Abstract
Aim
Depression is one of the most common mental disorders and affects many people around the world. Studies show different and conflicting prevalence rates in Iran. This study aimed to investigate the prevalence and associated risk factors for depression in the Prospective Epidemiological Research Studies of the Iranian Adults (PERSIAN) Guilan cohort study (PGCS).
Subject and methods
In this cross-sectional study, the population consisted of 10,520 individuals aged 35–70 years in the PGCS (Sowme’eh Sara, Guilan, Iran), which was conducted in 2014–2017. Demographic, anthropometric, and self-report depression data were used, and statistical analysis was performed using SPSS version 16.0 software.
Results
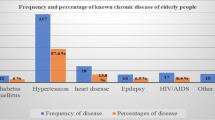
The prevalence of depression was 5.2% in this study and was more prevalent in women than in men (7.3% vs. 2.8%). According to the adjusted analysis, depression was significantly associated with female gender, being divorced, being unemployed, higher educational level, less physical activity, and presence of a chronic disease.
Conclusion
Pre-existence of underlying disease is likely to be the greatest risk factor associated with higher prevalence of depression. In light of these findings, there is a need to improve evidence-based and suitable community-based primary and secondary psychological health prevention programs.

Similar content being viewed by others
Data availability
All data and tables used in the manuscript were prepared originally by the authors and are available from the corresponding author on reasonable request.
Code availability
Not applicable.
References
Abe Y, Fujise N, Fukunaga R, Nakagawa Y, Ikeda M (2012) Comparisons of the prevalence of and risk factors for elderly depression between urban and rural populations in Japan. Int Psychogeriatr 24:1235–1241
Adib-Hajbaghery M, Aghahoseini S (2007) The evaluation of disability and its related factors among the elderly population in Kashan, Iran. BMC Public Health 7:261
Akhtar-Danesh N, Landeen J (2007) Relation between depression and sociodemographic factors. Int J Ment Heal Syst 1:4
Arias-de la Torre J, Vilagut G, Ronaldson A, Serrano-Blanco A, Martín V, Peters M, Valderas JM, Dregan A, Alonso J (2021) Prevalence and variability of current depressive disorder in 27 European countries: a population-based study. Lancet Public Health 6:e729–e738
Badillo N, Khatib M, Kahar P, Khanna D (2022) Correlation Between Body Mass Index and Depression/Depression-Like Symptoms Among Different Genders and Races. Cureus 14:e21841
Bjelland I, Krokstad S, Mykletun A, Dahl AA, Tell GS, Tambs K (2008) Does a higher educational level protect against anxiety and depression? The HUNT study. Social Sci Med (1982) 66:1334–1345
Choi KW, Chen CY, Stein MB, Klimentidis YC, Wang MJ, Koenen KC, Smoller JW (2019) Assessment of Bidirectional Relationships Between Physical Activity and Depression Among Adults: A 2-Sample Mendelian Randomization Study. JAMA Psychiat 76:399–408
Cohen AK, Nussbaum J, Weintraub MLR, Nichols CR, Yen IH (2020) Association of Adult Depression With Educational Attainment, Aspirations, and Expectations. Prev Chronic Dis 17:E94
Dreimüller N, Lieb K, Tadić A, Engelmann J, Wollschläger D, Wagner S (2019) Body mass index (BMI) in major depressive disorder and its effects on depressive symptomatology and antidepressant response. J Affect Disord 256:524–531
Fernandez-Montero A, Moreno-Galarraga L, Sánchez-Villegas A, Lahortiga-Ramos F, Ruiz-Canela M, Martínez-González M, Molero P (2020) Dimensions of leisure-time physical activity and risk of depression in the "Seguimiento Universidad de Navarra" (SUN) prospective cohort. BMC Psychiat 20:98
Freeman EW (2002) Treatment of depression associated with the menstrual cycle: premenstrual dysphoria, postpartum depression, and the perimenopause. Dialogues Clin Neurosci 4:177–191
Freeman A, Tyrovolas S, Koyanagi A, Chatterji S, Leonardi M, Ayuso-Mateos JL, Tobiasz-Adamczyk B, Koskinen S, Rummel-Kluge C, Haro JM (2016) The role of socio-economic status in depression: results from the COURAGE (aging survey in Europe). BMC Public Health 16:1098
García-Esquinas E, Ortolá R, Galán I, Soler-Vila H, Laclaustra M, Rodríguez-Artalejo F (2018) Moderate alcohol drinking is not associated with risk of depression in older adults. Sci Rep 8:11512
