Abstract
Aim
SCI may cause loss of sensory function, paralysis, and limited functional mobility. The specificity of SCI has expanded the scope of medical trials and given rise to therapeutic options that incorporate new technologies with robotics and electronic devices. We aimed to identify various therapeutic options and develop effective treatment regimens.
Methods
We conducted the systematic review using the following digital databases: MEDLINE/PubMed and Google Scholar. We focused on publications published between 2012 and 2023 and The following primary terms were searched: “Spinal cord injury rehabilitation,” “Spinal cord injury exercise,” and “Spinal cord injury therapy,” with the Boolean operator “AND/OR” used for additional searches. A total of 110 relevant articles were identified during the selection process. After screening and assessing eligibility, the final 17 studies were included in this systematic review
Results & conclusion
The current paper gave a taxonomy of electrical instrumentation and traditional rehabilitation technologies. We also discovered that FES is used as a comprehensive regimen that involves both the upper and lower extremities, and that locomotor training using robots is beneficial in improving walking ability. We discovered that diversified training programs using conventional methods concentrated on the physical independence of patients with chronic SCI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spinal cord injury (SCI) is a catastrophic disease that causes decreased aerobic capacity, glucose intolerance, and insulin resistance due to autonomic dysfunction, physical inactivity, and significant deconditioning (Gorgey et al. 2014). In addition, several individuals with SCI are significantly less active due to wheelchair dependency, and these metabolic changes tend to lead to cardiovascular diseases (Warburton et al. 2007). The negative effects experienced by patients with SCI have led researchers to study the need for physical rehabilitation in these patients. Therefore, substantial progress has been made in SCI treatment (Eng et al. 2007). Therapies for SCI, such as drug, radiotherapy, diet, and rehabilitation therapies, can be approached in various ways. Proper rehabilitation based on injury severity plays an important role in building joints and preventing muscle strength loss. From a metabolic perspective, treatment is also thought to be important for maintaining smooth functioning of the respiratory and digestive systems (Nas et al. 2015). Over the past few decades, several studies have shown that clinical intervention and rehabilitation have a positive effect on physical and functional recovery in patients with SCI. However, significant progress on SCI treatment should be made considering that there are no practical and conclusive alternative treatments to SCI. A previous study has adopted various approaches; however, this sporadic accumulation is not a practical measure. Little empirical data support the efficacy of the multiple specialized therapies offered in SCI (Whiteneck et al. 2009). In addition, rehabilitation comes in several shapes and forms, and there are different approaches depending on the patient’s condition, such as paralysis (e.g., tetraplegia, paraplegia). The specificity of SCI has expanded the scope of medical trials and given rise to therapeutic options that incorporate new technologies with robotics and electronic devices. Although these attempts have been positive catalysts for addressing the chronic problems of SCI, specific protocols and their outcomes are not well documented. As a result, we attempted to systematically analyze the protocols and effects of rehabilitation to provide knowledge on which methods work efficiently in practice. This study aimed to comprehensively evaluate the equipment and methods used for SCI rehabilitation. Through a systematic review, the current paper presents comprehensive data on interventions provided by all therapy professionals and adds to the result-driven criteria for medical decision-making by organizing research designs (i.e., purpose, participant and exercise descriptions, and results).
Methods
Search strategy and data resource
This systematic review implemented the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. From April 2023 to May 2023, a systematic search of relevant papers was conducted using the following digital databases: MEDLINE/PubMed and Google Scholar. We focused on publications published between 2012 and 2023 and included only articles on humans written in English. The search was narrowed to include only full-text clinical trial articles. The following primary terms were searched: “Spinal cord injury rehabilitation,” “Spinal cord injury exercise,” and “Spinal cord injury therapy,” with the Boolean operator “AND/OR” used for additional searches.
Selection criteria
The following criteria for eligibility were created in accordance with the Population, Intervention, Comparison, Outcomes, and Study strategy: (1) Population (P): Individuals with an SCI (except where an individual without disabilities acts as an individual with disabilities); (2) Intervention (I): Rehabilitation, exercise, and/or physical treatment for SCI; (3) Comparison (C): No rehabilitation or other interventions; (4) Outcomes (O): Results of intervention in terms of functional improvement and treatment effectiveness (e.g., pain reduction, gait performance, body composition, and treatment effectiveness); and (5) Study (S): Controlled medical trials and protocols. In addition, the studies included randomized clinical trials, controlled clinical trials, observational studies, and case studies. Meta-analyses, reviews, letters, and proceedings were excluded.
