Abstract
Aim
Long-term-care facility residents are a vulnerable population who experienced reduced healthcare access during the pandemic. This study aimed to assess the indirect impact of the COVID-19 pandemic, in terms of hospitalisation and mortality rates, among this population in two Italian Regions, Tuscany and Apulia, during 2020 in comparison with the pre-pandemic period.
Subject and methods
We conducted a retrospective cohort study on people residing in long-term-care facilities from 1 January 2018 to 31 December 2020 (baseline period: 1 January 2018–8 March 2020; pandemic period: and 9 March–31 December 2020). Hospitalisation rates were stratified by sex and major disease groups. Standardised weekly rates were estimated with a Poisson regression model. Only for Tuscany, mortality risk at 30 days after hospitalisation was calculated with the Kaplan–Meier estimator. Mortality risk ratios were calculated using Cox proportional regression models.
Results
Nineteen thousand two hundred and fifty individuals spent at least 7 days in a long-term-care facility during the study period. The overall mean non-Covid hospital admission rate per 100 000 residents/week was 144.1 and 116.2 during the baseline and pandemic periods, with a decrease to 99.7 and 77.3 during the first (March–May) and second lockdown (November–December). Hospitalisation rates decreased for all major disease groups. Thirty-day mortality risk ratios for non-Covid conditions increased during the pandemic period (1.2, 1.1 to 1.4) compared with baseline.
Conclusion
The pandemic resulted in worse non-COVID-related health outcomes for long-term-care facilities’ residents. There is a need to prioritise these facilities in national pandemic preparedness plans and to ensure their full integration in national surveillance systems.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
People living within long-term care facilities (LTCFs) typically suffer from multiple long-term conditions, cognitive impairment, and medical and social vulnerabilities (European Centre for Disease Prevention and Control 2021). Due to characteristics of this population and structural or organisational features of the facilities — such as staff working in multiple facilities and high rates of staff turnover (Mukamel et al. 2009) — risks of contracting Covid-19 or developing subsequent severe outcomes, especially before the introduction of the Covid-19 vaccination, were high among LTCF resident population (Giddings et al. 2021; McMichael et al. 2020). In a report published in May 2020 by the European Centre for Disease Prevention and Control (ECDC), it was estimated that deaths among LTCF residents accounted for 37–66% of all Covid-19 related deaths in EU/EEA countries, depending on the country. No data was provided on the Italian LTCF situation (ECDC Public Health Emergency Team 2020).
In Italy, the first confirmed autochthonous cases of Covid-19 were detected in Lombardy, a region in the North of Italy, in late February 2020, with subsequent spread to other regions at different times and rates (Bezzini et al. 2022; Gatto et al. 2020). During the first phase of the pandemic, the real number of Covid-19 cases among LTCF residents was difficult to assess due to the lack of a surveillance system specifically for LTCFs and context and time-specific features (e.g., low or absent testing capacity and undertrained staff (ECDC 2021). To fulfil these gaps, in March 2020, the Italian National Health Institute dedicated a survey to the issue. A dramatic picture emerged from it, with LTCFs reporting high infection rates (Lombardo et al. 2021). In addition, results from studies conducted at the national and local levels in 2020 suggest that the impact of the pandemic in terms of mortality among LTCF residents was large (de Girolamo et al. 2020; Tramarin et al. 2021). In particular, a study evaluating mortality rates of older adults in LTCF across different Italian regions during the first 4 months of 2020 highlighted that risk of death among LTCF residents increased about 4 times during the study period when compared to the same period in the previous years. Moreover, mortality rates of LTCF residents were significantly higher when compared to age-specific mortality rates of the general population (de Girolamo et al. 2020). Another national study highlighted that the Covid-19 incidence rate does not fully explain the differences of mortality impact among different regions (Amore et al. 2021).
Although less broadly investigated, it is expected that people living within LTCFs were also more likely to develop worse health outcomes for non-Covid conditions during the first phase of the pandemic. The non-medical measures enforced by Governments during the pandemic, including dramatic restrictions on individual liberties and prioritisation of healthcare services to reduce risks of system collapse (Bodilsen et al. 2021; Maringe et al. 2020), influenced access to healthcare services and hospital admissions for the entire population. In particular, in Italy, in March 2020, the Government asked regions to postpone outpatient and hospital scheduled activities that were not considered of high priority during the emergency, with a progressive re-activation from June 2020 (Direzione Generale della Programmazione Sanitaria 2020).
As highlighted by a systematic review by Moynihan et al. on 20 countries worldwide, including Italy, such restrictive measures, along with fear of becoming infected or inability to access care, resulted in an overall decrease of one-third of healthcare utilisation by the general population (Moynihan et al. 2021). No information was provided on LTCF resident population.
In the literature, the effects of the pandemic on non-communicable diseases (NCDs) have been extensively studied. In the UK, according to a retrospective cross-sectional study, total admissions and emergency department attendances for selected cardiovascular diseases dropped between 31% and 88% during the first lockdown in 2020 in comparison with 2019 (Ball et al. 2020; Mafham et al. 2020) and excess in acute cardiovascular mortality (+8%) was observed in England and Wales during the first semester of 2020 compared with the expected historical average in the same period of the year (Banerjee et al. 2021; Poon et al. 2020; Wu et al. 2021). Similar results have been observed in the USA, with a national increase in deaths by ischemic heart diseases and hypertensive diseases in the first semester of 2020 compared with 2019 (Wadhera et al. 2021). Further studies conducted worldwide, including in Italy (Cannata et al. 2022; Fondazione GIMBE Bologna 2021), investigating the indirect impact of the pandemic on a vast range of NCDs — especially cardiovascular diseases and cancer — showed similar results, with a decrease in hospital admissions for NCDs and an increase in disease burden after the onset of the pandemic compared to the pre-pandemic period (Gadsden et al. 2022; Mak et al. 2022; Maringe et al. 2020; Pécout et al. 2021; Richards et al. 2020).
