Abstract
Aim
Occupational exposures may harm the health of pregnant workers and their future children. While Switzerland has established specific regulations to safeguard pregnant employees while enabling them to pursue their job, there are limitations in implementing these provisions. This study aims to evaluate the contribution of an occupational medicine consultation (PregOH-consultation) in protecting pregnant workers and facilitating their safe return to work. Pregnant employees were referred to the consultation by their attending physicians in need of support in applying pregnancy protective legislation.
Subject and methods
Between 2015 and 2021, indicators were collected from pregnant workers who sought the consultation, as well as from their employers. Descriptive and correlational statistical analyses were performed.
Results
Out of the 328 work situations analysed, 98% presented at least one occupational hazard. Among the 272 companies contacted, only 14% had conducted a risk analysis, and 39% had implemented job adaptations. Among the pregnant workers whose employers were involved in the PregOH-consultation, 44% were able to return to work safely. Early referral to the consultation and pre-existing preventive measures within the company were identified as potential predictors of successul of the consultation in terms of safe return to work. The impact of the consultation was found to be less pronounced for women of foreign nationality.
Conclusion
The observed companies have insufficient measures in place to adequately protect pregnant employees, potentially jeopardizing their health or leading to premature job withdrawal. The PregOH-consultation serves as an effective intervention by facilitating hazard identification and enabling pregnant workers to safely continue their employment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Occupational risks and their impact on pregnant workers
Pregnancy induces physical, social, and emotional changes, which may increase pregnant women’s vulnerability to specific working conditions. Occupational exposure or activities, such as chemical products, microorganisms, carrying heavy loads, and prolonged standing hours, may harm pregnant workers’ health as well as their future children (e.g. preeclampsia, preterm birth, stillbirth, and birth defects) (Cai et al. 2019; Fowler and Culpepper 2021; Spinder et al. 2020). These hazards are prevalent across numerous occupational sectors, encompassing healthcare, education (particularly in settings involving young children), industry-related fields, and retail services, among others (Fowler and Culpepper 2021).
Studies have reported elevated rates of sick leaves among pregnant workers (Backhausen et al. 2018; Melsom 2014). Part of these sick leaves during pregnancy are not prescribed exclusively for medical reasons but are often used to relieve pregnant workers from strenuous work activities and occupational exposures (Abderhalden-Zellweger et al. 2020; Rudin et al. 2018). Indeed, several studies show a positive association between occupational exposures, arduous working conditions, and an increased rate of sick leave during pregnancy (Pedersen et al. 2020; Rudin et al. 2018). According to a recent narrative review, the absences or interruptions of work among pregnant employees can be attributed to various interlaced factors (Brunner et al. 2023). These include health status, sociodemographic factors, attitudes of healthcare providers, as well as national context and offer of social benefits and insurance. Furthermore, work-related characteristics, such as exposure to risks, heavy lifting, and night shifts, are strong predictors of work absences during pregnancy (Brunner et al. 2023). Nevertheless, research has also demonstrated that pregnant employees may benefit from protective measures in the workplace. Implementing interventions aimed at limiting or prohibiting exposure to factors such as vibration, shift-work schedules, night shifts, prolonged standing, and heavy lifting can effectively reduce adverse maternal and perinatal outcomes, including preterm birth and small-for-gestational-age deliveries (Croteau et al. 2006, 2007). Moreover, these measures have been shown to mitigate sick leave among pregnant workers (Henrotin et al. 2017; Kristensen et al. 2008).
Maternity protection legislation and shortcomings in its implementation
The protection of women from workplace exposures during pregnancy and maternity is an important concern for public international law. In order to protect pregnant women’s and their future children’s health, the International Labor Organization (ILO) (C183—Maternity Protection Convention 2000) requires an assessment of occupational hazards to pregnancy and the implementation of the necessary protective measures to face these risks. This should be done by eliminating risky exposures or by adapting working conditions, such as limiting working time to limit exposure, modifying the type of task, or providing the necessary equipment so as to reduce biomechanical or physical constraints and stopping the use of dangerous chemical substances. If this is not possible, employees must be reassigned to another job or, as a last resort, they have the right to benefit from a paid preventive leave. Consistent with the ILO’s provisions, in 2001, Switzerland introduced a specific regulation to protect pregnant workers’ health while enabling them to pursue their job (Maternity Protection Ordinance 2001). The Swiss Maternity Protection Ordinance (hereafter OProMa) requires that pregnant worker health and ability to work are assessed by their attending physician (mostly their gynaecologist-obstetrician (OB-GYN)). To make that assessment, OB-GYNs should rely on a risk analysis (RA) performed beforehand in the patient's company by an occupational physician or another qualified occupational safety specialist. If the RA is incomplete or absent, or if the protective measures recommended by this analysis (i.e. job adjustments or reassignment) are not implemented, the OB-GYN should prescribe a preventive leave certificate as a precautionary measure. Preventive leave is financed by the employer and represents at least 80% of the woman’s salary. It differs from sick leave which implies a disease or a pregnancy-related complication, and which is usually financed by the employer’s loss of income insurance.
Implementation of maternity protection legislation faces several limitations, both among companies and healthcare professionals (COWI 2015; Probst et al. 2018). At the company level, several factors can influence the implementation of protective measures for pregnant workers, such as the employers' knowledge of legal provisions (Lembrechts and Valgaeren 2010), the awareness and acknowledgement of the presence of hazards in certain occupational activities (Malenfant 2009), the company characteristics (e.g. size, presence of a trade union, presence of an occupational health unit) (Lembrechts and Valgaeren 2010; Rudin et al. 2018), and the additional organizational burdens generated by the implementation of protective measures (Adams et al. 2016). A study carried out in French-speaking Switzerland shows a poor application of protective measures: only 12% of employees in healthcare companies and 2% in food industry companies benefit from a protection in accordance with the Swiss legislation (Abderhalden-Zellweger et al. 2021). Some studies speculated that employers may prefer pregnant workers to be put on sick leave by their general practitioner, in order to employ another “healthy” candidate instead, rather than adjusting work conditions (Melsom 2014).
