Abstract
Aim
Public health officials recommended the use of face masks by the population to combat the transmission of COVID-19. Studies on self-reported behaviour are a poor substitute for assessing adherence to government recommendations. This study aimed to determine the percentage of pedestrians wearing masks in the Central Business District (CBD) and a suburb of Auckland, New Zealand (NZ).
Methods
This direct observational study of pedestrians crossing two busy intersections occurred between 22 August 2020 and 7 March 2022. Data collection occurred at three separate times during the day, in the morning (from 8 to 9 am), noon (from 12 to 1 pm) and afternoon (from 4 to 5 pm) for precisely one hour each time.
Results
Over 12 days of COVID alert level restrictions, we observed 30,855 pedestrians. Overall, 57.9% of pedestrians wore a mask outdoors. Masks-wearing was significantly higher in the CBD (64.0%) than in the suburb (38.7%), p < 0.001. Masks use was lower in the morning (51.1%) than at noon (56.1%) or afternoon (62.7%), p < 0.001, both in the CBD and the suburb.
Conclusion
This was the first observational study in NZ examining the public’s mask use during the COVID-19 pandemic. From our observations, there may be opportunities for improvement in public face mask use rates to decrease the spread of COVID-19 in the population. In addition, our findings can inform national and international public health agencies about face mask uptake in public.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
COVID-19 – global impact, transmission and non-pharmaceutical interventions
COVID-19 has been one of the most significant challenges globally and domestically since World War II (Lederer 2020). Since the pandemic’s start, the virus responsible for it has killed over 6.8 million people worldwide (World Health Organization [WHO] 2023). Commonly transmitted via droplets and small airborne particles from the mouth or nose of an infected person (Bundgaard et al. 2021; Gray et al. 2020), the virus can pass to those in close contact (Brooks and Butler 2021; Cheng et al. 2020). Healthy individuals can also get infected by touching their eyes, nose, or mouth with contaminated hands (Bundgaard et al. 2021). The infection is frequently asymptomatic or associated with only mild symptoms (Abaluck et al. 2022; Bundgaard et al. 2021; Eikenberry et al. 2020; Gray et al. 2020; Worby and Chang 2020). Still, it may cause severe and life-threatening illness in immunocompromised and older people, with a case fatality ratio of over 10% in the latter group (Worby and Chang 2020). As no vaccine was initially available, interventions to mitigate disease transmission were urgently needed, particularly throughout the community (Worby and Chang 2020). Public health authorities worldwide recommended large-scale non-pharmaceutical interventions to reduce the spread of infection (Flaxman et al. 2020; Gray et al. 2020). Among these interventions, mask-wearing, contact tracing, and physical distancing were practical measures to mitigate the impact of the pandemic on the population (Gray et al. 2020; Jagadeesan et al. 2021). While governments and public health departments strongly encouraged travel restrictions and the closing of borders, there was no consensus regarding mass masking (Cheng et al. 2020; Eikenberry et al. 2020).
Mask-wearing recommendations – global perspectives
Mask-wearing has the potential to slow the spread of the virus (Abaluck et al. 2022) and was among the first non-pharmaceutical interventions recommended to reduce the risk of transmission (Li et al. 2020). In this study, masks were defined as any cloth, medical-grade mask, or N95 respirator worn over the face (Jagadeesan et al. 2021). At the pandemic’s start, limited and inconsistent scientific evidence supported the effectiveness of masking the general public (Bundgaard et al. 2021; Leech et al. 2022; WHO 2020). Worldwide, public health officials strongly recommended mask-wearing for healthcare professionals, while its usefulness for the public was controversial (Eikenberry et al. 2020; Leech et al. 2022). An early randomised community-based study (DANMASK-19) found no significant reduction (over 50%) in the infection rate among the public wearing masks (Bundgaard et al. 2021). In contrast, a few small observational studies reported an association between mask use by an infected person and the prevention of onward transmission in public settings (WHO 2020). Several studies, most published as preprints, reported a decline in the number of COVID-19 cases associated with face masks used by the public (WHO 2021). Using observational data from 92 global regions, Leech et al. (2022) found evidence that mask-wearing reduces virus transmission. Studies in the United States (USA) modelled that high public compliance with facemask use can significantly decrease the number of daily cases and death rates (Eikenberry et al. 2020; Fischer et al. 2021). When used, face masks can reduce the COVID-19 spread with a pooled relative risk (95% CI) of 0.12 [0.06, 0.27] (p < 0.001), as shown in a meta-analysis (Tabatabaeizadeh 2021).