Although many studies have examined the impact of the pandemic on NCDs among the general population, investigations on LTCF resident population are scarce. A study conducted among Canadian LTCF residents during the first 6 months of the pandemic, observed that hospital admissions for non-Covid-19 diseases dropped by 27% during the study period in comparison with the same period in 2019, with the largest decrease in hospital transfers for chronic conditions requiring a doctor’s order to seek hospital care, such as heart failure and chronic respiratory conditions, while deaths for all causes increased by 19% in comparison with the average 5-year period (Betini et al. 2021).
Studies on the effects of the pandemic on the utilisation of healthcare services for non-Covid-19 diseases among LTCF residents in Italy are missing, and those on mortality for all causes limited. Availability of health data with regard to residents in LCTFs is limited and largely related to regional areas, as a consequence of decentralisation of healthcare services in the country and the coexistence of private and public LTCFs.
This study is a retrospective cohort study aimed to assess the indirect impact of the COVID-19 pandemic on the health outcomes of LTCFs residents in two Italian regions, Tuscany and Apulia (Central and Southern Italy). Hospital admission and mortality rates among LTCF residents were monitored during the 1st year of the pandemic and in the pre-pandemic period to identify significant changes.
Methods
Demography and healthcare services in the two regions
On 31 December 2020, there were 3,692,865 residents in Tuscany and 3,933,777 residents in Apulia. The distribution by sex was similar (females > 51% in both regions), while population in Tuscany was slighter older (mean age of 47 years in Tuscany and 45.4 in Apulia), with people over 65 representing about 25.7% of the whole population in Tuscany and 23.1% in Apulia. In 2019, people with at least one chronic disease were 40.9% and 40.4% of the population in Tuscany and Apulia, with the most frequent chronic conditions being hypertension (17.2% and 18.8%), arthrosis and arthritis (15.5% and 17.0%), allergic diseases (11.4% and 11.8%) and osteoporosis (7.4% and 9.4%) in both regions, followed by chronic bronchitis for Tuscany (5.4%) and diabetes for Apulia (7.1%) (Osservatorio Nazionale sulla Salute nelle Regioni Italiane 2019).
In the decade before the pandemic, hospital care went through a nationwide reshaping with the aim of increasing appropriateness and safety of care. De-hospitalisation and implementation of community healthcare was at the core of this reorganisation, with reduction in hospitalisations rate and number of hospital beds (Agenzia Regionale di Sanità Toscana 2021). In 2020, the hospital network in Tuscany included 39 public and 21 accredited private care institutions, for a total of 10,254 beds in ordinary inpatient care (2.78 beds per 1.000 inhabitants, lower than the Italian average of 3.1). In Apulia, the network included 33 public and 26 private institutions, for a total of 11,565 beds in ordinary inpatient care and 2.93 beds per 1,000.
In 2019, the standardised rates of hospitalisation for all causes by age and gender per 1,000 inhabitants in Tuscany and Apulia were among the lowest in Italy (120.4 and 114.6 respectively), confirming the downward trend already observed since 2013. The number of beds for non-self-sufficient elderly people in LTCFs in Tuscany was significantly higher than in Apulia in 2016 (146.0 beds compared to 74.2 per 10,000 inhabitants), with the number of residents in LCTFs per 1,000 inhabitants being respectively 13.5 and 7.1. Also, the rate of people over 65 who benefited from home care and community care services per 1,000 inhabitants in 2019 was 32.8 in Tuscany and 19.4 in Apulia (the overall Italian average was 28.1) (Osservatorio Nazionale sulla Salute nelle Regioni Italiane 2019).
Setting and study population
The Italian healthcare system is a regionally based national health service (NHS). The system is organized into three levels: national, regional, and local. The national level is responsible for establishing the general objectives and fundamental principles of the NHS. The regions and autonomous provinces (R&AP) (19 regions and two autonomous provinces) are then responsible for organising and delivering health care (Ferré et al. 2014). In this scenario, the R&AP are in charge of organising the long term-care facilities at the local level based on national guidelines.
Long-term care facilities have been established in Italy in the mid-1990s, after the release in 1989 of a governmental policy act for the creation of residential health care facilities for the elderly (Il Presidente del Consiglio dei Ministri 1989). With the release of two more decrees in 2001 (Il Presidente del Consiglio dei Ministri 2001a), the Government endorsed the role of social protection of the LTCFs, promoting integration between social and health care services within the facilities, and included assistance in LTCFs among those essential services that the NHS guarantees to non-self-sufficient people who do not have the possibility to care for themselves at home (Il Presidente del Consiglio dei Ministri 2001b). LTCFs can be administered by the public (NHS or the municipality) or by the private sector (alone or in affiliation with the NHS). The percentage of LTCFS administered by public or private sector can vary widely among regions.
In 2020, in Tuscany, there were 312 LTCFs with 13,997 beds. Of these facilities, 115 were public and 197 private (Regione Toscana 2013); in Apulia, there were 140 LTCFs with 6,937 beds, of which 97% were administered by the private sector (Italian Ministry of Health 2013). Most private facilities are contracted by the public system that partially subsidise the cost of resident stay. In Italy, the state provides all residents with free and unrestricted access to healthcare (La Camera dei Deputati e Il Senato della Repubblica 1978). Data are recorded prospectively in regional registries, allowing longitudinal surveillance of the entire population. This cohort study included individuals residing in the LTCFs from 1 January 2018 to 31 December 2020. The individuals included in the study were residing for at least 7 consecutive days in the LTCFs of Tuscany and Apulia regions during the study period.