In national contexts where OB-GYNs are involved in safeguarding pregnant workers, studies indicate that the OB-GYNs may not always feel equipped to assess the hazardous nature and suitability of working conditions for their patients (Grajewski et al. 2016; Larsson et al. 2006). For instance, findings from a national online survey conducted among members of the American Congress of Obstetricians and Gynecologists show that 50% of respondents rarely (less than 20% of the time) inquire about the environmental health history (including occupational health) of their pregnant patient (Stotland et al. 2014). Additionally, three focus groups involving obstetricians in this same study shed light on the main barriers they face, including insufficient knowledge and understanding of occupational risks during pregnancy, uncertainty regarding the extent to which environmental exposures can impact maternal and neonatal outcomes, and challenges in discussing occupational risks due to concerns about job loss and economic hardships for their patients (Stotland et al. 2014). These results are consistent with a study interviewing OB-GYNs working in French-speaking Switzerland, in which they underlined challenges they encounter in assessing their patients' ability to work (Abderhalden-Zellweger et al. 2020).
Occupational health consultation for pregnant workers
Since 2015, the Department of Occupational and Environmental Health (DSTE) of Unisanté in the French-speaking part of Switzerland has developed a specialized occupational medicine consultation for pregnant employees (PregOH-consultation). OB-GYNs can refer complex cases to the PregOH-consultation if they suspect a potential hazardous occupational exposure for a pregnant worker, they require assistance in applying pregnancy protective legislation, and the patient’s company does not have its own occupational health specialist.
The PregOH-consultation is carried out by an occupational health physician (OHP) and encompasses the following key elements: (1) providing support and guidance to the OB-GYN, who ultimately determines whether the pregnant worker can safely continue her employment; (2) identifying potential risky exposures through an anamnesis of the patient’s job; (3) informing the pregnant employee about her rights and other available resources, such as labour inspection services; and (4) advising the employer about their legal obligations and assisting them in conducting a risk assessment (RA) and implementing necessary workplace adjustments. Figure 1 summarizes the main steps of the consultation.
Study aims
To the best of our knowledge, no studies have focused on the impact of interventions such as occupational medicine consultation on the safe return to work for pregnant employees. It remains uncertain whether these interventions can effectively promote a safe transition back to the workplace for expectant employees. In light of this research gap, we aim to assess the impact of the PregOH-consultation on the safe return to work for pregnant employees, within the context of the Swiss legislative framework. Additionally, we aim to identify potential predictors of success or failure of the PregOH-consultation in terms of enabling a safe return to work. Furthermore, we intend to assess the evolution of the consultation's impact and its associated predictors of success over the course of the study period. By undertaking this investigation, we endeavour to provide valuable insights into the efficacy of the consultation and its potential in supporting pregnant women as they resume work under appropriate and secure conditions.
Methods
Data collection
Data were collected from January 2015 to December 2021, based on indicators systematically gathered by OHPs at the end of each consultation and through discussions with the designated contact person within the patient's company. The indicators were defined based on the authors' clinical expertise and encompassed various aspects related to the patient's health status, sociodemographic characteristics, and work-related factors. This included factors such as age, gestational weeks, employment status, industry sectors, and exposure to hazardous occupational conditions. Additionally, discussions with the company's contact person provided information on their awareness and knowledge of the OProMa and on the presence of maternity protective measures within the organization.
The form used to collect the indicators is available in Supplementary Information 1. All collected indicators were anonymized and recorded in an Excel file. Rigorous checks and verifications were conducted to ensure the consistency and accuracy of the collected data. It is important to note that the form for collecting the indicators underwent revisions over the course of the study period, resulting in a few instances of missing data. Supplementary Information 2 provides a comprehensive description of each collected indicator, and highlights the most significant changes that occurred between 2015 and 2021.
Study population
Pregnant workers who were referred by their OB-GYNs seeking guidance on the application of pregnancy protective legislation were included in the analysis. Unemployed, self-employed, and pregnant women working in agriculture were excluded from the analysis, as they are not subject to Switzerland’s Maternity Protection Ordinance (Secrétariat d'Etat à l'Economie [SECO] 2016).
In cases where pregnant women held multiple jobs, the OHP completed a separate form for each workstation. Each job was treated as a distinct situation and included in the analysis.
During the consultations, OHPs systematically asked pregnant employees for their consent to contact their company (e.g. the employer, the human resource manager).
Data analysis
To evaluate the contribution of the PregOH-consultation in facilitating a safe return to work, a composite variable was created to indicate whether the pregnant employees' workstations were deemed safe by OHPs at the first, second, or third advisory session (see Fig. 1). This main outcome—i.e. the return to work of the pregnant employee under safe conditions as assessed by the OHP—was considered to represent the success of the PregOH-consultation. This variable was generated by only considering occupational situations in which the company was contacted.
Relevant indicators, which may be associated with the PregOH-consultation success (e.g. the number of risky exposures encountered by women in their workplace, the presence of preventive maternity protective measures within the company) were tested as predictors of the success of the consultation in terms of safe return to work for the pregnant employees.
