ABM. That is, environmental factors (Afr, Ins, Dth) preceded population characteristic factors (Transp, Afford, Appt, Discuss), which in turn preceded behavior (OHSM).Footnote 2 Thus, the nodes associated with fear of COVID-19 (environmental factors) did not show a direct causal effect on oral health self-management behavior and were instead fully mediated by population characteristics. The DAG suggested three direct causes of OHSM—Appt, Afford, and Discuss—with Discuss also mediating the effects of Appt and Afford, and Appt mediating the effect of Afford.
Estimated SEM
The SEM was specified according to causal pathways present in the DAG. The estimated SEM model is displayed in Fig. 3 (panel C), with unstandardized and standardized beta coefficients and robust fit indices are given in Table 2. The strongest factor directly impacting OHSM was Discuss (β = 0.26), followed by Appt (β = 0.22) and Afford (β = 0.21). The model provided excellent fit to the data, χSB2 (13) = 19.2, p = .117, robust CFI = 0.994, robust RMSEA = 0.033, 95% CI = [0.00, 0.062], p = .804).
Discussion
Our study examined how factors like dental appointment availability, affordability, fear of COVID-19, and openness to discuss oral health influenced individual oral health behavior (oral health self-management) during the pandemic in Australia. We analyzed conditional associations between these variables, establishing their metric, network, and global strength invariance across sex and age. Our findings aligned with Andersen’s behavior model (ABM), showing that environmental factors preceded population characteristics, which in turn preceded health behaviors. For instance, heightened fear impacted conversation about oral health, affecting oral health self-management. The effect that environmental factors had on oral health behaviors during the COVID-19 pandemic in Australia was mediated by the population characteristics also present during the pandemic. That is, fear of COVID-19 did not directly cause people to increase their oral health behavior, such as regular tooth brushing, even although good oral hygiene practices are associated with reduced incidence rates and/or impacts of COVID-19 disease (Seale et al. 2020). Instead, fear of COVID-19 was mediated by the ability to afford dental care and the ability to make a dental appointment or discuss their oral health, worsening oral health self-management behaviors as a result. This is not surprising considering the crucial role that dental professionals, including dentists, dental hygienists, and dental therapists, play in providing oral health education and instruction. Yet during the pandemic, accessibility to dentists, dental hygienists, and dental therapists was tightly restricted, limiting opportunities for supportive interactions.
In light of these findings, consideration should be given to introducing new and innovative communication networks to support discussions surrounding oral health and oral health self-management. For example, while other hygiene measures, such as handwashing, were key components of the government campaigns to “flatten the curve” around the world (Seale et al. 2020), receiving the strongest messaging focus early in the pandemic (MacIntyre et al. 2021), it is surprising that oral hygeine messaging was also not a public health messaging priority. This is surprising since not only is the severity of COVID-19 disease reduced in people who do maintain good oral health (Kamel et al. 2021; Sampson et al. 2020), poor oral hygeine practices can also increase the spread of COVID-19 within households (González-Olmo et al. 2020). Indeed, the direct promotion of regular tooth-brushing habits is recommended as a cost-effective and practical means of improving overall health outcomes, with consistent oral hygiene practice being shown to reduce the incidence of respiratory infections (Mojon 2002), including COVID-19 (Sampson et al. 2020). Such promotional campaigns might be easily be incorporated to those promoting other forms of personal hygiene.
Limitations and further research
It should be noted that while the results provide evidence that support the theory that (1) appointment availability, (2) dental care affordability, and (3) inability to discuss oral health with people other than a dentist during COVID-19 are direct causes of poor oral health self- management, the causal effects discovered in an exploratory manner in our study need to be confirmed with other research methodologies and study designs, such as identification of such effects in longitudinal observational data and, whenever possible, across randomized controlled trials. There are several inherent limitations regarding the use of causal discovery algorithms (CDA) for the empirical identification of causal structures from the data. Firstly, because the fit of the GGM and SEM were evaluated on the same data on which the models were estimated, these model fits are likely to be inflated (Fokkema and Greiff 2017). Secondly, CDAs rely on several assumptions that are unrealistic in practice, such as causal sufficiency which requires that all confounders are measured and included in the causal structure (Eronen 2020). Another assumption is acyclicity, which requires that the graph does not contain cycles, so the causal structure may be represented as a DAG. In the real world, however, it is likely that causal structures include variables that mutually reinforce each other, violating the assumption of acyclicity (Briganti et al. 2022a). For example, on inspection of the DAG statistics for the item Discuss, the direction statistics for the links Discuss → OHSM is 54%, meaning that in 46% of the bootstrapped samples, the link OHSM → Discuss was inferred instead. That this relationship is indeed acyclic is assumed by the model, cyclicality cannot be ruled out, and should thus be further investigated.