In June 2020, the WHO recommended using masks for the first time when interacting with non-members of the individual’s household (WHO 2020). Face mask use by the public as an infection control measure was recommended early in the pandemic by governments in China, Hong Kong and Taiwan for all healthy persons in crowded public spaces (Feng et al. 2020; Kemmelmeier and Jami 2021). At the same time, masks were also recommended for those symptomatic in Japan and Singapore (Feng et al. 2020; Worby and Chang 2020). Hong Kong has experienced past SARS outbreaks, so people volunteered to wear masks even without official guidelines. As a result of many Asian countries implementing early public masking guidelines, the rest of the world experienced shortages of medical-grade masks (Feng et al. 2020).
In contrast, Western countries were slower to encourage or adopt face masks for the public, even though there was a growing recognition that this should be part of mitigation strategies to slow the spread of COVID-19. One of the reasons was the fFear of unnecessary costs and the depletion of the healthcare sector of much-needed face masks. In the early days of the pandemic, healthy individuals were not encouraged to wear a face mask (Worby and Chang 2020). In April 2020, the USA’s Centers for Disease Control and Prevention (CDC) recommended mask-wearing for the public for the first time. The United Kingdom’s (UK) government urged the utilization of cloth masks in June 2020, limited to public transport settings only (Worby and Chang 2020). In August 2020, the NZ government recommended public mask-wearing for the first time, stipulating that masks were required outdoors and in enclosed public spaces where physical distancing was impossible (New Zealand [NZ] Government 2020).
NZ’s COVID-19 response and mask-wearing policies
At the start of the pandemic, the NZ population without prior experience of previous SARS outbreaks found themselves unfamiliar with the public health measures implemented to reduce the virus transmission. That was in contrast to other nations where the public adopted mask-wearing even without government agencies’ specific recommendations (Cheng et al. 2020). In March 2020, NZ committed to an elimination strategy in response to the COVID-19 pandemic (Ministry of Health - Manatu Hauora 2022). The NZ government implemented a four-tier Alert Level system: 1 ‘prepare’, 2 ‘reduce’, 3 ‘restrict’ and 4 ‘lockdown’, and recommended wearing face masks to stop the spread of COVID-19 and keep the wearer and others safe (NZ Government 2022). All healthy individuals aged 12 and over were strongly encouraged to wear a face mask at all alert levels, except at Level 1, when the only mask-wearing recommendations were when using public transportation and aeroplanes. The Traffic Light system replaced the Alert Levels system in December 2021 (Ministry of Health - Manatu Hauora 2022). This three-tier system based its restrictions on vaccination rates and pressure on the health care system. The general recommendation for ‘Orange’ and ‘Red’ levels was to wear a face mask whenever leaving the house. The exceptions were when the public was able to physically distance themselves from other people (at home and in some workplaces) (Ministry of Health - Manatu Hauora 2022). During the early stages of the pandemic, the types of masks recommended included medical and non-medical-grade masks. Face masks used early in the pandemic did not have to conform to any infection control standard. They could be single-use disposable or reusable fabric masks. These recommendations changed once the more transmissible SARS-CoV-2 variants emerged, and scarves, bandannas, or t-shirts became no longer acceptable as face coverings (NZ Government 2022).