Since the development of the PregOH-consultation in 2015, the Swiss context has evolved towards better provision of information for the parties involved in maternity protection. In particular, the State Secretariat for Economic Affairs (SECO) has published three information brochures, each targeting the relevant stakeholders outlined in the OProMa (employers, attending physicians, and pregnant workers). In addition, the Department of Occupational and Environmental Health (DSTE) in French-speaking Switzerland provides training programs for health professionals and business actors interested in maternity protection at work. Furthermore, the outbreak of the COVID-19 pandemic has had a significant impact on maternity protection, as new protective measures and job reorganization have been necessary to reduce the transmission of the virus. Considering these factors, the impact of the PregOH-consultation in terms of return to work under safe conditions was assessed across three distinct periods: between 2015 and 2016 (preliminary data from the first 2 years of the consultationFootnote 1), between 2017 and 2019 (release of the SECO’s information brochures for the different stakeholders involved in the OProMa), and between 2020 and 2021 (COVID-19 pandemic). The evolution through the years of the relevant indicators who tested to be significantly associated to the impact of the PregOH-consultation in terms of safe return to work were also assessed.
All analyses were conducted using Stata 17 software. Descriptive statistics and correlational analyses (Fisher's test: p = 0.05) were performed on a selected set of indicators collected during the PregOH-consultation.
Ethical considerations
The Human Research Ethics Committee of the Canton Vaud (CER-VD) certified that the research study protocol associated with this study falls outside of the field of application of the Swiss Federal Act on Research Involving Humans (Req-2020–01320).
The participation in the study was voluntary. All participating pregnant workers were informed about the research objectives, the confidentiality standards regarding the use of the data, and signed a consent form at the end of the PregOH-consultation.
Results
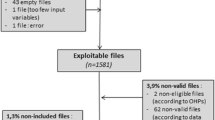
Between January 2015 and December 2021, 328 working situations (involving 313 patients) were analysed through the PregOH-consultation (Fig. 2).
Characteristics of the study population
Women who came to the PregOH-consultation had an average age of 29.8 years. They were referred to the consultation on average around the 21st week of amenorrhea (i.e. at the end of the fifth month of pregnancy) (Table 1). Concerning the education level, 29% of women had no post-compulsory education, while 42% had completed secondary education (i.e. vocational education and training, or general education which covers programs leading to the baccalaureate). Most of the women (59%) were of foreign nationality.
Characteristics of the work situations
Table 2 presents the characteristics of the work situations analysed through the PregOH-consultation (N = 328).
Nearly all the work situations (98%) involved at least one occupational hazard, as defined by the OProMa (art. 5-16, 2001) or the Swiss Employment Act (EmpA) (art. 35-35b 1964). Furthermore, 93% involved multiple exposures, ranging from two to seven occupational hazards per work situation. The most common exposures were movements, awkward postures, and shocks (92%), handling heavy loads (85%), standing for long periods (80%), exposure to chemicals (59%), and the absence of breaks or a designated place to rest (59%).
At the time of the consultation, the OB-GYNs had issued sick leave certificates (partial or total) for 36% of the work situations, and preventive leave certificates for 33% of the work situations. For 31% of the work situations, the employees were still at their workstation at their usual work rate. The OHPs estimate that 59% of the sick leave certificates were related to the working conditions of the patients.
Contact with the company and existing preventive measures before the consultation
With the workers' agreement, OHPs contacted 272 (83%) companies (Table 3). According to the estimation of the OHP, in 40% of cases, the contact person in the company had no knowledge of the OProMa. A minority of companies (14%) reported having conducted a RA. Furthermore, 30% of these companies did not submit their RA despite the OHP's request. Out of the submitted RA (n = 26), only 31% were deemed compliant by the OHP. Thirty-nine percent of the companies stated that some work adjustments, such as job adaptations or transfers, had been implemented prior to the consultation. Most of these adjustments were made by the employer themselves (90%), while only 8% were made based on a formal RA.
Contribution of the consultation in terms of pregnant employees’ return to work under safe conditions
It should be noted that only work situations in which the OHP was able to contact the company were included in the analysis. Data reveal that 44% (n = 121) of the work situations were judged to be safe for pregnant employees as a result of the PregOH-consultation (Fig. 3).
Possible predictors of success of the PregOH-consultation
Table 4 presents the possible predictors of success (or failure) of the PregOH-consultation in terms of safe return to work for pregnant employees.
Early referral to the PregOH-consultation, specifically between the first and third month of pregnancy, significantly increases the likelihood of a safe return to work (p = 0.000).
Pregnant workers with Swiss nationality demonstrate a significantly higher rate of returning to work under safe conditions (p = 0.000).
While not statistically significant, the impact of the PregOH-consultation appears to be less pronounced for women employed in occupational categories with lower levels of qualification, according to the ISCO-08 classification. For instance, only 33% of women working in level 9 were able to safely return to work, compared to 56% of women working in level 2. Similarly, the impact of PregOH-consultation is lower for workers facing multiple occupational exposures, with only 37% of women exposed to more than five hazards achieving a safe return to work, compared to 46% of those exposed to a single hazard.
These three variables (i.e. nationality, level of occupational qualification, and number of occupational exposures) appear to be related to each other. Indeed, in the study population, foreign-nationality workers are more likely to be employed in low-skilled occupations (45% work in elementary occupations compared to 4% of Swiss women, data not shown), and face a significantly higher prevalence of multiple occupational hazards (p = 0.007, data not shown).
When OHP considered that the contact person within the company had complete knowledge of the OProMa, pregnant workers were more likely to benefit from the PregOH-consultation in terms of a safe return to work (p = 0.002). Finally, women employed in companies where work adjustments and a risk assessment (RA) were performed prior to the consultation had a higher likelihood of safely returning to work (p = 0.000 and p = 0.000, respectively).
Evolution of the impact of the consultation and of its possible predictors of success
The impact of PregOH-consultation in terms of safe return to work remained relatively stable over the years, with minimal variation observed (Table 5).
Between 2020 and 2021, there was a significant increase in the proportion of pregnant workers referred early to the consultation, occurring between the first and third month of pregnancy. This figure rose to 40% compared to 21% in the period of 2017–2019 and 29% in 2015–2016 (p = 0.046).