Conclusion
Our findings offer empirical support to the theory that factors such as appointment availability, dental care affordability, and the opportunity to engage in oral health discussions with individuals other than dentists during the pandemic directly contributed to inadequate oral health self-care. It is important to note, however, that although consistent OHSM practices have been proven to reduce the occurrence of respiratory infections, including COVID-19, fear of the virus did not directly influence oral health self-care. In light of these findings, we recommend that discussions about OHSM outside the client–practitioner relationship should be encouraged within the community, especially where there are low levels of accessibility to oral healthcare appointments, to enhance overall population health outcomes. This may occur via consistent OHSM public health messaging alongside hand hygiene.
Availability of data and material
The datasets generated and/or analyzed during the current study are not publicly available. We do not have permission from the University of Adelaide Human Research Ethics Committee to publicly release the NDTIS 2021 dataset in either identifiable or de-identified form. The datasets and R syntax are available from the corresponding author upon reasonable request.
Notes
For a detailed discussion of orientation propagation rules and the PC algorithm, please refer to Glymour, C., Zhang, K., & Spirtes, P. (2019). Review of causal discovery methods based on graphical models. Frontiers in Genetics, 10, 524. https://doi.org/https://doi.org/10.3389/fgene.2019.00524.
Abbreviations: Appt = accessibility to dental appointments, Afford = affordability of dental care, Transp = availability of transportation to dental appointments, Discuss = ability to discuss oral health issues, Afr = most afraid of COVID-19, Dth = most afraid dying because of COVID-19, Ins = insomnia due to worry about getting COVID-19, OHSM = oral health self-management behavior.
References
Ahorsu DK, Lin C-Y, Imani V, Saffari M, Griffiths MD, Pakpour AH (2022) The fear of COVID-19 scale: development and initial validation. Int J Ment Heal Addict 20:1537–1545. https://doi.org/10.1007/s11469-020-00270-8
Andersen RM (1995) Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav 36(1):1–10. https://doi.org/10.2307/2137284
Beck MJ, Hensher DA, Nelson JD (2021) Public transport trends in Australia during the COVID-19 pandemic: an investigation of the influence of bio-security concerns on trip behaviour. J Transp Geogr 96:103167. https://doi.org/10.1016/j.jtrangeo.2021.103167
Benjamini Y, Hochberg Y (1995) Controlling the false discovery rate: a practical and powerful approach to multiple testing. J Roy Stat Soc: Ser B (methodol) 57(1):289–300
Borsboom D, Deserno MK, Rhemtulla M, Epskamp S, Fried EI, McNally RJ, Robinaugh DJ, Perugini M, Dalege J, Costantini G, Isvoranu AM, Wysocki AC, van Borkulo CD, van Bork R, Waldorp LJ (2021) Network analysis of multivariate data in psychological science. Nat Rev Methods Primers 1:1–58. https://doi.org/10.1038/s43586-021-00055-w
Briganti G, Decety J, Scutari M, McNally RJ, Linkowski P (2022) Using Bayesian networks to investigate psychological constructs: the case of empathy. Psychol Reports(Online ahead of print). https://doi.org/10.1177/00332941221146711
Briganti G, Scutari M, McNally RJ (2022) A tutorial on bayesian networks for psychopathology researchers. Psychol Methods 28(4):947–961. https://doi.org/10.1037/met0000479
Burgette JM, Weyant RJ, Ettinger AK, Miller E, Ray KN (2021) What is the association between income loss during the COVID-19 pandemic and children’s dental care? J Am Dent Assoc 152(5):369–376. https://doi.org/10.1016/j.adaj.2021.02.001
Cărămidă M, Dumitrache MA, Țâncu AMC, Ilici RR, Ilinca R, Sfeatcu R (2022) Oral habits during the lockdown from the SARS-CoV-2 pandemic in the Romanian population. Medicina 58(3):387. https://doi.org/10.3390/medicina58030387
Christensen AP, Golino H, Silvia PJ (2020) A psychometric network perspective on the validity and validation of personality trait questionnaires. Eur J Pers 34(6):1095–1108. https://doi.org/10.1002/per.2265