Data synthesis and extraction process
This systematic review collected papers in accordance with the PRISMA 2020 guidelines, and three independent examiners were engaged in the study selection and extraction procedure. Subsequently, two authors inspected and evaluated the results. Finally, the researchers and reviewers reached a consensus on the selection and extraction process. In the identification process, a search engine in a scientific database was used to identify papers by combining keywords. Duplicated and irrelevant papers were excluded from the collected papers after searching. In the screening step, articles that did not meet the criteria were eliminated from the analysis list by screening titles and abstracts. Studies that did not include individuals with SCI were also excluded. Next, to verify the eligibility of the selected articles, each researcher reviewed the entire article and excluded articles. Studies with ambiguity were selected or excluded through discussions between the researchers and evaluators.
Assessment of quality of studies
The Physiotherapy Evidence Database (PEDro) was used to verify the quality of the collected articles. The PEDro scale is used to grade the methodology-related “quality” of each medical trial in the PEDro database. The PEDro scale is intended to assist users of the PEDro database in quickly determining which randomized clinical trials are likely to be valid internally and may have adequate statistical data to make the findings comprehensible (Sherrington et al. 2000). It consists of the following 11 items: eligibility standard, random and concealed allocation, group similarity at baseline, blinding, < 15% dropout, intention-to-treat analysis, between-group statistical comparisons, and variability. Each item contributes 1 point to the total PEDro score, except for the first item (Maher et al. 2003). The PEDro scores of the current study are provided in Appendix 1.
Results
Identification of studies
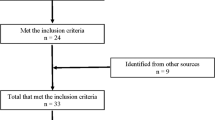
A total of 110 relevant articles were identified during the selection process. Fifteen duplicated records and 17 irrelevant topics were removed. After screening and assessing eligibility, the final 17 studies were included in this systematic review. A flow diagram of the selection process is shown in Fig. 1.
General overview
Articles related to the rehabilitation of patients with SCI were collected according to the criteria mentioned above, and 17 papers were derived. To precisely analyze exercise protocols, 12 electronic- and robot-based papers and 5 conventional types of rehabilitation articles were classified. This was examined by dividing the number of study participants by average age, duration of injury (years), level of injury (C1–T12), exercise design, research purpose, assessment, and results. The table of research results is presented in Table 1.
Robotic- and electronic-based rehabilitation
Twelve publications discussed electronic and robotic therapies for the survivors of SCI. For the systematic analysis, rehabilitation devices and methods were classified into functional electronic stimulation (FES) and robotic and locomotor training (LT).
Functional electrical stimulation rehabilitation
Six articles [1, 2, 3, 4, 5, 6] employed FES rehabilitation using rowing, cycling, and ergometers. FES rowing training (FESRT) was covered in four studies [1, 2, 3, 5]. Afshari et al. (2022) [1] assessed the effects of FESRT on the body composition profiles in the subacute phase of SCI. This clinical trial involved a hybrid exercise involving the upper and lower limbs, which required more muscular activity. Following a substantial increase in total and leg lean mass (p < 0.05), FESRT contributed to a greater exercise ability and a propensity for reduced body fat accumulation. Vivodtzev et al. (2020) [2] instructed patients with high-level SCI (T3–C4) to undergo a whole-body FES rowing protocol with noninvasive ventilation. After 3 months of training, the participants showed an improvement in their capacity to take up oxygen for certain ventilations. Chou et al. (2020) [3] and Kim et al. (2014) [5] employed rowing exercise interventions in the survivors of SCI. This protocol led to improvements in the patients’ motor function and body composition. Gorgey et al. (2019) [4] and Thrasher et al. (2013) [6] focused on the lower extremities using FES cycling and ergometry. Gorgey et al. (2019) [4] confirmed that FES lower limb cycling had positive effects on cardiometabolic results and aerobic fitness. Similarly, Thrasher et al. (2013) [6] designed FES leg cycle ergometry training to compare patients with incomplete and complete SCI. Following 40 exercise sessions, the researchers noted improvements in the power output of the lower extremities and fatigue test.