Assessing public mask use – self-reported versus direct observations
Monitoring mask use helps design interventions to improve the prevalence of mask-wearing among the public (Jagadeesan et al. 2021). The literature on mask-wearing during the COVID-19 pandemic shows that some studies focus on the effect of government mask-wearing recommendations on COVID-19 transmission. Those studies showed a weak relationship between government recommendations’ timing and mask-wearing among the public, making detecting the link between recommendations and transmission challenging (Leech et al. 2022). Some studies have inferred limited or inconclusive effects of government recommendations on transmission, while others found evidence that mask recommendations lead to decreased transmission and mortality (Leech et al. 2022). Leech et al. (2022) argue that the data on mask-wearing recommendations timing may be a poor substitute for analysing the virus’s transmission. Introducing public health official regulations regarding mask-wearing is a one-off intervention that may have an impact soon after its announcement. Still, it loses its significance after the gradual behaviour change and once pandemic fatigue occurs (Leech et al. 2022; MacIntyre et al. 2021). The circumstances of mandate policies are highly heterogeneous regarding the pre-existing level of voluntary wearing at the time of implementation and how they are defined, enforced and complied with (Leech et al. 2022). Studies that use self-reported mask-wearing behaviour suffer from bias (Haischer et al. 2020; Jakubowski et al. 2021), especially those collecting personal details, leading to inflated mask-wearing data (Leech et al. 2022). Self-reported mask use differs considerably between countries (Worby and Chang 2020). A self-reporting survey in China in early 2020 found that 99.0% of participants wore a mask outdoors (Tan et al. 2021), while a study in Kenya found that the difference between self-reported and observed pedestrian behaviour can be as high as 77.7% (95% CI 0.7, 0.8). That proves that the public knows that masks are recommended, and their use is socially desirable. However, people do not wear them consistently (Haischer et al. 2020). In contrast, direct observational studies can provide objective results on the prevalence of public mask-wearing in the community (Jagadeesan et al. 2021).
Study rationale
Few observational studies on pedestrians' mask-wearing during the COVID-19 pandemic have been published. Investigations on using masks in the community are ongoing; nevertheless, published work has identified the need for continued research. Well-conducted observational studies are required to clarify outstanding inquiries concerning mask use in community settings (WHO 2021). This study aimed to determine the uptake of general mask-wearing in Auckland, CBD, and compare it to a suburb during the COVID-19 pandemic.
Methods
Observations occurred during the COVID-19 pandemic at various alert levels over 12 days from 23 August 2020 to 7 March 2022, on week and weekend days. The authors deemed it essential to compare the centre of Auckland with a suburb (Devonport) to observe any differences between the city centre and the suburb. The CBD of Auckland is the leading centre of NZ’s business and economic development, with high-rise buildings mainly used for commercial and retail purposes. The CBD is also culturally diverse and densely populated. A feature of the Auckland CBD relevant to this study is that the Managed Isolation Quarantine hotels were within blocks of the chosen intersection, and authors were expecting that in the proximity of these facilities, the rate of pedestrians wearing face masks would be high. To compare the uptake of mask-wearing by the public in the suburbs, we chose the suburb of Devonport on Auckland’s North Shore as the second location. The intersection selected in the suburb represented this mainly residential suburb as the public visited it frequently, close to grocery shops and cafes. The data collection site in the suburb was also close to the beach and a large public park. The distance between the observation points was approximately 3.7 km. Both locations had high rates of pedestrian traffic, which minimised the time observers spent near individuals. The observers wore medical-grade face masks and maintained physical distancing at all times. They counted everyone who walked past them, omitting the people in wheelchairs, bicycles, scooters or skateboards and people travelling in cars during the one-hour observation period. Children being held or being pushed in a child carriage were also excluded. Observers recorded pedestrians as wearing a mask if it appeared to be worn correctly. We counted any face mask that covered the mouth and nose, including medical and non-medical-grade face masks (reusable fabric face masks, bandanas, scarves or t-shirts) as per the NZ government recommendations (NZ Government 2022).
Observers collected data using their smartphones. Counting was aided by a freely available electronic counter software application (akibonn. Multi Counter APK. 1.0.1. ed2011.) downloaded onto Android smartphones that could be set with two counters, one for mask wearers and the other for those without masks. Interobserver testing was performed over a one-hour trial observation. Interobserver agreement using the electronic counter was 96%. Owing to the lack of researcher availability, no recordings occurred in the suburb at noon on day 6.
Data collection occurred on each observation day at three separate times during the day, in the morning (from 8 to 9 am), noon (from 12 to 1 pm) and afternoon (from 4 to 5 pm) for precisely one hour each time. We expected differences in the mask-wearing rates between morning, noon and afternoon observations. Most morning and afternoon pedestrians walked to or from work, and some shopped, whereas at noon, the pedestrians were more likely to stroll, visiting cafes and parks. Observations were made on weekdays when people were commuting to work, in work attire, and compared with weekends when most people were not working.
From the literature, it is unknown if weather influences outdoor mask use. Brooks and Butler (2021) suggest that warm environments make mask-wearing unpleasant, primarily when used for long periods. Weather information from the Meteorological Service of NZ for each session was recorded for temperature, wind speed, rainfall, humidity, and atmospheric pressure for Auckland’s CBD. The suburban observation location was not far from the CBD point, measured in a straight line, so the weather was essentially the same.