Gémes K, Forsell Y, Janszky I, László KD, Lundin A, Ponce De Leon A, Mukamal KJ, Moller J (2019) Moderate alcohol consumption and depression - a longitudinal population-based study in Sweden. Acta Psychiatr Scand 139:526–535
Gharraee B, Zahedi Tajrishi K, Sheybani F, Tahmasbi N, Mirzaei M, Farahani H, Naserbakht M (2019) Prevalence of major depressive disorder in the general population of Iran: A systematic review and meta-analysis. Med J Islam Repub Iran 33:151
(GHDx), GHDE (2019) Institute of Health Metrics and Evaluation
Girgus JS, Yang K (2015) Gender and depression. Curr Opin Psychol 4:53–60
Handley TE, Inder KJ, Kay-Lambkin FJ, Stain HJ, Fitzgerald M, Lewin TJ, Attia JR, Kelly BJ (2012) Contributors to suicidality in rural communities: beyond the effects of depression. BMC Psychiat 12:105
Hossain HUAD, Aftab A, Soron TR, Alam MT, Chowdhury MWA, Uddin A (2017) Suicide and depression in the World Health Organization South-East Asia region: A systematic review. WHO South-East Asia J Public Health 6:60–66
Jaafari Z, Sadidi N, Abdolahinia Z, Shahesmaeili A (2022) Prevalence of Depression among Iranian Patients with Beta-Thalassemia Major: A Systematic Review and Meta-analysis. Iranian J Med Sci 47:15
Jahangir S, Adjepong D, Al-Shami HA, Malik BH (2020) Is There an Association Between Migraine and Major Depressive Disorder? A Narrative Review. Cureus 12:e8551
Kandola A, Ashdown-Franks G, Hendrikse J, Sabiston CM, Stubbs B (2019) Physical activity and depression: Towards understanding the antidepressant mechanisms of physical activity. Neurosci Biobehav Rev 107:525–539
Kuehner C (2017) Why is depression more common among women than among men? Lancet Psychiatry 4:146–158
Levecque K, Anseel F, De Beuckelaer A, Van der Heyden J, Gisle L (2017) Work organization and mental health problems in PhD students. Res Policy 46:868–879
Lim GY, Tam WW, Lu Y, Ho CS, Zhang MW, Ho RC (2018) Prevalence of Depression in the Community from 30 Countries between 1994 and 2014. Sci Rep 8:2861
Liu Y, Tang X (2018) Depressive Syndromes in Autoimmune Disorders of the Nervous System: Prevalence, Etiology, and Influence. Front Psychiat 9:451
Llorente JM, Oliván-Blázquez B, Zuñiga-Antón M, Masluk B, Andrés E, García-Campayo J, Magallón-Botaya R (2018) Variability of the Prevalence of Depression in Function of Sociodemographic and Environmental Factors: Ecological Model. Front Psychol 9:2182
Mahmudi L, Karimi P, Arghavan FS, Shokri M, Badfar G, Kazemi F, Azami M (2021) The prevalence of depression in Iranian children: A systematic review and meta-analysis. Asian J Psychiatr 58:102579
Mansour-Ghanaei F, Joukar F, Naghipour MR, Sepanlou SG, Poustchi H, Mojtahedi K, Balou HA, Heidarzadeh A, Malekzadeh R (2019) The PERSIAN Guilan Cohort Study (PGCS). Arch Iranian Med 22:39–45
Martín-Merino E, Ruigómez A, Johansson S, Wallander MA, García-Rodriguez LA (2010) Study of a cohort of patients newly diagnosed with depression in general practice: prevalence, incidence, comorbidity, and treatment patterns. Prim Care Companion J Clin Psychiat 12:PCC.08m00764
Mirzaie M, Darabi S (2017) Population aging in Iran and rising health care costs. Iranian J Ageing 12:156–169
Modabernia MJ, Tehrani HS, Fallahi M, Shirazi M, Modabbernia AH (2008) Prevalence of depressive disorders in Rasht, Iran: A community based study. Clin Pract Epidemiol Ment Health 4:1–6
Mohammadi M, Rahgozar M, Bagheri Yazdi S, Mesgarpour B, Khalkhali M, Farsi M, Sharafati M (2004) An epidemiological study of psychiatric disorders in Guilan province (year 2001). J Guilan Univ Med Sci 13:55–66
Moledina SM, Bhimji KM, Manji KP (2018) Prevalence and Associated Factors of Depression in an Asian Community in Dar es Salaam, Tanzania. Psychiatry J 2018:9548471
Mulat N, Gutema H, Wassie GT (2021) Prevalence of depression and associated factors among elderly people in Womberma District, north-west, Ethiopia. BMC Psychiat 21:136
Nerurkar L, Siebert S, McInnes IB, Cavanagh J (2019) Rheumatoid arthritis and depression: an inflammatory perspective. Lancet Psychiat 6:164–173
Nuguru SP, Rachakonda S, Sripathi S, Khan MI, Patel N, Meda RT (2022) Hypothyroidism and Depression: A Narrative Review. Cureus 14:e28201
Parker G, Brotchie H (2010) Gender differences in depression. Int Rev Psychiat (Abingdon, England) 22:429–436