Robotic and locomotor training
Of the selected articles, six studies [7, 8, 9, 10, 11, 12] used LT as a rehabilitation program for patients with SCI. Onushko et al. (2019) [7] attempted to determine how sympathetic–somatomotor (SS) coupling in individuals with incomplete SCI (iSCI) can be affected by high- and low-intensity LT. In their study, the participants performed stepping tasks during 20 sessions for 4–6 weeks. The researchers discovered that high-intensity training might outperform low-intensity training, indicating that SS coordination in individuals with iSCI may change depending on the intensity of the intervention. Similarly, Leech et al. (2016) [8] evaluated the effects of exercise intensity on walking function and quality. They also found that high-intensity LT resulted in more favorable outcomes in terms of gait speed and muscle activity than low-intensity LT. Leech and George (2017) [9] employed a high-intensity LT program in patients with iSCI and noted that physical indicators (e.g., serum brain-derived neurotrophic factor, insulin-like growth factor-1) were enhanced following the intervention. Consequently, both studies reported that higher LT intensities were associated with greater improvements in patients with iSCI. Martinez et al. (2018) [10] also revealed that a body weight-supported treadmill using Lokomat® (Hocoma) improved locomotor function, including the motor score of the lower limb and balance. Gorman et al. (2019) [11] also used Lokomat® to assess and compare cardiorespiratory effects. The initial robotic session lasted 20 min and was subsequently extended in 5-min increments in future sessions until the exercise lasted 45 min. Each session began with a 5-min warm-up, followed by personalized, trained gait exercises, and finished with a 5-min cool-down. Peak VO2 level measured using robotic treadmill ergometry statistically improved (14.7%, p = 0.03) during the period of the robotic intervention. In a study by Francisco et al. (2017) [12], 10 individuals with chronic cervical SCI underwent robot-assisted arm training. They performed single-degree-of-freedom upper limb exercises to demonstrate the feasibility, tolerance, and efficacy of MAHI Exo-II for cervical SCI. This device is an electronically operated upper extremity haptic exoskeleton appliance developed for rehabilitation. The treatments were modified based on the movement ability of each joint. After robotic intervention, arm and hand functions (Jebsen-Taylor Hand Function Test, Action Research Arm Test) were improved. In addition, it was found that both trainings using robots improved the targeted physical function.
Conventional rehabilitation
Based on the abovementioned criteria, traditional rehabilitation methods for patients with SCI are categorized into resistance training, balance task, aerobic exercise, and mixed training. Five articles [13, 14, 15, 16, 17] were used for the systematic analysis. The table of research results is presented in Table 2.
Resistance training
Silva et al. (2020) [13] studied the effects of circuit resistance training (CRT) in individuals with SCI. The participants consisted of patients with chronic SCI, primarily those with injury levels from T4 to T11. CRT protocols involved physical and motor abilities (e.g., frontal lift, agility station, biceps curl). The interventions consisted of activities that were easy for patients to follow in their daily routine and could be performed directly in a wheelchair. After 12 weeks of exercise, although there were no differences in bone-related indicators, the patients’ muscle strength (p = 0.028) and agility (p = 0.028) improved.
Balance training
Sadeghi et al. (2018) [14] used rebound therapy for spinal cord rehabilitation. This intervention involves exercising on a trampoline to improve static stability. The participants performed core stability training and upper extremity exercises on a trampoline and several basic exercises using instruments, such as balls and balloons. After the participants practiced the exercises thrice a week, rebound therapy was found to have a positive effect on several standing stability parameters (p < .01).
Aerobic training
Aerobic training for patients with SCI has been addressed in studies by Wouda et al. (2016) [15] and DiPiro et al. (2016) [16]. Wouda et al. (2016) [15] aimed to determine whether high-intensity interval training (HIIT) increases physical capacity and fitness levels more than moderate-intensity training (MIT) and standard care. The two experimental groups were trained for 12 weeks at intensities of 70% (MIT) and 85–95% (HIIT) of HRmax. The intervention program consisted of jogging or running according to the patient’s fitness level and physical condition. The results showed no differences in effectiveness among the three groups (i.e., HITT, MIT, and standard care). DiPiro et al. (2016) [16] also used an aerobic exercise training (AET) program for iSCI. Ten patients were instructed to perform a non-task-specific, voluntary, progressive AET protocol. The researchers discovered significant improvements in aerobic and locomotor capacities.