Statistical analysis
Descriptive statistics were conducted for each variable. Chi-squared tests determined a statistically significant difference in frequencies between categories. We counted ‘pedestrians with masks’ and ‘pedestrians without masks’. The proportion of pedestrians wearing masks was compared between locations, circulating COVID-19 variants, time of the day, day of the week and weather (rain or not). A p-value of less than 0.05 was considered significant. Statistical analysis was performed with SPSS version 28.0 statistic software package.
Results
We observed a total of 30,855 pedestrians for face mask usage. The CBD intersection was more active (23,393 pedestrians counted), although most businesses were closed during the COVID-19 restrictions. There were a total of 71 hours of observations (36 in the CBD and 35 in Devenport), of which 11 hours occurred at alert level 4 (lockdown) when there were widespread restrictions on movement across Auckland. Overall, the percentage of pedestrians wearing masks during the study period was 57.9%. In the CBD, the overall rate was 64.0%, ranging from 19.2% to 80.3%, while in the suburb, it was 38.7%, with a daily average ranging from 1.2% to 74.8% (Fig. 1, Supplementary Information). The OR of wearing a mask in CBD versus Devonport was 2.8 (95% CI, 2.6 to 2.9.). More people wore masks during alert level 3 step 1 (68.6%), level 4 (74.3%) and ‘red’ (64.2%) than alert level 3 (34.6%) (Table 1, Fig. 1). Masks use was lower in the morning (51.1%) than at noon (56.1%) or afternoon (62.7%) (Table 1). Of 12 days of observations, 6 were weekend days, and 6 were weekdays. Fewer pedestrians wore masks during the weekend than the rest of the week. The percentage of mask-wearing increased significantly during the delta and omicron SARS-CoV-2 outbreaks (Table 1).
Fewer pedestrians wore masks when it rained (Table 1). Overall, the OR of wearing a mask when it was raining was 0.50 (95% CI 0.4 to 0.5).
Discussion
While face mask use does not entirely prevent SARS-CoV-2 transmission, masking may be important in controlling the pandemic and averting future lockdowns (Pitanga et al. 2021). However, no direct observational studies have been reported in the literature examining universal face-masking in NZ. Worldwide, a small number of similar studies have been published to date. This study aimed to quantify mask usage by pedestrians crossing through two busy intersections, one in the Auckland CBD and the second in the suburb of Devonport. During the study period, face mask usage in public was found not widely practised, despite recommendations by the NZ government. We examined the effect of city location on face mask-wearing by the public. A small but noticeable number of people wore their masks incorrectly (under their chin). These people were, in some cases, smoking, eating or drinking (outside of food and drinking businesses). We assumed that some of them had their masks ready to be worn when entering a supermarket or re-entering a café, etc. However, they were not wearing face masks in proximity to other pedestrians and were recorded as not wearing a mask.
We found six studies that had a study design similar to our research. One of the earliest studies on mask-wearing during the COVID-19 pandemic was published in April 2020. Cheng et al. (2020) assessed the number of pedestrians wearing masks among the first 50 people encountered during their morning commute in Hong Kong over three consecutive days by 67 staff members from the Queen Mary Hospital (Cheng et al. 2020). They found a high mask-wearing compliance [96.6% (95% CI 95.7, 97.2)]. The public of Hong Kong was on high alert at the beginning of the pandemic, having experienced the SARS outbreak in 2003 (Cheng et al. 2020). Owing to the experience of previous SARS outbreaks, the Hong Kong population voluntarily wears face masks even without the government’s recommendations. In Honolulu, USA, 77% of all individuals observed were appropriately using face masks that covered their nose and mouth (Tamamoto et al. 2020). Another observational study in Poland was conducted in student resident locations in ‘open spaces’ such as sidewalks and parks at three different periods. The study researchers noticed that the percentage of those wearing masks decreased from 73.6% during the first point time of observations to 66.5% a week later and 65.7% two weeks later (Ganczak et al. 2021).
The mask-wearing rate in our study was closer to that observed in an Iranian study. In south-eastern Iran, in August 2020, Rahimi et al. (2021) observed a mask-wearing prevalence of 45.6% (95% CI 44.6, 46.5) among pedestrians in Ahvaz. Jagadeesan et al. (2021) observed that nearly one-third of residents of Chennai, India, wore masks correctly in public places. Jakubowski et al. (2021) found that mask-wearing among the Kenyan public was higher (22%) when the chances of meeting strangers were higher (daily commuting) than in places such as villages (14%) where those observed were expecting to meet family, friends and neighbours.