Cohen SM, Fiske J, Newton JT (2000) The impact of dental anxiety on daily living. Br Dent J 189(7):385–390. https://doi.org/10.1038/sj.bdj.4800777
Colombo D, Maathuis MH (2014) Order-independent constraint-based causal structure learning. J Machine Learn Res 15(1):3741–3782. https://doi.org/10.48550/arXiv.1211.3295
Cook MJ, Dri GG, Logan P, Tan JB, Flahault A (2020) COVID-19 down under: Australia’s initial pandemic experience. Int J Environ Res Public Health 17(23):8939. https://doi.org/10.3390/ijerph17238939
Coulthard P, Thomson P, Dave M, Coulthard FP, Seoudi N, Hill M (2020) The COVID-19 pandemic and dentistry: the clinical, legal and economic consequences-part 2: Consequences of withholding dental care. Br Dent J 229(12):801–805. https://doi.org/10.1038/s41415-020-2406-9
Epskamp S, Fried EI (2018) A tutorial on regularized partial correlation networks. Psychol Methods 23(4). https://doi.org/10.1037/met0000167
Eronen MI (2020) Causal discovery and the problem of psychological interventions. New Ideas Psychol 59:100785. https://doi.org/10.1016/j.newideapsych.2020.100785
Fokkema M, Greiff S (2017) How Performing PCA and CFA on the same data equals trouble. Eur J Psychol Assess 33(6):399–402. https://doi.org/10.1027/1015-5759/a000460
Glymour C, Zhang K, Spirtes P (2019) Review of causal discovery methods based on graphical models. Front Genet 10:524. https://doi.org/10.3389/fgene.2019.00524
Golino HF, Christensen AP (2022) EGAnet: exploratory graph analysis: a framework for estimating the number of dimensions in multivariate data using network psychometrics. R package version 1.1.1. [Online]
González-Olmo MJ, Delgado-Ramos B, Ruiz-Guillén A, Romero-Maroto M, Carrillo-Díaz M (2020) Oral hygiene habits and possible transmission of COVID-19 among cohabitants. BMC Oral Health 20(1):286. https://doi.org/10.1186/s12903-020-01274-5
Harris RV, Pennington A, Whitehead M (2017) Preventive dental visiting: a critical interpretive synthesis of theory explaining how inequalities arise. Commun Dent Oral Epidemiol 45(2):120–134. https://doi.org/10.1111/cdoe.12268
Hernán MA, Robins JM (2006) Instruments for causal inference: an epidemiologist’s dream? Epidemiology 17(4):360–372. https://doi.org/10.1097/01.ede.0000222409.00878.37
Hopcraft M, Farmer G (2021) Impact of COVID-19 on the provision of paediatric dental care: analysis of the Australian child dental benefits schedule. Commun Dent Oral Epidemiol 49(4):369–376. https://doi.org/10.1111/cdoe.12611
Jamison L, Golino H, Christensen AP (2022) Metric invariance in exploratory graph analysis via permutation testing. [Pre-print]. https://doi.org/10.31234/osf.io/j4rx9
Kamel AHM, Basuoni A, Salem ZA, AbuBakr N (2021) The impact of oral health status on COVID-19 severity, recovery period and C-reactive protein values. British Dental J(Online ahead of print), 1–7. https://doi.org/10.1038/s41415-021-2656-1
Keyes K, Galea S (2017) The limits of risk factors revisited: is it time for a causal architecture approach? Epidemiology 28(1):1–5. https://doi.org/10.1097/EDE.0000000000000578
Kline RB (2015) Principles and practice of structural equation modeling. Guilford publications
Kuhn M, Johnson K (2019) Feature engineering and selection: a practical approach for predictive models. Taylor & Francis Group.https://doi.org/10.1080/00031305.2020.1790217
Kuhn M (2008) Building predictive models in R using the caret package. J Stat Software 28(5):1–26. https://doi.org/10.18637/jss.v028.i05
MacIntyre CR, Nguyen P-Y, Chughtai AA, Trent M, Gerber B, Steinhofel K, Seale H (2021) Mask use, risk-mitigation behaviours and pandemic fatigue during the COVID-19 pandemic in five cities in Australia, the UK and USA: a cross-sectional survey. Int J Infect Dis 106:199–207. https://doi.org/10.1016/j.ijid.2021.03.056
McNally RJ, Mair P, Mugno B, Riemann B (2017) Co-morbid obsessive–compulsive disorder and depression: a Bayesian network approach. Psychol Med 47(7):1204–1214. https://doi.org/10.1017/S0033291716003287
Mojon P (2002) Oral health and respiratory infection. J Canadian Dental Assoc 68(6):340–345. https://citeseerx.ist.psu.edu/document?repid=rep1&type=pdf&doi=db25898716cdd594cee46bbdefaf7821a449469a