Pandemic stages and preventive measures
In Italy, after the detection of the first locally acquired Covid-19 case in Lombardy on February 20, 2020, the number of cases increased greatly in the following weeks, although unevenly among regions, forcing the government to adopt unprecedented restrictive measures (Il Presidente del Consiglio dei Ministri 2020e, c). In particular, during the first year of the pandemic, the following phases can be defined: (1) first comprehensive national lockdown from 9 March to 3 May (closure of schools and most workplaces, and the implementation of quarantines, border closings, and restriction on public gatherings) (Il Presidente del Consiglio dei Ministri 2020c), (2) gradual reopening phase from 4 May to 14 June (restrictions were gradually rolled back) (Il Presidente del Consiglio dei Ministri 2020d), (3) Few restrictions from 15 June to 7 October (Covid-19 incidence remained low) (Il Presidente del Consiglio dei Ministri 2020a), (4) new restrictions from 8 October to 5 November (Il Presidente della Repubblica 2020), and (5) lockdowns on a regional basis from 6 November until the end of 2020 (closure of regional borders) (Il Presidente del Consiglio dei Ministri 2020b).
The Italian government issued specific provisions aimed at minimising the risk of introducing and transmitting diseases within LTCFs. In particular, with a decree released in April 2020, along with measures regulating the entry of new residents and visits from family members, it was decided to avoid the access of LTCF residents to hospitals as far as possible, even if for specialist visits or diagnostic or therapeutic procedures (Istituto Superiore di Sanità 2020b). In August 2020, the use of telemedicine in delivering care to LTCF residents was promoted, and general practitioners’ access for in-person visits recommended for essential cases only (Istituto Superiore di Sanità 2020a). These national recommendations were endorsed by Tuscany and Apulia, which adapted them to the local context with the implementation of more stringent restrictions if needed.
Due to the fact that Northern Italy was the first and more heavily affected area during the first phase of the pandemic, while Central and Southern Italy were affected later during 2020, our first intention was to select two regions for each area of the country. We asked six Italian regions to participate in the study but only Tuscany and Apulia accepted, due to reported difficulties in using data from the regional registries of people admitted in the public and the contracted private LTCFs.
Data sources and study period
We conducted a retrospective cohort study by analysing and merging two electronic health records from the Tuscany and Apulia health-care information systems: the regional registries of people admitted in the public and the contracted private LTCFs and the regional hospital discharge dataset (≥ 95% of all LTCF beds available). The study period ran from 1 January 2018 to 31 December 2020. We defined the period between 1 January 2018 and 8 March 2020 as the pre-Covid-19 baseline period, and the period between 9 March and 31 December 2020 as the Covid-19 pandemic period.
The regional registries of people admitted in the LTCFs track age, sex, and LTCF admission and discharge dates. For Tuscany only, this data source also provided data on the vital status of LTCF residents. The regional hospital discharge form dataset includes hospital admission and discharge date, sex, and principal diagnosis of discharge coded according to the World Health Organisation’s international classification of diseases version 9 (ICD-9-CM) (National Center for Health Statistics 2015).
Through a numeric identification code, we linked the registries of LTCF residents with the hospital discharge dataset. All the health data used in the study were anonymous administrative health data routinely collected through the regional health information systems.
The study protocol was approved on October 10, 2021, by the Joint Ethical Committee for research of the Scuola Normale Superiore (Pisa, Italy) and the Sant'anna School for Advanced Studies (Pisa, Italy). Number of approval: 39/2021.
Outcomes
From 1 January 2018 to 31 December 2020, all hospital admissions of people residing in LCTFs were identified by principal diagnosis codes in the hospital discharge form. These codes were subsequently grouped according to the multi-level diagnosis clinical classification system (CCS) (Agency for Healthcare Research and Quality 2015) which is based on the ICD-9-CM classification. In 2020, in the ICD-9-CM diagnosis group the category “Covid-19” was added.
Only for people residing in LTCFs in Tuscany, we computed the overall weekly average mortality rate per 1,000 LTCF residents before and after the pandemic, and the 30-day mortality risks for hospital admissions investigated overall and according to major disease groups by pandemic period.
Statistical analysis
We examined overall hospital admission rates stratified by sex and major disease groups. We used a Poisson regression model to estimate standardised weekly hospital admission rates.
We computed hospital admission rate ratios and 95% confidence intervals by using the pre-Covid-19 baseline period (1 January 2018–8 March 2020) as reference. We then repeated the analyses for the two regional study population cohorts.
For the Tuscany region, we assessed mortality risk at 30 days after hospital admission by using the Kaplan–Meier estimator, with censoring at LTCF discharge or end of follow-up whichever occurred first. Mortality risk ratios and 95% confidence intervals were calculated using Cox proportional regression models, and the pre-Covid-19 baseline period (1 January 2018–8 March 2020) as competing risk.
Stata MP version 15 was used for all statistical analysis, and a p-value of 0.05 was applied for testing statistical significance.
Results
A total of 19,250 individuals who spent at least 7 days in a LTCF from 1 January 2018 to 31 December 2020 were included in the study cohort. Of these individuals, 11,806 (median age 87, 28% male) were LTCF residents in Tuscany and 7,444 (median age 84, 29% male) in Apulia. Table 1 shows the weekly average population in the LTCFs in the pre-pandemic period and in the different pandemic phases overall and by region. The number of (non-Covid-19) hospital admission among LTCFs residents in 2018 were 4,883 (3,570 in Tuscany; 1,313 in Apulia), in 2019 were 4,914 (3,667 in Tuscany; 1,247 in Apulia), and in 2020 were 3,456 (2,583 in Tuscany; 873 in Apulia). During the study period, the median age of individuals hospitalised was 85 in Tuscany and 83 in Apulia.