As expected, more pedestrians wore face masks in Auckland’s CBD than in Devonport. The Auckland CBD is primarily a business area with a higher population density than the suburbs. If fear of exposure is a motivating factor for mask use, the higher density of pedestrians on footpaths presumably increases the risk of exposure, particularly to strangers. This finding is consistent with other studies. For example, the rate of compliance with correct public mask use in downtown Honolulu (business area) (88%) was significantly higher than in Waikiki (recreational area) (66%) (Tamamoto et al. 2020). In Chennai (India), the prevalence of appropriate mask use outdoors was significantly lower in the slums (28–29%) than in non-slum areas (36–35%) of Chennai (p < 0.01). A Hong Kong study also observed differences between mask-wearing in business and recreational areas. Compared to workplaces, the authors observed more COVID-19 clusters in mask-off settings (recreational) locations (Cheng et al. 2020). More research conducted in the USA found that the population living in suburban areas is more resistant to wearing a mask than the urban population (Haischer et al. 2020). In Wisconsin, USA, between June and August 2020, a study found that mask-wearing was similar in urban and suburban areas; however, the odds of observing a masked shopper were four times higher in urban and suburban areas than in rural shops (Haischer et al. 2020).
We found more people wore masks during the higher alert levels 3.1, 4 and ‘red’. Also, more people wore masks during delta and omicron variant outbreaks. In an NZ study in April 2020, the authors identified that one barrier to face mask-wearing by the public was a perceived national shortage and the belief that healthcare and essential workers needed them more. However, mask-wearing was also strongly related to ideas about efficacy and perceived discomfort (2020). Their findings are consistent with the low levels of mask usage observed during alert level 3 in August 2020. Risk perception (level of fear) strongly affects preventative measures adopted by the population (Wang et al. 2021). Therefore, the percentage of pedestrians wearing face masks increased when delta and omicron variants (more transmissible and with poorer outcomes) were reported for the first time in NZ. Public perceptions and personal characteristics are heterogeneous between subgroups, which may impact health-protective behaviours such as mask-wearing (Fujii et al. 2021). We found that the mask-wearing prevalence was higher at noon and in the afternoon. In contrast, in the Iranian study, the prevalence was significantly higher in the morning (49.4%) compared to the afternoon (43.9%) (p < 0.001) (Rahimi et al. 2021). There may be various reasons for higher mask-wearing rates at noon and in the afternoon. The number of pedestrians in our study was higher during those times of the day (Table 1). It is possible that people feel a higher risk of exposure to the virus when more people are out and about and interacting with others, making them more likely to wear masks for protection. In addition, the social influence of seeing more people wearing masks might influence others to follow suit. Future research will be needed to examine these differences observed in our study.
To our knowledge, this is the first observational study on public mask-wearing in NZ. We directly observed pedestrians’ behaviour during different alert levels, at other times of the day, on weekdays and weekends, over a more extended period and with various circulating virus variants. We also recorded weather variables, searching for any relationships with mask-wearing. The study had several limitations. There were only two observers and, hence, two observation sites. Therefore, our study has limitations due to its convenience sampling and lack of additional observation sites. The results do not necessarily represent the entire Auckland City or NZ population. We did not include in the study a small number of pedestrians with faces obscured by umbrellas or looking away from the observer. We did not record the type of face mask, such as cloth, medical-grade masks or N95 respirator, as it was impossible to count and attempt to identify the mask type. We also did not count people exercising their pets while not wearing masks. Individuals may wish to wear face masks during the pandemic; however, there is debate on whether it is safe for individuals to exercise while wearing a face mask and what should be the recommended exercise intensity for the general population if wearing a mask. While the WHO and CDC recommend that everyone wear a face mask in public, both organisations do not encourage wearing a mask while exercising (Poon et al. 2021). Specifically, the WHO states that wearing masks during exercise may reduce the individual’s ability to breathe comfortably. At the same time, the CDC recognises it may be challenging to wear a mask during high-intensity exercise (Poon et al. 2021). As this study observed outdoor pedestrians, it is unknown what the relationship to mask use in an enclosed space is.