Over the years, the work situations of the women who came for the consultation are more often characterized by multiple occupational exposures (p = 0.001).
Discussion
The study aimed to assess the impact of the PregOH-consultation and identify predictors of success regarding the safe return to work for pregnant women. It also addresses critical points that can enhance the provision of care and may have implications for other countries grappling with the issue of work retention during pregnancy. Some of the findings from this study indeed have relevance beyond the borders of Switzerland.
Contribution of the PregOH-consultation and its possible predictors of success
Our results provide evidence supporting the effectiveness of the PregOH-consultation in facilitating the reconciliation of work and pregnancy by enabling a safe return to work for a significant proportion of women who benefitted from the consultation. The PregOH-consultation also serves as a valuable resource for employers, who can benefit from specialized advice and support on maternity protection provisions while ensuring the retention of valuable human resources within their companies. A qualitative study conducted in Danish public hospitals shows that managers feel that healthcare professionals often signed off pregnant employees without exploring alternative solutions to keep them employed (Backhausen et al. 2021). A better understanding of the role of OHPs in this process is crucial to prevent unnecessary sick leaves (Backhausen et al. 2021). In the Swiss economic landscape, which is predominantly composed of small- and medium-sized companies (99% with fewer than 250 full-time equivalents) (Federal Statistical Office 2019b), the presence of in-house occupational health units is limited within companies. Consequently, specialized occupational medicine consultations such as the one analysed in this study can help address this gap in national contexts where only a few companies have their own occupational health units. Moreover, when the companies were contacted and actions were undertaken by OHPs as a result of the consultation, certain women were able to return to work safely within 3–6 months after the consultation. It is important to consider strategies for organizing and maintaining effective long-term follow-up pertaining to maternity protection and occupational health in general.
The data collected in this study allowed for the identification of potential predictors of the consultation success in terms of safe return to work for pregnant employees.
-
1.
Early referral to the PregOH-consultation. When workers are referred to the consultation before three months of pregnancy, a higher proportion of them were able to return to work under safe conditions. However, we observed that, on average, workers were referred to the consultation towards the end of the fifth month of pregnancy, which raises concerns on multiple fronts. Firstly, this delayed referral means that workers are exposed for several months to occupational hazards that are dangerous fo their health and that of their future child, most often without protective measures being taken and without their workstation having been adequately assessed through a RA. It is important to note that early identification of occupational hazards that can impact reproductive health, including pre-conception exposures, is crucial for minimizing the adverse effects of certain exposures (such as chemicals and biological agents) on pregnancy outcomes and child health and development (Messerlian et al. 2022). Secondly, as pregnancy is a limited period of time, the late referral to the consultation often prevents the implementation of the necessary protective measures due to lack of time. These observations underscore the importance of raising awareness among health professionals who can refer their patients to the PregOH consultation, about the benefits of this consultation, and the importance of acting as early as possible. While it is encouraging to observe that workers have been referred to the PregOH-consultation earlier over the years, it is crucial to recognize that work interruptions can still occur at any time. This can happen either due to inadequate protective measures during the course of pregnancy or due to the occurrence of intercurrent diseases.
-
2.
Employers’ knowledge of maternity protection legislation and the presence of preventive measures within the company. The knowledge of the contact person in the company regarding the OProMa, the presence of an RA, and prior implementation of workplace adjustments were predictive factors for the success of the PregOH consultation in terms of safe return to work for pregnant employees. The implementation of preventive measures serves not only to ensure immediate protection upon pregnancy announcement but also to minimize disorganization within the company. It is therefore essential to enhance companies' awareness of their rights and responsibilities, emphasizing the importance of proactively implementing maternity protective measures. Studies in other national contexts report a lack of knowledge or recognition of occupational exposures faced by pregnant workers among employers. For instance, research conducted in Scandinavian countries has revealed a low level of job adjustments for pregnant employees (Stafne et al. 2019), indicating insufficient efforts and attention from employers towards the working conditions of pregnant women (Backhausen et al. 2021). The focus groups conducted by Andersen et al. (2022) revealed that pregnant women consider managers' concern, understanding, and recognition of their needs in relation to challenging working conditions as a key factor predicting a positive and successful experience of workplace adjustments. A randomized trial study conducted in Denmark (Begtrup et al. 2021) indicated that short educational interventions targeting managers alone are inadequate in reducing occupational risks, improving the psychosocial work environment, promoting the well-being of pregnant employees, or reducing absences during pregnancy. These findings emphasize the importance of not only increasing employers' knowledge and understanding of maternity protection legislation but also fostering a proactive and institutional approach to implement preventive measures in workplaces.
-
3.
Nationality of the women. For workers of foreign nationality, the impact of the consultation in terms of safely returning to work is more limited compared Swiss workers. This finding can be partially attributed to the higher likelihood of foreign workers being employed in low-skilled jobs and being exposed to multiple occupational hazards. Existing literature indicates that employees of foreign nationality are over-represented in hazardous industries and occupations, such as in manual jobs, which carry higher risks (Premji et al. 2010; Sterud et al. 2018). These workers not only face greater physical and psychosocial risks but also have reduced access to healthcare services (Aktas et al. 2022). In Switzerland, women of foreign nationality are overexposed to physical risks (39% of women of Swiss nationality vs 64.3% for women from South-Western Europe, 60.6% for women from South-Eastern and Eastern Europe, and 57.5% for women outside Europe) (Federal Statistical Office 2019a). A systematic review and meta-analysis (Hargreaves et al. 2019) highlight that migrant workers are exposed to significant risks of occupational illness and injury. The authors further conclude that the specific needs of migrant populations in occupational settings are largely neglected in research and public policies (Hargreaves et al. 2019). In addition to greater exposure to occupational hazards, negative attitudes and stereotypes towards foreign workers may contribute to their poorer integration within companies, resulting in less attention and willingness to adapt to working conditions. Finally, given that the quality of patient–doctor interaction (e.g. communication, partnership) may be hindered by ethnic differences (Cooper et al. 2006) and linguistic difficulties, further studies should investigate whether interactions between foreign-nationality pregnant workers and OHPs during the PregOH-consultation are affected by implicit factors (e.g. misunderstandings) that impede the consultation's impact on safe return to work. Addressing these issues of inequality requires a broader paradigm in occupational health research that encompasses social, economic, and cultural determinants of health (Flynn et al. 2022). A study conducted in the United States reveals a similar phenomenon concerning the utilization of paid maternity leave (Hawkins 2020). Substantial disparities in the use of maternity leave were observed based on occupation, race/ethnicity, and education. Younger, Black, and Hispanic mothers, as well as those with fewer years of education, were less likely to utilize paid maternity leave (Hawkins 2020). Moreover, even after adjusting for occupation, racial/ethnic differences in the utilization of paid maternity leave persisted (Hawkins 2020). Further research should explore these factors in greater detail to gain a comprehensive understanding of the interplay between sociodemographic factors, maternity protective measures, and the effectiveness of consultations in promoting safe return to work.