Peloso R-M, Pinzan A (2021) Does the use of face masks during the COVID-19 pandemic impact on oral hygiene habits, oral conditions, reasons to seek dental care and esthetic concerns? J Clin Exp Dent 13(4):e369. https://doi.org/10.4317/jced.57798
Rosseel Y (2012) An R package for structural equation modeling. J Stat Software 48(2):1–36. https://doi.org/10.18637/jss.v048.i02
Ryan O, Bringmann LF, Schuurman NK (2022a) The challenge of generating causal hypotheses using network models. Struct Equ Modeling 29(6):1–18. https://doi.org/10.1080/10705511.2022.2056039
Ryan O, Bringmann LF, Schuurman NK (2022b) The challenge of generating causal hypotheses using network models. Struct Equ Model 29(6):953–970
Sampson V, Kamona N, Sampson A (2020) Could there be a link between oral hygiene and the severity of SARS-CoV-2 infections? Br Dent J 228(12):971–975. https://doi.org/10.1038/s41415-020-1747-8
Sari A, Bilmez Z (2021) Effects of Coronavirus (COVID-19) fear on oral health status. Oral Health Prev Dent 19(1):411–423. https://doi.org/10.3290/j.ohpd.b1870377
Scutari M, Graafland CE, Gutiérrez JM (2019) Who learns better Bayesian network structures: accuracy and speed of structure learning algorithms. Int J Approximate Reason 115:235–253. https://doi.org/10.1016/j.ijar.2019.10.003
Scutari M (2019) Bayesian network constraint-based structure learning algorithms: parallel and optimized implementations in the bnlearn R package. J Stat Software 77(2):1–20. https://doi.org/10.18637/jss.v077.i02
Seale H, Dyer CEF, Abdi I, Rahman KM, Sun Y, Qureshi MO, Dowell-Day A, Sward J, Islam MS (2020) Improving the impact of non-pharmaceutical interventions during COVID-19: examining the factors that influence engagement and the impact on individuals. BMC Infect Dis 20(1):607. https://doi.org/10.1186/s12879-020-05340-9
van Borkulo CD, van Bork R, Boschloo L, Kossakowski JJ, Tio P, Schoevers RA, Borsboom D, Waldorp LJ (2022) Comparing network structures on three aspects: a permutation test. Psychological Methods.https://doi.org/10.1037/met0000476
VanderWeele TJ (2012) Invited commentary: structural equation models and epidemiologic analysis. Am J Epidemiol 176(7):608–612. https://doi.org/10.1093/aje/kws213
Zhou J, Zhou J, Feng L, Feng Y, Xiao L, ChenX, Yang J, Wang G (2022) The associations between depressive symptoms, functional impairment, and quality of life, in patients with major depression: undirected and Bayesian network analyses. Psychol Med 1–13. https://doi.org/10.1017/S0033291722003385
Acknowledgements
We would like to extend our thanks to the curator of these data, Mr. Sergio Chrisopoulos, for his support during this project. Mr. Chrisopoulos is supported by the University of Adelaide.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions This study was supported by the grant Strategic Research Support Scheme received by the Faculty of Health and Medical Sciences, The University of Adelaide. Data used in this study were collected in partnership with the Australian Department of Health.
Author information
Authors and Affiliations
Contributions
Conceptualization: Kym M. McCormick, Pedro Henrique Ribeiro Santiago; Software: Kym M. McCormick; Methodology: Kym M. McCormick, Pedro Henrique Ribeiro Santiago; Formal analysis: Kym M. McCormick; Writing – Original Draft: Kym M. McCormick; Visualization: Kym M. McCormick; Writing – Review & Editing: Pedro Henrique Ribeiro Santiago, Lisa Jamieson; Supervision: Lisa Jamieson; Project administration: Lisa Jamieson; Funding acquisition: Lisa Jamieson.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The NDTIS 2021 was approved by the Human Research Ethics Committee at the University of Adelaide (approval number H-2020–153). All participants provided verbal consent to participate in the survey and datasets were de-identified to ensure anonymity.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
McCormick, K.M., Ribeiro Santiago, P.H. & Jamieson, L. The impact of COVID-19 on the oral health self-care practices of Australian adults. J Public Health (Berl.) (2024). https://doi.org/10.1007/s10389-024-02287-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10389-024-02287-y