Hospital admission rates
The overall mean non-Covid-19 hospital admission rate was 144.1 (198.4 males; 123.2 females) per 100,000 LCTF residents/week during the baseline period and 116.2 (138.9 males; 82.5 females) per 100,000/week during the pandemic period (Fig. 1). The overall mean non-Covid-19 hospital admission rate was 155.8 in Tuscany and 114.5 in Apulia during the baseline period, and 123.5 in Tuscany and 56.8 in Apulia during the pandemic period (Supplemental material Table e1 and Table e2). The mean hospital admission rate for non-Covid-19 conditions decreased to 99.7 (rate ratio 0.7; 95% confidence interval (95% CI: 0.6 to 0.8)) during the first national lockdown, 92.1 (0.6; 95% CI: 0.6 to 0.7) during the gradual reopening phase, 108.9 (0.8; 95% CI: 0.7 to 0.8) during the period with few restrictions, 90.1 (0.6; 95% CI: 0.5 to 0.7) during the period with new restrictions, and 77.3 (0.5; 95% CI: 0.5 to 0.6) during regional lockdown phase. The mean hospital admission rate for non-Covid-19 conditions in men decreased to 149.6 (0.8; 95% CI: 0.7 to 0.9) during the first national lockdown, 121.7 (0.6; 95% CI: 0.5 to 0.7) during the gradual reopening phase, 153.3 (0.8; 95% CI: 0.7 to 0.9) during the period with few restrictions, 133.2 (0.7; 95% CI: 0.5 to 0.8) during the period with new restrictions, and 109.5 (0.6; 95% CI: 0.5 to 0.7) during the regional lockdown phase (Supplemental material Fig. 2.A). In female LTCF residents, the mean hospital admission rate for non-Covid-19 conditions decreased to 80.7 (0.7; 95% CI: 0.6 to 0.7) during the first national lockdown, 85.3 (0.7, 0.6 to 0.8) during the gradual reopening phase, 91.6 (0.7; 95% CI: 0.7 to 0.8) during the period with few restrictions, 73.3 (0.6; 95% CI: 0.5 to 0.7) during the period with new restrictions, and 64.2 (0.5; 95% CI: 0.4 to 0.6) during regional lockdown phase (Supplemental material Fig. 2.B) (Table 2). Similar results were obtained when the analysis was repeated by region (Supplemental material Tables 1 and 2).
Hospital admission rates for major disease groups
For all other major diagnosis groups, the hospital admission rate decreased markedly during the pandemic period compared with the baseline period. The decreased rate remained statistically significant in all the pandemic phases only for hospital admission with a cardiovascular disease, endocrine, nutrition, and metabolism diseases and respiratory diseases diagnosis (Table 2, Fig. 2).
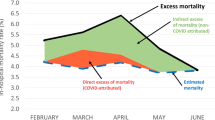
Mortality among LTCF residents in Tuscany
The overall weekly average mortality rate for 1,000 LTCF residents in Tuscany was 8.9 before the start of the pandemic, and 12.5 during the pandemic. The proportion of deaths at 30 days after hospitalisation was 40.3% in the pre-pandemic period, and decreased to 34.5% in the pandemic period, excluding Covid-19 related hospitalisation. The overall 30-day mortality risk ratios among people admitted to hospital for non-Covid-19 causes increased during the first national lockdown (1.4, 1.2 to 1.7), during the period with new restrictions (1.5, 1.2 to 1.9), and during the regional lockdown (1.5, 1.2 to 1.9) compared with the pre-pandemic baseline period. The increase in mortality risk was higher among males than females for the first pandemic phases, while we have the opposite scenario in the last reported pandemic phases (Table 3).
Discussion
Although there is extensive literature describing Covid-19 outbreaks in LTCFs and the excess mortality that occurred during the pandemic (ECDC Public Health Emergency Team 2020; de Girolamo et al. 2020; Thompson et al. 2020), to our knowledge this is the first attempt to extensively study the indirect impact of the Covid-19 pandemic on hospital care provided to LTCFs residents in Europe.
Here, we analysed regional health registers that include residents of LTCFs in Tuscany and Apulia and observed a lower overall hospitalisation rate during the1st year of the pandemic compared with the pre-pandemic period, combined with an increased risk of mortality within 30 days of hospital admission.
During the study period, we observe that the weekly average population of the LTCFs gradually decreased, and this is in line with the Ministry of Health's recommendations (Istituto Superiore di Sanità 2020b) to limit new admissions of residents to urgent and unavoidable cases, in order to allow for a reduction in the number of residents to facilitate management of Covid-19 cases in isolation. In these recommendations, it is suggested to avoid sending residents to hospitals for specialist visits and instrumental examinations as much as possible.
This may be one of the reasons why, in our study, we observe a significant reduction in hospital admission rate during the pandemic period compared to the previous 2 years. This reduction has also been reported in the general population in Italy as in other countries (Kalanj et al. 2021; Boldrini et al. 2021, Rennert-May et al. 2021; Shah et al. 2022; Spadea et al. 2021). Furthermore, our results are in line with the findings of Betini et al., who reported a drop by 27% of LTCF resident transfers to hospitals for the treatment of chronic conditions and infections (Betini et al. 2021).
According to our results, the decrease in the admission rate is particularly pronounced in the second epidemic wave. This may be due to the fact that, although the hospitals were better prepared, the second epidemic wave was more extensive than the first (Italian National Institute of Health (Istituto Superiore di Sanità) 2020). Moreover, teams of healthcare workers periodically accessed the LTCFs to deal mainly with Covid-19 patients, allowing the nursing home staff and general practitioners who periodically visit the facilities to devote themselves to other patients (Istituto Superiore di Sanità 2020b).