Mixed training
Lotter et al. (2020) [17] identified the effects of task-specific therapies compared with impairment-based therapies on gait performance. Impairment-based training includes non-walking training, whereas the task-specific method involves training involving rehabilitation approaches (e.g., strengthening, balance, and aerobic exercise). Weight machines were used for the strengthening activities. During balance training, patients performed standing or sitting activities on unbalanced surfaces (e.g., foam, trampoline) or dual upper limb balance tasks. Aerobic exercise involved cycling or stepping (e.g., NuStep LLC). The protocol consisted of 20 sessions over 6 weeks, with the intensity set at 70–80% HRmax. The researchers found that task-specific training had a positive effect on the determinants of mobility capacity.
Discussion
This systematic review included 17 articles that examined the effects of various physical rehabilitation protocols on SCI. Six FES papers, six articles related to robotic training and LT, and five publications on traditional treatment modalities were analyzed and categorized. Based on our analysis of the technology and protocols of rehabilitation, we described how previous studies have applied physical rehabilitation for SCI and their rehabilitative features and results. Several researchers have adopted and developed electromechanical technologies for clinical trials. Among these methods, FES, which utilizes short electrical impulses to produce movements in the paralyzed muscle, is the most frequently employed approach for increasing motor skills in patients (Lynch and Popovic 2008). These treatments use the undamaged neuromuscular system to provide various therapeutic exercise alternatives, facilitate functional rehabilitation, and manage or prevent complications (Ho et al. 2014). Increasing the level of physical activity is crucial for individuals with SCI, whose physical activity has been significantly reduced, and electrical stimulation can maximize this. FES is applied in various ways, including rowing, cycling, and ergometry (Gorgey et al. 2019). The studies analyzed in this review also employed FES rowing [1, 2, 3, 5] and FES cycling [4, 6]. In terms of rehabilitation protocols, the duration of the exercises ranged from 30 min to 3 h, and the duration ranged from 3 months to 6 months. This was mainly conducted with the observation and assistance of therapists, and the intensity was set after monitoring the subjects’ exercise levels through a test. In addition, four studies [1, 2, 4, 6] included acclimation sessions to electrical stimulation before the full intervention. This adaptation process appears to be a necessary step in the rehabilitation of FES in patients with SCI. External factors, such as unfamiliarity with the intervention and nervousness, may have a negative effect on an individual’s initial performance on a specific measure (Awad et al. 2013). Various tests and acclimation training make it easier for participants to adapt to new stimuli and increase the reliability of the results. The FES publications that we analyzed primarily investigated biological responses after FES rehabilitation and showed improvements in metabolic factors. Body composition [1, 4, 5], cardiorespiratory function [1, 2, 4, 6], and neural factors [3] showed positive outcomes. FES rehabilitation tended to emphasize the movements and effects of the entire body rather than focusing on a single extremity [1, 2, 3]. Davis et al. (2008) and Duffell et al. (2010) also suggested that although the initial goal of FES was to reinstate the lower extremity, FES-evoked exercise enhanced whole-body metabolism in subjects with SCI. Thus, hybrid FES allows patients to perform voluntary upper extremity and FES-assisted lower body exercises simultaneously, reducing disabling limitations and focusing on their treatment (Andrews et al. 2017). Therefore, FES is expected to provide conative exercises with multiple effects.