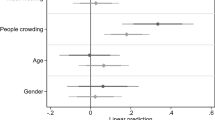
We did not determine the impact of gender, age or ethnicity on mask-wearing behaviour. Not estimating age and sex is an obvious limitation of this study. Age and gender could have been misclassified, leading to biased estimations. However, a large sample size increases the study power and offsets the effect of variability from the estimates (Haischer et al. 2020). In addition, a breakdown by ethnicity would have helped tailor the mask-wearing recommendations for specific groups. We did not find any relationship between weather variables and the frequency of pedestrians wearing masks, nor did we examine the causes of not wearing a mask. Another limitation of our study is that we did not count separately those wearing the mask incorrectly; instead, we recorded them as ‘not wearing a mask’. Possessing but not wearing a mask does not stop COVID-19 transmission. We did not observe mask use in other settings, including public transport, shops and recreational areas where people are close to strangers. Manually detecting mask-wearing in public is cumbersome, with multiple restrictions and limitations. With the current advancements in technology, a real-time system could be created to recognise a person wearing a face mask (Vibhuti et al. 2022). Finally, the observational nature of the study limits the interpretation of our findings to descriptive statistics that cannot be interpreted as causal.
Conclusion
To be motivated to wear masks, people must perceive that the policy measures are relevant to them (Kaine et al. 2022). As such, misconceptions and barriers to encouraging proper mask usage must be addressed. Policymakers can improve public compliance by focusing on subgroups of people when health administrations implement preventative measures (Fujii et al. 2021). Location-specific strategies to increase mask usage in areas with lower compliance may also be helpful. Our results suggest opportunities for improvement in public face mask use rates to potentially decrease the spread of COVID-19 in the population. In addition, the study provides information on how closely people in Auckland follow recommendations, highlighting the importance of monitoring public compliance with mask-wearing recommendations and adjusting policies accordingly.
Data availability
The data supporting this study’s findings are available from the corresponding author upon reasonable request.
Code availability
Not applicable.
References
Abaluck J, Kwong LH, Styczynski A, Haque A, Kabir MA, Bates-Jefferys E, Crawford E, Benjamin-Chung J, Raihan S, Rahman S, Benhachmi S, Bintee NZ, Winch PJ, Hossain M, Reza HM, Jaber AA, Momen SG, Rahman A, Banti FL et al (2022) Impact of community masking on COVID-19: a cluster-randomised trial in Bangladesh. Science 375(6577):eabi9069. https://doi.org/10.1126/science.abi9069
Brooks JT, Butler JC (2021) Effectiveness of mask wearing to control community spread of SARS-CoV-2. JAMA 325(10):998–999. https://doi.org/10.1001/jama.2021.1505
Bundgaard H, Bundgaard JS, Raaschou-Pedersen DET, von Buchwald C, Todsen T, Norsk JB, Pries-Heje MM, Vissing CR, Nielsen PB, Winsløw UC, Fogh K, Hasselbalch R, Kristensen JH, Ringgaard A, Porsborg Andersen M, Goecke NB, Trebbien R, Skovgaard K, Benfield T et al (2021) Effectiveness of adding a mask recommendation to other public health measures to prevent SARS-CoV-2 infection in Danish mask wearers: a randomized controlled trial. Ann Intern Med 174(3):335–343. https://doi.org/10.7326/m20-6817
Cheng VC-C, Wong S-C, Chuang VW-M, So SY-C, Chen JH-K, Sridhar S, To KK-W, Chan JF-W, Hung IF-N, Ho P-L, Yuen K-Y (2020) The role of community-wide wearing of face mask for control of coronavirus disease 2019 (COVID-19) epidemic due to SARS-CoV-2. J Infect 81(1):107–114. https://doi.org/10.1016/j.jinf.2020.04.024
Eikenberry SE, Mancuso M, Iboi E, Phan T, Eikenberry K, Kuang Y, Kostelich E, Gumel AB (2020) To mask or not to mask: modeling the potential for face mask use by the general public to curtail the COVID-19 pandemic. Infect Disease Modell 5:293–308. https://doi.org/10.1016/j.idm.2020.04.001