The magnitude of the reduction in the hospitalisation rate for the major disease groups was homogenous (around 30–40%) if we compare the pre-pandemic period with the pandemic period as a whole. In specific periods, the reduction in the rate of hospitalisation for specific diseases was more pronounced. For instance, for neoplasms during the first lock-down the reduction in hospitalisation rates is about 80%, about twice the reduction reported for the same period in the Italian population (Spadea et al. 2021). The two Italian regions in our study have different hospitalisation rates for both the baseline and pandemic periods. In particular, the Apulia region reported lower hospitalisation rates and has experienced a more drastic reduction in access to hospital during the pandemic. This may be due to various factors: the healthcare provided in LTCFs may be dissimilar in the two regions, or criteria for hospitalisation may be different. Further studies are needed for a proper understanding of the reasons behind these differences as well as a harmonisation of data collection systems.
During the pandemic period, the mortality risk at 30 days after non-Covid-19 hospital admission increased by about 20%, higher when compared to age-specific mortality rates of the general population (Dorrucci et al. 2021), and this is consistent with what previous studies have reported (Berloto et al. 2020; Betini et al. 2021; Kalanj et al. 2021; Sepulveda et al. 2020).
Even before the crisis, the Italian LTCFs were characterized by weaknesses, due to a strong level of fragmentation both in terms of competencies among institutional and non-institutional actors, and unheard struggles to enter the policymakers’ agenda. LTCFs were not conceived and developed as a comprehensive model, rather they emerged from multiple legislative interventions that aimed intermittently at integrating what existed already (Berloto et al. 2020). LTCF governance structure is, at the central level, somewhere in the middle between the Ministry for Labour and Social Policy and the Ministry of Health.
Moreover, R&AP implement the dual ministerial policies by organising the LTCFs at the local level, defining the network of services; ultimately, local health authorities and municipalities manage services and interventions at the local and individual level. This fragmented situation is further compromised by the insufficient level of coordination that exists among all the actors involved in LTCFs: the absence of national awareness and lack of strategic vision inevitably inhibits dialogue, cooperation, and joint actions even in non-crisis times. This fragmentation also affects the information monitoring system, which is not integrated with national health data collection systems and is heterogeneous among regions, as evidenced by the fact that four out of the six regions that were invited to participate in the study declined because of low quality of data. However, although imperfect, these registers are available at regional level. Using them allows us not only to evaluate the health care performance of LTCFs, but also to advocate for the development of unified and comparable data collection systems across regions.
Limits
This study has limitations. First, while we acknowledge that data regarding age-specific mortality, comorbidities, and cause of death of older residents would allow a more detailed assessment of the indirect impact of COVID-19 pandemic in LTCFs, we decided not to further stratify by age groups in order to increase accuracy of estimates. Second, the epidemic burden and organisation of LTCFs differ among Italian regions; therefore, it is not possible to translate our findings into the Italian context. Finally, we have no information on the type of LTCFs in which the subjects reside. This does not allow us to assess whether there are differences between privately and publicly managed LTCFs that might have had implications on the outcome during the Covid-19 pandemic.
Conclusion
The Covid-19 pandemic had strong direct and indirect impact on LTCFs. They are vulnerable places for structural reasons and because of the residents’ characteristics; therefore, LTCFs need to be prioritized in pandemic preparedness plans.
In addition to the pandemic, it is important to monitor LTCFs potential threats and health performance. This implies integrating LTCF health registries within national surveillance and implementing possible sentinel sites for syndromic surveillance for early warning. These registries are available, and can be harmonised among regions and used to build a monitoring system against key indicators reflecting healthcare quality, but also to ensure appropriate use of the health system resources, including access to specialised services and hospitalisation.
Data availability
Data can be obtained upon request. Requests should be directed towards the corresponding author by email (giudittascardina77@gmail.com). Due to restrictions based on privacy regulations, data can not be made freely available in a public repository.
Code availability
Not applicable.
References
Agency for Healthcare Research and Quality (2015) Clinical Classifications Software (CCS) for ICD-9-CM. Agency for Healthcare Research and Quality, Rockville, MD, USA. https://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp. Accessed 23 Sept 2022