Another group of this analysis, robotic training and LT, is devoted to the rehabilitative properties and effectiveness of electromechanical robots as assistive devices for patients with SCI and physical activity limitations. This clinical practice allows individuals to practice gait motions more independently of assistance, probably with their body weight supported and with robotic motion of the lower limbs (Laursen et al. 2016). After an injury, patients experience a decrease in gait speed, limited functional mobility, and an increased risk of falls (Louie et al. 2015). Ultimately, enhancing mobility and activity is important for individuals with SCI. In this context, studies on LT have focused on the effects of ambulation and improvements in lower extremity function. In this review, five [7, 8, 9, 10, 11] publications reported positive changes in walking ability, lower limb kinematic data, and motor scores with locomotor and robotic training. Several studies related to robotic training and LT have examined the function (e.g., speed) and quality (e.g., kinematics) of locomotion. In the training paradigm, the intervention time ranged from 30 min to 3 hours and the duration ranged from 4 weeks to 3 months. Compared with FES, this intervention was slightly shorter in duration. They employed Lokomat® robotic treadmill training device (Hocoma, Inc.) [10, 11] and MAHI Exo-II robotic device [12]. Several studies have focused on individuals with iSCI. Morawietz and Moffat (2013) attributed this inclination to the growing number of individuals with iSCI who have great possibilities for improvement. In cases of incomplete injury, it is critical to enhance physical activity and to return to regular activities; hence, gait training is deemed critical. Patients with iSCI should concentrate on the physical problems such as reducing activities and limiting participation (Carpenter et al. 2007). These findings confirm that rehabilitation should be tailored to the patient’s condition and that ambulation training is an important rehabilitation strategy for patients with iSCI. Furthermore, several publications [7, 8, 9] have focused on exercise intensity. They compared the effects of low- and high-intensity exercise to verify which exercise was effective for individuals with SCI. In summary, these studies showed that higher intensities were more beneficial for the cardiometabolic aspects.
Although the abovementioned clinical practices are relatively new approaches that use new technologies, some studies have employed conventional rehabilitation for SCI. The analyzed papers dealt with resistance, aerobics, balance, and mixed methods. The participants performed functional exercises that encompassed physical and motor skills. Researchers using traditional methods have designed their own exercise programs or followed guidelines, such as the American College of Sports Medicine guidelines and the 2008 Physical Activity Guidelines for Americans [16]. Regarding the exercise protocol, the intervention time ranged from 20 to 40 min, and the duration ranged from 6 to 12 weeks. Unlike other methods in the study, participants in the traditional regimens had a long duration of injury (i.e., time since injury). This treatment is expected to be used in chronic patients who require active movements rather than assistive devices. Importantly, these studies emphasized patient independence during intervention [13, 14]. These programs were designed to be performed and reproduced on their own and were implemented in the wheelchair itself.
In conclusion, this systematic analysis confirmed that FES might target the whole-body exercise effect and that robotic training was effective in improving walking ability. These devices play supportive roles and exert various metabolic effects. In addition, traditional methods are expected to work well in patients with chronic SCI who need to enhance their physical independence. We found that appropriate rehabilitation is required depending on the patient’s injury and paralysis level and that protocols, such as exercise intensity and duration, should be different. The combination of SCI and technology is constantly evolving, with several different studies reported annually. For this quantitative flood, it is important to provide a precise direction regarding which treatments are effective, at what stage, and for which patients. Therefore, by simultaneously reviewing and analyzing both technological and conventional rehabilitation, this study presents a holistic view of effective intervention protocols and results. This limitation suggests that the systematic review could include studies with low quality and small effect, which can potentially bias the outcomes. In addition, Spanish and German papers were excluded from the analysis.
Conclusion
SCI may cause loss of sensory function, paralysis, and limited functional mobility. Researchers have adopted several rehabilitation approaches to reduce these negative effects in patients with SCI. We aimed to identify various therapeutic options and develop effective treatment regimens. First, it examined research involving technologies that utilize electrical instruments and conventional rehabilitation. We also found that FES is utilized as a comprehensive rehabilitation program, including the upper and lower limbs, and that LT with robots is effective in enhancing walking ability. Using traditional methods, we discovered that various training programs emphasize the physical independence of patients with chronic SCI. This systematic review presents specific findings that hold the potential to provide practical rehabilitation options for patients with SCI.
Data availability
Not applicable.