Feng S, Shen C, Xia N, Song W, Fan M, Cowling BJ (2020) Rational use of face masks in the COVID-19 pandemic. Lancet Respir Med 8(5):434–436. https://doi.org/10.1016/s2213-2600(20)30134-x
Fischer CB, Adrien N, Silguero JJ, Hopper JJ, Chowdhury AI, Werler MM (2021) Mask adherence and rate of COVID-19 across the United States. PLOS ONE 16(4):e0249891. https://doi.org/10.1371/journal.pone.0249891
Flaxman S, Mishra S, Gandy A, Unwin HJT, Mellan TA, Coupland H, Whittaker C, Zhu H, Berah T, Eaton JW, Monod M, Perez-Guzman PN, Schmit N, Cilloni L, Ainslie KEC, Baguelin M, Boonyasiri A, Boyd O, Cattarino L et al (2020) Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature 584(7820):257–261. https://doi.org/10.1038/s41586-020-2405-7
Fujii R, Suzuki K, Niimi J (2021) Public perceptions, individual characteristics, and preventive behaviors for COVID-19 in six countries: a cross-sectional study. Environ Health Prev Med 26(1):29. https://doi.org/10.1186/s12199-021-00952-2
Ganczak M, Pasek O, Duda Duma Ł, Świstara D, Korzeń M (2021) Use of masks in public places in Poland during SARS-Cov-2 epidemic: a covert observational study. BMC Public Health 21(1). https://doi.org/10.1186/s12889-021-10418-3
Gray L, Macdonald C, Tassell-Matamua N, Stanley J, Kvalsvig A, Zhang J, Murton S, Wiles S, Puloka V, Becker J, Johnston D, Baker MG (2020) Wearing one for the team: views and attitudes to face covering in New Zealand/Aotearoa during COVID-19 Alert Level 4 lockdown. J Primary Health Care 12(3):199. https://doi.org/10.1071/hc20089
Haischer MH, Beilfuss R, Hart MR, Opielinski L, Wrucke D, Zirgaitis G, Uhrich TD, Hunter SK (2020) Who is wearing a mask? Gender-, age-, and location-related differences during the COVID-19 pandemic. PLOS ONE 15(10):e0240785. https://doi.org/10.1371/journal.pone.0240785
Jagadeesan M, Polani R, Raju M, Sakthivel M, Murali S, Nagarajan R, Sendhilkumar M, Sambath I, Ilangovan K, Harikrishnan D, Venkatasamy V, Ganeshkumar P, Reddy M, Kaur P (2021) Surveillance for face mask compliance, Chennai, Tamil Nadu, India, October-December, 2020. PLOS ONE 16(9):e0257739. https://doi.org/10.1371/journal.pone.0257739
Jakubowski A, Egger D, Nekesa C, Lowe L, Walker M, Miguel E (2021) Self-reported mask wearing greatly exceeds directly observed use: urgent need for policy intervention in Kenya. medRxiv, 2021.2001.2027.21250487. https://doi.org/10.1101/2021.01.27.21250487
Kaine G, Greenhalgh S, Wright V (2022) Compliance with Covid-19 measures: Evidence from New Zealand. PLOS ONE 17(2):e0263376. https://doi.org/10.1371/journal.pone.0263376
Kemmelmeier M, Jami WA (2021) Mask wearing as cultural behavior: an investigation across 45 U.S. states during the COVID-19 pandemic. Front Psychol 12. https://doi.org/10.3389/fpsyg.2021.648692
Lederer EM (2020) UN chief says COVID-19 is worst crisis since World War II. https://apnews.com/article/asia-pacific-united-nations-virus-outbreak-financial-markets-us-news-dd1b9502802f03f88d56c34f7d95270c. Accessed 15 Aug 2020
Leech G, Rogers-Smith C, Teperowski Monrad J, Sandbrink JB, Snodin B, Zinkov R, Rader B, Brownstein JS, Gal Y, Bhatt S, Sharma M, Mindermann S, Brauner JM, Aitchison L (2022) Mask wearing in community settings reduces SARS-CoV-2 transmission. Proc Natl Acad Sci 119(23):e2119266119. https://doi.org/10.1073/pnas.2119266119
Li T, Liu Y, Li M, Qian X, Dai SY (2020) Mask or no mask for COVID-19: A public health and market study. PLOS ONE 15(8). https://doi.org/10.1371/journal.pone.0237691
MacIntyre CR, Nguyen P-Y, Chughtai AA, Trent M, Gerber B, Steinhofel K, Seale H (2021) Mask use, risk-mitigation behaviours and pandemic fatigue during the COVID-19 pandemic in five cities in Australia, the UK and USA: a cross-sectional survey. IJID 106:199–207. https://doi.org/10.1016/j.ijid.2021.03.056
Ministry of Health - Manatu Hauora (2022) Covid-19: Response planning. https://www.health.govt.nz/covid-19-novel-coronavirus/covid-19-response-planning. Accessed 20 November 2022