Agenzia Regionale di Sanità Toscana (2021) Welfare e salute in Toscana. Agenzia Regionale di Sanità Toscana, Florence, Italy. https://www.ars.toscana.it/images/pubblicazioni/Collana_ARS/2021/welfare_e_salute/Libro_WS_1_def.pdf
Amore S, Puppo E, Melara J, Terracciano E, Gentili S et al (2021) Impact of COVID-19 on older adults and role of long-term care facilities during early stages of epidemic in Italy. Scientific Reports 11:12530. https://doi.org/10.1038/s41598-021-91992-9
Ball S, Banerjee A, Berry C, Boyle JR, Bray B et al (2020) Monitoring indirect impact of COVID-19 pandemic on services for cardiovascular diseases in the UK. Heart 106(24):1890–1897. https://doi.org/10.1136/heartjnl-2020-317870
Banerjee A, Chen S, Pasea L, Lai AG, Katsoulis M et al (2021) Excess deaths in people with cardiovascular diseases during the COVID-19 pandemic. Eur J Prevent Cardiol 28(14):1599–1609. https://doi.org/10.1093/eurjpc/zwaa155
Berloto S, Notarnicola E, Perobelli E, Rotolo A (2020) Italy and the COVID-19 long-term care situation. International Long Term Care Policy Network. Country report in LTCcovid.org, International Long Term Care Policy Network, CPEC-LSE. https://ltccovid.org/wp-content/uploads/2020/04/LTC-COVID19-situation-in-Italy-22-April-2020.pdf. Accessed 23 Sept 2022
Betini R, Milicic S, Lawand C (2021) The impact of the COVID-19 pandemic on long-term care in Canada. Healthc Q 24(3):13–15. https://doi.org/10.12927/hcq.2021.26625
Bezzini D, Schiavetti I, Manacorda T, Franzone G, Battaglia MA (2022) First wave of COVID-19 pandemic in Italy: data and evidence. In: Asea AAA, Kaur P (eds) Coronavirus therapeutics, vol II. Springer, Cham, pp 91–113
Bodilsen J, Nielsen PB, Søgaard M, Dalager-Pedersen M, Speiser LOZ et al (2021) Hospital admission and mortality rates for non-Covid diseases in Denmark during Covid-19 pandemic: nationwide population based cohort study. BMJ 373:n1135. https://doi.org/10.1136/bmj.n1135
Boldrini T, Girardi P, Clerici M et al (2021) Consequences of the COVID-19 pandemic on admissions to general hospital psychiatric wards in Italy: reduced psychiatric hospitalizations and increased suicidality. Prog Neuropsychopharmacol Biol Psychiatry. 110:110304. https://doi.org/10.1016/j.pnpbp.2021.110304
Cannata A, Watson SA, Daniel A, Giacca M, Shah AM et al (2022) Impact of the COVID-19 pandemic on in-hospital mortality in cardiovascular disease: a meta-analysis. Eur J Prev Cardiol 29(8):1266–1274. https://doi.org/10.1093/eurjpc/zwab119
de Girolamo G, Bellelli G, Bianchetti A, Starace F, Zanetti O et al (2020) Older people living in long-term care facilities and mortality rates during the COVID-19 pandemic in Italy: preliminary epidemiological data and lessons to learn. Front Psychiat 11(October):1–7. https://doi.org/10.3389/fpsyt.2020.586524
Direzione Generale della Programmazione Sanitaria (2020) Linee di indirizzo per la rimodulazione dell’attività programmata differibile in corso di emergenza da COVID-19. Ministero Della Salute, Rome. https://s3-eu-west-1.amazonaws.com/img.web.mdsnet.it/fism/allegati_upload_file/5fa3b0e09bef1_All.%20Linee%20indirizzo%20attivit%C3%A0%20programmata%20differibile_strutture%20intermedie.pdf. Accessed 23 Sept 2022
Dorrucci M, Minelli G, Boros S, Manno V, Prati S et al (2021) Excess mortality in Italy during the COVID-19 pandemic: assessing the differences between the first and the second wave, year 2020. Front Public Health 9(July):1–9. https://doi.org/10.3389/fpubh.2021.669209
ECDC Public Health Emergency Team, Danis K, Fonteneau L, Georges S, Daniau C, Bernard-Stoecklin S, Domegan L, O’Donnell J, Hauge Siri H, Dequeker S, Vandael E, Van der Heyden J, Renard F, Sierra N B, Ricchizzi E, Schweickert B, Schmidt N, Abu Sin M, Eckmanns T, Paiva JA, Schneider E (2020) High impact of COVID-19 in long-term care facilities, suggestion for monitoring in the EU/EEA, May 2020. EuroSurveill 25(22):2000956. https://doi.org/10.2807/1560-7917.ES.2020.25.22.2000956
European Centre for Disease Prevention and Control (2021) Surveillance of COVID-19 in long-term care facilities in the EU / EEA (Issue November). European Centre for Disease Prevention and Control, Solna, Sweden. https://www.ecdc.europa.eu/en/publications-data/surveillance-COVID-19-long-term-care-facilities-EU-EEA. Accessed 23 Sept 2022
Ferré F, de Belvis AG, Valerio L, Longhi S, Lazzari A et al (2014) Italy: Health system review. Health Syst Trans 16(4):1–166
Fondazione GIMBE Bologna (2021) Report Osservatorio GIMBE 1/2021 Impatto della pandemia COVID-19 sull’erogazione di prestazioni sanitarie. Fondazione GIMBE, Bologna. https://www.gimbe.org/osservatorio/Report_Osservatorio_GIMBE_2021.01_Impatto_COVID_19_prestazioni_sanitarie.pdf. Accessed 23 Sept 2022
Gadsden T, Downey LE, Vilas VDR, Peiris D, Jan S (2022) The impact of COVID-19 on essential health service provision for noncommunicable diseases in the South-East Asia region: a systematic review. Lancet Reg Health Southeast Asia 1:100010. https://doi.org/10.1016/j.lansea.2022.04.006
Gatto M, Bertuzzo E, Mari L, Miccoli S, Carraro L et al (2020) Spread and dynamics of the COVID-19 epidemic in Italy: Effects of emergency containment measures. Proc Natl Acad Sci USA 117(19):10484–10491. https://doi.org/10.1073/pnas.2004978117
Giddings R, Krutikov M, Palmer T, Fuller C, Azmi B et al (2021) Changes in COVID-19 outbreak severity and duration in long-term care facilities following vaccine introduction, England, November 2020 to June 2021. Eurosurveillance 26(46):1–9. https://doi.org/10.2807/1560-7917.ES.2021.26.46.2100995