Literature shows that larger companies are usually more inclined to implement maternity protective measures (e.g. job adjustments, RA) (Abderhalden-Zellweger et al. 2021; Adams et al. 2016; Rudin et al. 2018). However, contrary to expectations, the size of the company did not significantly influence the impact of the PregOH-consultation in terms of ensuring a safe return to work for pregnant employees. This finding could be explained by (1) the negative selection bias of the study population, which may participate to erase the differences according to company size identified in the literature. Indeed, only particularly complex work situations and for which it was not possible to refer the pregnant worker to the in-house company's occupational health unit were referred to the PregOH-consultation; and (2) larger companies, having more resources and flexibility, could more easily accept that the pregnant worker stays at home via the preventive leave certificate and pay her 80% of her salary.
Evolution of the impact of the PregOH-consultation and of its predictors of success
The impact of PregOH-consultation on the safe return to work for pregnant employees has shown limited variation over the years. This may be attributed to the fact that several factors identified as predictors of the success of the consultation (Table 4) (i.e. the contact person's knowledge of the OProMa, existing work adjustments and RA, and the nationality of the pregnant workers who came for consultation), do not differ significantly over the years (Table 5). Furthermore, other factors may have had an adverse effect on the return to work for pregnant workers. For example, during the COVID-19 pandemic, the implementation of additional protective measures was required, and exceptional financial compensation measures for companies emerged, which may have hindered the pregnant women’s return to work. Additionally, considering the documented negative impact of the Sars-Cov-2 virus on pregnant women and their newborns (Simbar et al. 2023; Villar et al. 2021), OB-GYNs may have opted more often to issue sick leave certificates as a precautionary measure. It is worth noting that, over the years, workers referred to the consultation have been significantly more exposed to multiple occupational risks. Multiple exposures may complicate the implementation of workplace adjustments and hamper the pregnant workers’ return to work under safe conditions. These findings align with recent data from the Swiss health survey, which indicates an upward trend in multiple workplace exposures among female workers (e.g. the proportion of women exposed to ≥ 3 occupational physical hazards rose from 33.2% in 2007 to 42.2% in 2017) (Federal Statistical Office 2019a).
Lastly, it is essential to acknowledge that Switzerland, like many other European countries, faces a significant shortage of occupational health professionals (Danuser 2014; The European Trade Union Institute’s [ETUI] 2014). This scarcity of resources poses challenges in further developing and expanding such consultations, even to other regions within Switzerland.
Strengths and limitations
This study provides valuable insights into the positive impact of specialized occupational medicine consultations on protecting and facilitating the safe return to work for pregnant employees, offering a potential avenue for enhancing maternity protection in Switzerland.
However, there are certain limitations to consider. Firstly, the number of women referred to the consultation remains relatively small compared to the annual birth rate in Western Switzerland. This limited sample size hinders the generalizability of the findings. Secondly, the study population consists of workers referred to the PregOH-consultation by their OB-GYNs, who typically face complex work situations. This negative selection bias might account for the higher proportion of women exposed to multiple occupational risks compared to data collected by the Swiss health survey (Federal Statistical Office 2019a). Furthermore, the exclusion from our study of self-employed and pregnant women working in agriculture who are not subject to the OProMa overlooks the unique challenges and occupational hazards faced by these groups, potentially affecting the effectiveness of the PregOH-consultation. Due to limited sample sizes in certain variable categories, multiple variable analyses were not feasible, limiting the ability to explore comprehensive relationships among variables. Finally, the absence of a control group in the study precludes making conclusive claims about the specific contribution of the PregOH-consultation compared to alternative approaches. These limitations should be taken into account when interpreting the findings of this study, and future research should strive to address these limitations to provide a more comprehensive understanding of the impact of specialized occupational medicine consultations for pregnant workers.
Conclusion
The PregOH-consultation demonstrates significant benefits in identifying occupational hazards for pregnant employees and facilitating their safe return to work. It is crucial to support the development of this consultation and explore opportunities to extend its availability to other regions in Switzerland. Additionally, the findings of our study raise important considerations for improving care provisions not only in Switzerland but also in other national contexts where implementing occupational medicine consultations for pregnant workers is being considered.
-
1.
Raising awareness among healthcare professionals about the existence and the positive impact of such consultations is vital to encourage early referrals of pregnant workers and promote timely access to necessary support and interventions.
-
2.
Stakeholders within the company play a crucial role in the success of the consultation. Having a strong grasp of the legislation governing maternity protection at work and the implementation of preventive measures are essential factors contributing to positive outcomes of the consultation.
-
3.