References
Afshari K, Ozturk D, Yates B, Picard G, Taylor A (2022) Effect of hybrid FES exercise on body composition during the sub-acute phase of spinal cord injury. Plos one 17(1):e0262864
Andrews B, Gibbons R, Wheeler G (2017) Development of functional electrical stimulation rowing: the Rowstim series. Artificial Organs 41(11):E203–E212
Awad L, Kesar M, Reisman D, Binder-Macleod A (2013) Effects of repeated treadmill testing and electrical stimulation on post-stroke gait kinematics. Gait Posture 37(1):67–71
Carpenter C, Forwell J, Jongbloed E, Backman L (2007) Community participation after spinal cord injury. Arch Phys Med Rehab 88(4):427–433
Chou RC, Taylor JA, Solinsky R (2020) Effects of hybrid-functional electrical stimulation (FES) rowing whole-body exercise on neurologic improvement in subacute spinal cord injury: secondary outcomes analysis of a randomized controlled trial. Spinal Cord 58(8):914–920
Davis GM, Hamzaid NA, Fornusek C (2008) Cardiorespiratory, metabolic, and biomechanical responses during functional electrical stimulation leg exercise: health and fitness benefits. Artificial Organs 32(8):625–629
DiPiro ND, Embry AE, Fritz SL, Middleton A, Krause JS, Gregory CM (2016) Effects of aerobic exercise training on fitness and walking-related outcomes in ambulatory individuals with chronic incomplete spinal cord injury. Spinal Cord 54(9):675–681
Duffell LD, de Neufville DN, Newham DJ (2010) Power output during functional electrically stimulated cycling in trained spinal cord injured people. Neuromodul: Technol Neural Interface 13(1):50–57
Eng J, Teasell R, Miller W, Wolfe D, Townson A, Aubut JA, Konnyu K (2007) Spinal cord injury rehabilitation evidence: method of the SCIRE systematic review. Topics Spinal Cord Injury Rehab 13(1):1–10
Francisco GE, Yozbatiran N, Berliner J, O'Malley MK, Pehlivan AU, Kadivar Z, Boake C (2017) Robot-assisted training of arm and hand movement shows functional improvements for incomplete cervical spinal cord injury. Am J Phys Med Rehab 96(10):S171–S177
Gorgey AS, Dolbow DR, Dolbow JD, Khalil RK, Castillo C, Gater DR (2014) Effects of spinal cord injury on body composition and metabolic profile–Part I. J Spinal Cord Med 37(6):693–702
Gorgey AS, Khalil RE, Davis JC, Carter W, Gill R, Rivers J, Adler RA (2019) Skeletal muscle hypertrophy and attenuation of cardio-metabolic risk factors (SHARC) using functional electrical stimulation-lower extremity cycling in persons with spinal cord injury: study protocol for a randomized clinical trial. Trials 20:1–14
Gorman PH, Scott W, VanHiel L, Tansey KE, Sweatman WM, Geigle PR (2019) Comparison of peak oxygen consumption response to aquatic and robotic therapy in individuals with chronic motor incomplete spinal cord injury: a randomized controlled trial. Spinal Cord 57(6):471–481
Ho CH, Triolo RJ, Elias AL, Kilgore KL, DiMarco AF, Bogie K, Mushahwar VK (2014) Functional electrical stimulation and spinal cord injury. Phys Med Rehab Clin 25(3):631–654
Kim DI, Park DS, Lee BS, Jeon JY (2014) A six-week motor-driven functional electronic stimulation rowing program improves muscle strength and body composition in people with spinal cord injury: a pilot study. Spinal Cord 52(8):621–624
Laursen CB, Nielsen JF, Andersen OK & Spaich EG (2016) Feasibility of using Lokomat combined with functional electrical stimulation for the rehabilitation of foot drop. Eur J Transl Myol 26(3)
Leech A, George H (2017) High-intensity locomotor exercise increases brain-derived neurotrophic factor in individuals with incomplete spinal cord injury. J Neurotrauma 34(6):1240–1248
Leech KA, Kinnaird CR, Holleran CL, Kahn J, Hornby TG (2016) Effects of locomotor exercise intensity on gait performance in individuals with incomplete spinal cord injury. Phys Ther 96(12):1919–1929
Lotter JK, Henderson CE, Plawecki A, Holthus ME, Lucas EH, Ardestani MM, Hornby TG (2020) Task-specific versus impairment-based training on locomotor performance in individuals with chronic spinal cord injury: a randomized crossover study. Neurorehab Neural Repair 34(7):627–639