Il Presidente del Consiglio dei Ministri (1989) Atto di indirizzo e coordinamento dell’attivita’ amministrativa delle regioni e province autonome concernente la realizzazione di strutture sanitarie residenziali per anziani non autosufficienti non assistibili a domicilio o nei servizi semiresidenziali. Gazzetta Ufficiale Della Repubblica Italiana
Il Presidente del Consiglio dei Ministri (2001a) Atto di indirizzo e coordinamento in materia di prestazioni socio-sanitarie. Gazzetta Ufficiale Della Repubblica Italiana
Il Presidente del Consiglio dei Ministri (2001b) Definizione dei livelli essenziali di assistenza. Gazzetta Ufficiale Della Repubblica Italiana
Il Presidente del Consiglio dei Ministri (2020a) DECRETO DEL PRESIDENTE DEL CONSIGLIO DEI MINISTRI 11 giugno 2020. Ulteriori disposizioni attuative del decreto-legge 23 febbraio 2020, n. 6, recante misure urgenti in materia di contenimento e gestione dell’emergenza epidemiologica da COVID-19. Gazzetta Ufficiale Della Repubblica Italiana. https://www.gazzettaufficiale.it/eli/id/2020/06/11/20A03194/sg
Il Presidente del Consiglio dei Ministri (2020b) DECRETO DEL PRESIDENTE DEL CONSIGLIO DEI MINISTRI 11 giugno 2020 Ulteriori disposizioni attuative del decreto-legge 25 marzo 2020, n. 19, recante misure urgenti per fronteggiare l’emergenza epidemiologica da COVID-19, e del decreto-legge 16 maggio 2020, n. Gazzetta Ufficiale Della Repubblica Italiana. https://www.gazzettaufficiale.it/eli/id/2020/06/11/20A03194/sg
Il Presidente del Consiglio dei Ministri (2020c) DECRETO DEL PRESIDENTE DEL CONSIGLIO DEI MINISTRI 11 marzo 2020. Ulteriori disposizioni attuative del decreto-legge 23 febbraio 2020, n. 6, recante misure urgenti in materia di contenimento e gestione dell’emergenza epidemiologica da COVID-19. Gazzetta Ufficiale Della Repubblica Italiana. https://www.gazzettaufficiale.it/eli/id/2020/03/11/20A01605/sg
Il Presidente del Consiglio dei Ministri (2020d) DECRETO DEL PRESIDENTE DEL CONSIGLIO DEI MINISTRI 26 aprile 2020. Ulteriori disposizioni attuative del decreto-legge 23 febbraio 2020, n. 6, recante misure urgenti in materia di contenimento e gestione dell’emergenza epidemiologica da COVID-19. Gazzetta Ufficiale Della Repubblica Italiana. https://www.gazzettaufficiale.it/eli/id/2020/04/27/20A02352/sg
Il Presidente del Consiglio dei Ministri (2020e) DECRETO DEL PRESIDENTE DEL CONSIGLIO DEI MINISTRI 8 marzo 2020. Ulteriori disposizioni attuative del decreto-legge 23 febbraio 2020, n. 6, recante misure urgenti in materia di contenimento e gestione dell’emergenza epidemiologica da COVID-19. Gazzetta Ufficiale Della Repubblica Italiana. https://www.gazzettaufficiale.it/eli/id/2020/03/08/20A01522/sg
Il Presidente della Repubblica (2020) Misure urgenti connesse con la proroga della dichiarazione dello stato di emergenza epidemiologica da COVID-19 e per la continuita’ operativa del sistema di allerta COVID, nonche’ per l’attuazione della direttiva (UE) 2020/739 del 3 giugno 2020. Gazzetta Ufficiale Della Repubblica Italiana. https://www.trovanorme.salute.gov.it/norme/dettaglioAtto?id=76574
Istituto Superiore di Sanità (2020a) Indicazioni ad interim per la prevenzione e il controllo dell’ infezione da SARS-COV-2 in strutture residenziali sociosanitarie (Versione 24 agosto 2020). Istituto Superiore di Sanità, Rome. https://www.iss.it/documents/20126/0/Rapporto+ISS+COVID-19+n.+4-2020_Rev.+2+%281%29.pdf/54f1745b-adef-935d-9b2a-09e875b14481?t=1599152636882. Accessed 23 Sept 2022
Istituto Superiore di Sanità (2020b) Indicazioni ad interim per la prevenzione ed il controllo dell’infezione da SARS- COV-2 in strutture residenziali e sociosanitarie (Versione del 17 aprile 2020). Istituto Superiore di Sanità, Rome. https://www.epicentro.iss.it/coronavirus/pdf/rapporto-covid-19-4-2020.pdf. Accessed 23 Sept 2022
Italian Ministry of Health (2013) L’offerta assistenziale per anziani e disabili in Puglia. . Italian Ministry of Health, Rome. Accessed 23 Sept 2022
Italian National Institute of Health (Istituto Superiore di Sanità) (2020) Epidemia COVID-19 Aggiornamento nazionale 29 dicembre 2020 – ore 12.00.Istituto Superiore di Sanità, Rome. https://www.epicentro.iss.it/coronavirus/bollettino/Bollettino-sorveglianza-integrata-COVID-19_29-dicembre-2020.pdf. Accessed 23 Sept 2022
Kalanj K, Marshall R, Karol K, Tiljak MK, Orešković S (2021) The impact of COVID-19 on hospital admissions in Croatia. Front Public Health 9(September):1–11. https://doi.org/10.3389/fpubh.2021.720948
La Camera dei Deputati e Il Senato della Repubblica (1978) Istituzione del Servizio Sanitario Nazionale. Gazzetta Ufficiale Della Repubblica Italiana
Lombardo FL, Bacigalupo I, Salvi E, Lacorte E, Piscopo P et al (2021) The Italian national survey on Coronavirus disease 2019 epidemic spread in nursing homes. Int J Geriatric Psychiat 36(6):873–882. https://doi.org/10.1002/gps.5487
Mafham MM, Spata E, Goldacre R, Gair D, Curnow P et al (2020) COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet 396(10248):381–389. https://doi.org/10.1016/S0140-6736(20)31356-8
Mak IL, Wan EYF, Wong TKT, Lee WWJ, Chan EWY et al (2022) The spill-over impact of the novel Coronavirus-19 pandemic on medical care and disease outcomes in non-communicable diseases: a narrative review. Public Health Rev 43:1604121. https://doi.org/10.3389/phrs.2022.1604121
Maringe C, Spicer J, Morris M, Purushotham A, Nolte E et al (2020) The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol 21(8):1023–1034. https://doi.org/10.1016/S1470-2045(20)30388-0