Special attention is needed for pregnant women of foreign nationality working in low-skilled jobs, as the effectiveness of the consultation in ensuring a safe return to work for this population appears to be lower. Addressing the specific challenges faced by these populations, such as language barriers, limited access to healthcare services, and disparities in social benefits like paid maternity leave is crucial to promote equity and improve occupational health for all workers.
-
4.
Considering that a significant proportion of work situations are deemed safe by occupational health professionals after 3–6 months from the consultation, it is important to explore effective strategies for long-term monitoring.
A mixed-method study on the experience and perspectives of users (employees, OB-GYNs, companies) and their views on the PregOH-consultation has been finalized (unpublished work). This study will help to address their needs and insights to further enhance care provisions and optimize the consultation process.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
Notes
Preliminary results of the first 2 years of the consultation and details regarding the PregOH-consultation are presented elsewhere (Krief et al. 2022).
References
Abderhalden-Zellweger A, Probst I, Politis Mercier MP, Danuser B, Wild P, & Krief P (2020) Implementation of maternity protection legislation: gynecologists’ perceptions and practices in French-speaking Switzerland. PloS one 15(4). https://doi.org/10.1371/journal.pone.0231858
Abderhalden-Zellweger A, Probst I, Politis Mercier MP, Zenoni M, Wild P, Danuser B, & Krief P (2021) Implementation of the Swiss Ordinance on Maternity Protection at Work in companies in French-speaking Switzerland. WORK: J Prev Assess Rehab 69(1):157–172. https://doi.org/10.3233/WOR-213465
Adams L, Winterbotham M, Oldfield K, McLeish J, Stuart A, Large A, Murphy L, Rossiter H, Selner S (2016) Pregnancy and maternity-related discrimination and disadvantage: experiences of employers. Department for Business, Innovation and Skills and the Equality and Human Rights Commission. www.gov.uk/bis. Accessed 18 Jan 2024
Aktas E, Bergbom B, Godderis L, Kreshpaj B, Marinov M, Mates D, McElvenny DM, Mehlum IS, Milenkova V, Nena E, Glass DC (2022) Migrant workers occupational health research: an OMEGA-NET working group position paper. Int Arch Occup Environ Health 95:765–777. https://doi.org/10.1007/s00420-021-01803-x
Andersen DR, Momsen AH, Pedersen P, Damkjaer Maimburg R (2022) Reflections on workplace adjustments for pregnant employees: a qualitative study of the experiences of pregnant employees and their managers. BMC Preg Childbirth 22(1):456. https://doi.org/10.1186/s12884-022-04749-1
Backhausen M, Damm P, Bendix J, Tabor A, Hegaard H (2018) The prevalence of sick leave: Reasons and associated predictors - A survey among employed pregnant women. Sex Reprod Healthc 15:54–61. https://doi.org/10.1016/j.srhc.2017.11.005
Backhausen MG, Iversen ML, Skold MB, Thomsen TG, Begtrup LM (2021) Experiences managing pregnant hospital staff members using an active management policy-A qualitative study. PloS one 16(2). ARTNe024754710.1371/journal.pone.0247547
Begtrup LM, Brauer C, Jensen JH, Tottenborg SS, Flachs EM, Hammer PEC, Malmros PA, Bonde JPE (2021) Impact of a manager-oriented intervention on occupational exposures and well-being among pregnant hospital and day-care employees: A cluster randomised trial. Scandinavian J Public Health 51(2):188–196. https://doi.org/10.1177/14034948211018387
Brunner L, Krief P, Probst I, Abderhalden-Zellweger A, Renteria SC, Vonlanthen J, & Moschetti K (2023) A narrative review on factors associated with job interruption during pregnancy. Int J Occup Med Environ Health 36(3). https://doi.org/10.13075/ijomeh.1896.02132
C183 - Maternity Protection Convention (2000) International Labour Organization (ILO) Retrieved from https://www.ilo.org/dyn/normlex/fr/f?p=NORMLEXPUB:12100:0::NO::P12100_INSTRUMENT_ID:312328. Accessed 18 Jan 2024
Cai C, Vandermeer B, Khurana R, Nerenberg K, Featherstone R, Sebastianski M, Davenport MH (2019) The impact of occupational activities during pregnancy on pregnancy outcomes: a systematic review and meta-analysis. Am J Obstet Gynecol. https://doi.org/10.1016/j.ajog.2019.08.059
Cooper LA, Beach MC, Johnson RL, Inui TS (2006) Delving below the surface - Understanding how race and ethnicity influence relationships in health care. J Gen Intern Med 21:S21–S27. https://doi.org/10.1111/j.1525-1497.2006.00305.x
COWI (2015) Evaluation of the Practical Implementation of the EU Occupational Safety and Health (OSH) Directives in EU Member States. Report by directive: directive 92/85/EEC on the introduction of measures to encourage improvements in the safety and health of work of pregnant workers and workers who have recently given birth or are breastfeeding (pregnant/breastfeeding workers directive) (DG employment, social affairs and inclusion). https://ec.europa.eu/social/BlobServlet?docId=16897&langId=en. Accessed 18 Jan 2024
Croteau A, Marcoux S, Brisson C (2006) Work activity in pregnancy, preventive measures, and the risk of delivering a small-for-gestational-age infant. Am J Public Health 96(5):846–855. https://doi.org/10.2105/ajph.2004.058552
Croteau A, Marcoux S, Brisson C (2007) Work activity in pregnancy, preventive measures, and the risk of preterm delivery. Am J Epidemiol 166(8):951–965. https://doi.org/10.1093/aje/kwm171