New Zealand Government (2020) Rapid response to cases of COVID-19 in the community. https://covid19.govt.nz/assets/resources/legislation-and-key-documents/Rapid-response-one-pager.pdf. Accessed 15 November 2021
New Zealand Government (2022) Wear a face mask. https://covid19.govt.nz/prepare-and-stay-safe/keep-up-healthy-habits/wear-a-face-mask/. Accessed 20 December 2022
Pitanga FJG, Brito MP, Silva MS, Gomes JM, Aras Júnior R, Alves CFA, Caria ACI (2021) Physical activity for health and use of face masks in the COVID-19 pandemic. Rev Assoc Med Bras 67(5):641–644. https://doi.org/10.1590/1806-9282.20210212
Poon ET-C, Zheng C, Wong SH-S (2021) Effect of Wearing Surgical Face Masks During Exercise: Does Intensity Matter? Front Physiol 12. https://doi.org/10.3389/fphys.2021.775750
Rahimi Z, Shirali GA, Araban M, Mohammadi MJ, Cheraghian B (2021) Mask use among pedestrians during the Covid-19 pandemic in Southwest Iran: an observational study on 10,440 people. BMC Public Health 21(1). https://doi.org/10.1186/s12889-020-10152-2
Tabatabaeizadeh S (2021) Airborne transmission of COVID-19 and the role of face mask to prevent it: a systematic review and meta-analysis. Eur J Med Res 26(1):1. https://doi.org/10.1186/s40001-020-00475-6
Tamamoto KA, Rousslang ND, Ahn HJ, Better HE, Hong RA (2020) Public compliance with face mask use in Honolulu and regional variation. Hawaii J Health Soc Welf 79(9):268–271 https://pubmed.ncbi.nlm.nih.gov/32914093
Tan M, Wang Y, Luo L, Hu J (2021) How the public used face masks in China during the coronavirus disease pandemic: a survey study. Int J Nurs Stud 115:103853. https://doi.org/10.1016/j.ijnurstu.2020.103853
Vibhuti JN, Singh H, Rana PS (2022) Face mask detection in COVID-19: a strategic review. Multimed Tools Appl 81(28):40013–40042. https://doi.org/10.1007/s11042-022-12999-6
Wang L, Yu J, Chen D, Yang L (2021) Relationships among COVID-19 prevention practices, risk perception and individual characteristics: a temporal analysis. Int J Environ Res Public Health 18(20):10901. https://doi.org/10.3390/ijerph182010901
Worby CJ, Chang H-H (2020) Face mask use in the general population and optimal resource allocation during the COVID-19 pandemic. Nature. Communications 11(1). https://doi.org/10.1038/s41467-020-17922-x
World Health Organization (2020) Advice on the use of masks in the community, during home care and in health care settings in the context of the novel coronavirus (2019-nCoV) outbreak: interim guidance, 29 January 2020. https://apps.who.int/iris/handle/10665/330987. Accessed 15 May 2021
World Health Organization (2021) Covid-19 infection prevention and control: living guideline - masks use in the community settings. https://www.who.int/publications/i/item/WHO-2019-nCoV-IPC_masks-2021.1. Accessed 15 May 2022
World Health Organization (2023) WHO Coronavirus (COVID-19) dashboard. https://covid19.who.int/. Accessed 25 March 2023
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions
Author information
Authors and Affiliations
Contributions
ZM conceived and designed the study. ZM and CZ collected data and performed the analysis. CZ wrote the first draft. Both authors revised and agreed upon the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
This observational study undertaken in public did not require approval from the Auckland University of Technology Ethics Committee. Pedestrians observed remained anonymous, and the compilation of the data did not involve any harmful or objectionable activity.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors have no conflict of interest to declare.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 31 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zagreanu, C., Morse, Z. Public face mask use during the COVID-19 pandemic in Auckland, New Zealand. J Public Health (Berl.) (2023). https://doi.org/10.1007/s10389-023-01976-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10389-023-01976-4