McMichael TM, Currie DW, Clark S, Pogosjans S, Kay M et al (2020) Epidemiology of Covid-19 in a long-term care facility in King County, Washington. N Engl J Med 382(21):2005–2011. https://doi.org/10.1056/nejmoa2005412
Moynihan R, Sanders S, Michaleff ZA, Scott AM, Clark J et al (2021) Impact of COVID-19 pandemic on utilisation of healthcare services: A systematic review. BMJ Open 11(3):11–17. https://doi.org/10.1136/bmjopen-2020-045343
Mukamel DB, Spector WD, Limcangco R, Wang Y, Feng Z et al (2009) The costs of turnover in nursing homes. Med Care 47(10):1039–1045. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2761533/
National Center for Health Statistics (2015) ICD-9-CM Addenda, conversion table, and guidelines. National Center for Health Statistics, Hyattsville, MD, USA. https://www.cdc.gov/nchs/icd/icd9cm_addenda_guidelines.htm. Accessed 23 Sept 2022
Osservatorio Nazionale sulla Salute nelle Regioni Italiane. Rapporto OsservaSalute (2019) Stato di salute e qualità dell'assistenza nelle regioni italiane. Osservatorio Nazionale sulla Salute nelle Regioni Italiane, Rome. https://osservatoriosullasalute.it/osservasalute/rapporto-osservasalute-2019
Pécout C, Pain E, Chekroun M, Champeix C, Kulak C et al (2021) Impact of the Covid-19 pandemic on patients affected by non-communicable diseases in Europe and in the USA. Int J Environ Res Public Health 18(13):6697. https://doi.org/10.3390/ijerph18136697
Poon MTC, Brennan PM, Jin K, Figueroa JD, Sudlow CLM (2020) Tracking excess deaths (TRACKED) — an interactive online tool to monitor excess deaths associated with the COVID-19 pandemic in the United Kingdom. Wellcome Open Res 5:168. https://doi.org/10.12688/wellcomeopenres.16058.2
Regione Toscana (2013) Non autosufficienza, i dati della Toscana. Regione Toscana, Florence https://www.toscana-notizie.it/documents/735693/23079821/Non autosufficenza, tutti i numeri della Toscana.pdf/c0c0c764-0a91-43fc-978b-666f0854c84b. Accessed 23 Sept 2022
Rennert-May E, Leal J, Thanh NX, Lang E, Dowling S et al (2021) The impact of COVID-19 on hospital admissions and emergency department visits: a population-based study. PLoS ONE 16(6):e0252441. https://doi.org/10.1371/journal.pone.0252441
Richards M, Anderson M, Carter P, Ebert BL, Mossialos E (2020) The impact of the COVID-19 pandemic on cancer care. Nat Cancer 1(6):565–567. https://doi.org/10.1038/s43018-020-0074-y
Sepulveda ER, Stall NM, Sinha SK (2020) A comparison of COVID-19 mortality rates among long-term care residents in 12 OECD countries. J Am Med Direct Assoc 21(11):1572–1574.e3. https://doi.org/10.1016/j.jamda.2020.08.039
Shah SA, Brophy S, Kennedy J, Fisher L, Walker A et al (2022) Impact of first UK COVID-19 lockdown on hospital admissions: Interrupted time series study of 32 million people. EClinicalMedicine 49:101462. https://doi.org/10.1016/j.eclinm.2022.101462
Spadea T, Di Girolamo C, Landriscina T, Leoni O, Forni S et al (2021) Indirect impact of Covid-19 on hospital care pathways in Italy. Scientific Reports 11(1):21526. https://doi.org/10.1038/s41598-021-00982-4
Thompson DC, Barbu MG, Beiu C, Popa LG, Mihai MM et al (2020) The impact of COVID-19 pandemic on long-term care facilities worldwide: an overview on international issues. Biomed Res Int 2020:8870249. https://doi.org/10.1155/2020/8870249
Tramarin A, Gennaro N, Dal Grande G, Bragagnolo L, Carta MR et al (2021) The impact of COVID-19 first wave on long term care facilities of an Italian province: an historical reference. Geriatric Care 7(1):29–33. https://doi.org/10.4081/gc.2021.9654
Wadhera RK, Shen C, Gondi S, Chen S, Kazi DS et al (2021) Cardiovascular deaths during the COVID-19 pandemic in the United States. J Am College Cardiol 77(2):159–169. https://doi.org/10.1016/j.jacc.2020.10.055
Wu J, Mamas MA, Mohamed MO, Kwok CS, Roebuck C et al (2021) Place and causes of acute cardiovascular mortality during the COVID-19 pandemic. Heart 107(2):113–119. https://doi.org/10.1136/heartjnl-2020-317912
Funding
Open access funding provided by Università di Pisa within the CRUI-CARE Agreement. No funding was required to perform this study.
Author information
Authors and Affiliations
Contributions
SM, GS, FC, SF, and LT conceived the study and developed the study protocol.
SM and GS performed data analysis and results interpretation in consultation with FC, SF, GB, FG, and LT. SM and GS drafted the manuscript in collaboration with GG and LT. FC, SF, LB, PL, AC, GO, NV, GB, FG, and LT provided expert insights and contributed to manuscript drafting. All authors read, revised, and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study received the approval of the Joint Ethical Committee for research of the Scuola Normale Superiore (Pisa, Italy) and the Sant'anna School for Advanced Studies (Pisa, Italy) on October 10, 2021. Number of approval: 39/2021.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflicts of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 201 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mazzilli, S., Scardina, G., Collini, F. et al. Hospital admission and mortality rates for non-Covid diseases among residents of the long-term care facilities before and during the pandemic: a cohort study in two Italian regions. J Public Health (Berl.) (2023). https://doi.org/10.1007/s10389-023-01925-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10389-023-01925-1