Danuser B (2014) Comment soigner la santé au travail ? REISO. https://www.reiso.org/articles/themes/travail/277-comment-soigner-la-sante-au-travail. Accessed 18 Jan 2024
Employment Act (EmpA) (1964) Retrieved from https://www.admin.ch/opc/fr/classified-compilation/19640049/index.html#a2. Accessed 18 Jan 2024
Federal Statistical Office (2019a) Conditions de travail et état de santé, 2012–2017. Enquête suisse sur la santé (ESS). https://www.bfs.admin.ch/bfs/fr/home/statistiques/sante/enquetes/sgb.assetdetail.9366233.html. Accessed 18 Jan 2024
Federal Statistical Office (2019b) Petites et moyennes entreprises. https://www.bfs.admin.ch/bfs/fr/home/statistiques/industrie-services/entreprises-emplois/structure-economie-entreprises/pme.html. Accessed 18 Jan 2024
Flynn MA, Check P, Steege AL, Siven JM, Syron LN (2022) Health Equity and a Paradigm Shift in Occupational Safety and Health. Int J Environ Res Public Health 19(1). ARTN34910.3390/ijerph19010349
Fowler JR, Culpepper L (2021) Working during pregnancy. UpToDate. https://www.uptodate.com/contents/working-during-pregnancy. Accessed 18 Jan 2024
Grajewski B, Rocheleau CM, Lawson CC, Johnson CY (2016) “Will my work affect my pregnancy?” Resources for anticipating and answering patients’ questions. Am J Obstet Gynecol 214(5):597–602. https://doi.org/10.1016/j.ajog.2016.03.005
Hargreaves S, Rustage K, Nellums LB, McAlpine A, Pocock N, Devakumar D, Aldridge RW, Abubakar I, Kristensen KL, Himmels JW, Friedland JS, Zimmerman C (2019) Occupational health outcomes among international migrant workers: a systematic review and meta-analysis. Lancet Glob Health 7(7):E872–E882. https://doi.org/10.1016/S2214-109x(19)30204-9
Hawkins D (2020) Disparities in the usage of maternity leave according to occupation, race/ethnicity, and education. Am J Ind Med 63(12):1134–1144. https://doi.org/10.1002/ajim.23188
Henrotin JB, Vaissiere M, Etaix M, Dziurla M, Malard S, Lafon D (2017) Exposure to occupational hazards for pregnancy and sick leave in pregnant workers: a cross-sectional study. Annals Occup Environ Med 29. https://doi.org/10.1186/s40557-017-0170-3
Krief P, Mediouni Z, Abderhalden-Zellweger A, Ker D, Seraj N, Renteria SC, Vonlanthen J, Danuser B (2022) Evaluation of a pilot consultation for maternity protection at work in Switzerland. Swiss Medical Weekly 152:w30160(23). https://doi.org/10.4414/smw.2022.w30160
Kristensen P, Nordhagen R, Wergeland E, Bjerkedal T (2008) Job adjustment and absence from work in mid-pregnancy in the Norwegian Mother and Child Cohort Study (MoBa). Occup Environ Med 65(8), 560–566. https://oem.bmj.com/content/oemed/65/8/560.full.pdf. Accessed 18 Jan 2024
Larsson C, Sydsjo A, Alexanderson K, Sydsjo G (2006) Obstetricians' attitudes and opinions on sickness absence and benefits during pregnancy. Acta Obstet Gynecol Scand 85(2):165–170. https://www.ncbi.nlm.nih.gov/pubmed/16532909. Accessed 18 Jan 2024
Lembrechts L, Valgaeren E (2010) Grossesse au travail. Le vécu et les obstacles rencontrés par les travailleuses en Belgique. Etude quantitative et qualitative. Institut pour l’égalité des femmes et des hommes. https://igvm-iefh.belgium.be/sites/default/files/downloads/40%20-%20Grossesse%20au%20travail_FR.pdf. Accessed 18 Jan 2024
Malenfant R (2009) Risk, Control and Gender: Reconciling Production and Reproduction in the Risk Society. Organ Stud 30(2–3):205–226. https://doi.org/10.1177/0170840608101477
Maternity Protection Ordinance (2001) Retrieved from https://www.admin.ch/opc/fr/classified-compilation/20002241/index.html. Accessed 18 Jan 2024
Melsom AM (2014) Long-term sickness absence during pregnancy and the gender balance of workplaces. Scand J Public Health 42(7):627–634. https://doi.org/10.1177/1403494814541596
Messerlian C, Zhang Y, Sun Y, Wang Y, Mustieles V (2022) An ounce of prevention is worth a pound of cure: time to focus on preconception workplace reproductive health. Hum Reprod 37(1):1–4. https://doi.org/10.1093/humrep/deab263
Pedersen P, Momsen AMH, Andersen DR, Nielsen CV, Nohr EA, Maimburg RD (2020) Associations between work environment, health status and sick leave among pregnant employees. Scandinavian J Public Health 49(2):149–158. https://doi.org/10.1177/1403494820919564
Premji S, Duguay P, Messing K, Lippel K (2010) Are Immigrants, Ethnic and Linguistic Minorities Over-Represented in Jobs With a High Level of Compensated Risk? Results From a Montreal, Canada Study Using Census and Workers’ Compensation Data. Am J Ind Med 53(9):875–885. https://doi.org/10.1002/ajim.20845
Probst I, Zellweger A, Politis Mercier MP, Danuser B, Krief P (2018) Implementation, mechanisms, and effects of maternity protection legislation: a realist narrative review of the literature. Int Arch Occup Environ Health 91(8):901–922. https://doi.org/10.1007/s00420-018-1339-y
Rudin M, Stutz H, Bischof S, Jäggi J, Bannwart L (2018) Erwerbsunterbrüche vor der Geburt. Bern Bundesamt für Sozialversicherungen (BSV) Retrieved from https://www.bsv.admin.ch/bsv/home.webcode.html?webcode=C814.C165.de. Accessed 18 Jan 2024
Secrétariat d'Etat à l'Economie (SECO) (2016) Maternité: Protection des travailleuses. Berne Retrieved from https://www.seco.admin.ch/seco/fr/home/Publikationen_Dienstleistungen/Publikationen_und_Formulare/Arbeit/Arbeitsbedingungen/Broschuren/mutterschaft-_-schutz-der-arbeitnehmerinnen.html. Accessed 18 Jan 2024
Simbar M, Nazarpour S, Sheidaei A (2023) Evaluation of pregnancy outcomes in mothers with COVID-19 infection: a systematic review and meta-analysis. J Obstet Gynaecol 43(1):2162867. https://doi.org/10.1080/01443615.2022.2162867