Louie DR, Eng JJ, Lam T (2015) Gait speed using powered robotic exoskeletons after spinal cord injury: a systematic review and correlational study. J Neuroeng Rehab 12(1):1–10
Lynch CL, Popovic MR (2008) Functional electrical stimulation. IEEE Control Syst Mag 28(2):40–50
Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M (2003) Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther 83(8):713–721
Martinez SA, Nguyen ND, Bailey E, Doyle-Green D, Hauser HA, Handrakis JP, Harel NY (2018) Multimodal cortical and subcortical exercise compared with treadmill training for spinal cord injury. PloS One 13(8):e0202130
Morawietz C, Moffat F (2013) Effects of locomotor training after incomplete spinal cord injury: a systematic review. Arch Phys Med Rehab 94(11):2297–2308
Nas K, Yazmalar L, Şah V, Aydın A, Öneş K (2015) Rehabilitation of spinal cord injuries. World J Orthopedics 6(1):8
Onushko T, Mahtani GB, Brazg G, Hornby TG, Schmit BD (2019) Exercise-induced alterations in sympathetic-somatomotor coupling in incomplete spinal cord injury. J Neurotrauma 36(18):2688–2697
Sadeghi M, Ghasemi G, Karimi M (2018) Effect of 12-week rebound therapy exercise on static stability of patients with spinal cord injury. J Sport Rehab 28(5):464–467
Sherrington C, Herbert RD, Maher CG, Moseley AM (2000) PEDro. A database of randomized trials and systematic reviews in physiotherapy. Manual Ther 5(4):223–226
Silva DF, Resende NM, Aidar FJ & CE PDO (2020). Effects of circuit resistance training on muscle power, functional agility, and bones' mineral content in people with spinal injury. J Sports Med Phys Fitness, 61(4), 505-511
Thrasher TA, Ward JS, Fisher S (2013) Strength and endurance adaptations to functional electrical stimulation leg cycle ergometry in spinal cord injury. NeuroRehabilitation 33(1):133–138
Vivodtzev I, Napolitano A, Picard G, Taylor JA (2020) Ventilatory support during whole-body row training improves oxygen uptake efficiency in patients with high-level spinal cord injury: A pilot study. Respiratory Med 171:106104
Warburton D, Eng J, Krassioukov A, Sproule S (2007) Cardiovascular health and exercise rehabilitation in spinal cord injury. Topics Spinal Cord Injury Rehab 13(1):98–122
Whiteneck G, Cassaway J, Dijkers M, Jha A (2009) New approach to study the contents and outcomes of spinal cord injury rehabilitation: the SCIRehab Project. J Spinal Cord Med 32(3):251–259
Wouda MF, Wejden L, Lundgaard E, Strøm V (2016) Energetic and cardiovascular responses to treadmill walking and stationary cycling in subjects with incomplete spinal cord injury. Spinal Cord 54(1):51–56
Acknowledgments
This study was supported by the Translational R&D Program on Smart Rehabilitation Exercises (NCR-TRSRE-Eq01A), National Rehabilitation Center, Ministry of Health and Welfare, Korea.
Funding
This study was supported by the Translational R&D Program on Smart Rehabilitation Exercises (NCR-TRSRE-Eq01A), National Rehabilitation Center, Ministry of Health and Welfare, Korea.
Author information
Authors and Affiliations
Contributions
Conceptualization, K.E.L. and B.J.; methodology, K.E.L.; software, K.E.L.; validation, K.E.L. and B.J.; formal analysis, K.E.L. and B.J.; investigation, K.E.L. and B.J.; resources, B.J.; data curation, K.E.L. and B.J.; writing- original draft preparation, K.E.L.; writing—review and editing, K.E.L. and B.J.; visualization, K.E.L.; supervision, B.J.; project administration, B.J.; funding acquisition, B.J. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Institutional review board statement
Not applicable.
Informed consent statement
Not applicable.
Ethics approval
Not applicable.
Consent for publication
Not applicable.
Consent to participate
Not applicable.
Conflicts of interest
The authors declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, K.E., Jeoung, B. An analysis of the effectiveness of rehabilitation protocols for patients with spinal cord injury: A systematic review. J Public Health (Berl.) (2023). https://doi.org/10.1007/s10389-023-02115-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10389-023-02115-9