Spinder N, Almli LM, Desrosiers TA, Arnold KE, Bergman JEH, Kromhout H, Boezen HM, de Walle HEK, Rocheleau C, Reefhuis J (2020) Maternal occupational exposure to solvents and gastroschisis in offspring - National Birth Defects Prevention Study 1997–2011. Occup Environ Med 77(3):172–178. https://doi.org/10.1136/oemed-2019-106147
Stafne SN, Vollestad NK, Morkved S, Salvesen KA, Stendal Robinson H (2019) Impact of job adjustment, pain location and exercise on sick leave due to lumbopelvic pain in pregnancy: a longitudinal study. Scand J Prim Health Care 37(2):218–226. https://doi.org/10.1080/02813432.2019.1608058
Sterud T, Tynes T, Mehlum IS, Veiersted KB, Bergbom B, Airila A, Johansson B, Brendler-Lindqvist M, Hviid K, Flyvholm MA (2018) A systematic review of working conditions and occupational health among immigrants in Europe and Canada. BMC Public Health 18. ARTN77010.1186/s12889-018-5703-3
Stotland NE, Sutton P, Trowbridge J, Atchley DS, Conry J, Trasande L, Gerbert B, Charlesworth A, Woodruff TJ (2014) Counseling patients on preventing prenatal environmental exposures–a mixed-methods study of obstetricians. PLoS ONE 9(6):e98771. https://doi.org/10.1371/journal.pone.0098771
The European Trade Union Institute’s (ETUI) (2014) Occupational health services in need of emergency care. Health and safety at work magazine (10). https://www.etui.org/sites/default/files/Hesamag_10_EN_1.pdf. Accessed 18 Jan 2024
Villar J, Ariff S, Gunier RB, Thiruvengadam R, Rauch S, Kholin A, Roggero P, Prefumo F, do Vale MS, Cardona-Perez JA, Maiz N, Cetin I, Savasi V, Deruelle P, Easter SR, Sichitiu J, Soto Conti CP, Ernawati E, Mhatre M, . . . Papageorghiou AT (2021) Maternal and Neonatal Morbidity and Mortality Among Pregnant Women With and Without COVID-19 Infection: The INTERCOVID Multinational Cohort Study. JAMA Pediatr 175(8), 817-826. https://doi.org/10.1001/jamapediatrics.2021.1050
Acknowledgements
We would like to thank the participating women and companies agreeing to sharing their experiences, which made this study possible. We gratefully thank all the OHPs leading the consultations and supporting this research. We would also like to thank the research assistants who entered the collected data. Finally, we would like to thank the research team that conducted the first study analysing the preliminary data of the first 2 years of the consultation.
Funding
Open access funding provided by University of Lausanne This work was supported by the Commission de promotion de la santé et de lutte contre les addictions, Direction Générale de la Santé du canton de Vaud.
Author information
Authors and Affiliations
Contributions
Alessia Abderhalden-Zellweger: Methodology, Investigation, Formal analysis, Data curation, Original draft preparation, Reviewing and Editing; Julien Vonlanthen: Methodology, Investigation, Data curation, Reviewing and Editing; Saira-Christine Renteria: Methodology, Reviewing and Editing; Pascal Wild: Methodology, Validation, Reviewing and Editing; Karine Moschetti: Methodology, Reviewing and Editing; Loïc Brunner: Methodology, Reviewing and Editing; Zakia Médiouni: Methodology, Reviewing and Editing; Isabelle Probst: Conceptualization, Methodology, Supervision, Reviewing and Editing, Funding acquisition; Peggy Krief: Conceptualization, Methodology, Supervision, Reviewing and Editing, Project administration, Funding acquisition.
Corresponding author
Ethics declarations
Ethics approval
The Human Research Ethics Committee of the Canton Vaud (CER-VD) certified that the research study protocol associated with this study falls outside of the field of application of the Swiss Federal Act on Research Involving Humans (Req-2020–01320).
Consent to participate
The participation in the study was voluntary. All participating pregnant workers were informed about the research objectives, the confidentiality standards regarding the use of the data, and signed a consent form at the end of the PregOH-consultation.
Consent for publication
All participating pregnant workers were informed about the research objectives, the confidentiality standards regarding the use of the data, and signed a consent form at the end of the PregOH-consultation.
Competing interests
PKR and ZME are among the OHPs performing the PregOH-consultation. However, no personal financial benefits are involved.
The authors have no competing interests to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Probst I and Krief P are co-last authors.
Supplementary Information
Below is the link to the electronic supplementary material.
10389_2023_2190_MOESM1_ESM.docx
Supplementary file1 Translated version in English of the form used by OHPs to collect the indicators during the PregOH-consultation and the discussions with the designated contact person within the patient's company(DOCX 54 KB)
10389_2023_2190_MOESM2_ESM.docx
Supplementary file2 Description of the collected indicator and of the most significant changes that occurred between 2015 and 2021(DOCX 41 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abderhalden-Zellweger, A., Vonlanthen, J., Renteria, SC. et al. Enhancing maternity protection at work: assessing the contribution of a specialized occupational medicine consultation for pregnant employees in Switzerland. J Public Health (Berl.) (2024). https://doi.org/10.1007/s10389-023-02190-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10389-023-02190-y