Pelgrims I, Devleesschauwer B, Guyot M, Keune H, Nawrot TS, Remmen R, Saenen ND, Trabelsi S, Thomas I, Aerts R, De Clercq EM (2021) Association between urban environment and mental health in Brussels, Belgium. BMC Public Health 21:635
Polak M, Nowicki GJ, Naylor K, Piekarski R, Ślusarska B (2022) The prevalence of depression symptoms and their socioeconomic and health predictors in a local community with a high deprivation: a cross-sectional studies. Int J Environ Res Public Health 19(18):11797
Poustchi H, Eghtesad S, Kamangar F, Etemadi A, Keshtkar AA, Hekmatdoost A, Mohammadi Z, Mahmoudi Z, Shayanrad A, Roozafzai F, Sheikh M, Jalaeikhoo A, Somi MH, Mansour-Ghanaei F, Najafi F, Bahramali E, Mehrparvar A, Ansari-Moghaddam A, Enayati AA et al (2018) Prospective Epidemiological Research Studies in Iran (the PERSIAN Cohort Study): Rationale, Objectives, and Design. Am J Epidemiol 187:647–655
Probst JC, Laditka SB, Moore CG, Harun N, Powell MP, Baxley EG (2006) Rural-urban differences in depression prevalence: implications for family medicine. Fam Med 38:653–660
Rezayi S, Manouchehri M (2008) Comparison of mental disorders between home owner residents and nurse homes elders. Iranian J Ageing 3:16–25
Romans S, Cohen M, Forte T (2011) Rates of depression and anxiety in urban and rural Canada. Soc Psychiatry Psychiatr Epidemiol 46:567–575
Rondet C, Cornet P, Kaoutar B, Lebas J, Chauvin P (2013) Depression prevalence and primary care among vulnerable patients at a free outpatient clinic in Paris, France, in 2010: results of a cross-sectional survey. BMC Fam Pract 14:1–9
Sarokhani D, Parvareh M, Hasanpour Dehkordi A, Sayehmiri K, Moghimbeigi A (2018) Prevalence of Depression among Iranian Elderly: Systematic Review and Meta-Analysis. Iran J Psychiatry 13:55–64
Sartorius N (2018) Depression and diabetes. Dialogues Clin Neurosci 20:47–52
Sengupta P, Benjamin AI (2015) Prevalence of depression and associated risk factors among the elderly in urban and rural field practice areas of a tertiary care institution in Ludhiana. Indian J Public Health 59:3–8
Shi P, Yang A, Zhao Q, Chen Z, Ren X, Dai Q (2021) A Hypothesis of Gender Differences in Self-Reporting Symptom of Depression: Implications to Solve Under-Diagnosis and Under-Treatment of Depression in Males. Front Psychiat 12:589687
Stansfeld SA, Head J, Fuhrer R, Wardle J, Cattell V (2003) Social inequalities in depressive symptoms and physical functioning in the Whitehall II study: exploring a common cause explanation. J Epidemiol Commun Health 57:361–367
Stubbs B, Vancampfort D, Firth J, Solmi M, Siddiqi N, Smith L, Carvalho AF, Koyanagi A (2018) Association between depression and smoking: A global perspective from 48 low- and middle-income countries. J Psychiatr Res 103:142–149
Summergrad P (2016) Investing in global mental health: the time for action is now. Lancet Psychiatry 3:390–391
Tahan M, Saleem T, Zygoulis P, Pires LVL, Pakdaman M, Taheri H, Ebrahimpour M (2020) A systematic review of prevalence of Depression in Iranian patients. Neuropsychopharmacologia Hungarica : a Magyar Pszichofarmakologiai Egyesulet lapja = Off J Hungarian Assoc Psychopharmacol 22:16–22
Tomita A, Manuel JI (2020) Evidence on the Association Between Cigarette Smoking and Incident Depression From the South African National Income Dynamics Study 2008-2015: Mental Health Implications for a Resource-Limited Setting. Nicotine Tobacco Res: Off J Soc Res Nicotine Tobacco 22:118–123
van den Berg JF, Luijendijk HJ, Tulen JH, Hofman A, Neven AK, Tiemeier H (2009) Sleep in depression and anxiety disorders: a population-based study of elderly persons. J Clin Psychiat 70:1105–1113
Wang J, Wu X, Lai W, Long E, Zhang X, Li W, Zhu Y, Chen C, Zhong X, Liu Z (2017) Prevalence of depression and depressive symptoms among outpatients: a systematic review and meta-analysis. BMJ Open 7:e017173
Weyerer S, Eifflaender-Gorfer S, Köhler L, Jessen F, Maier W, Fuchs A, Pentzek M, Kaduszkiewicz H, Bachmann C, Angermeyer MC, Luppa M, Wiese B, Mösch E, Bickel H (2008) Prevalence and risk factors for depression in non-demented primary care attenders aged 75 years and older. J Affect Disord 111:153–163
World Health, O. (2017) Depression and other common mental disorders: global health estimates. World Health Organization, Geneva
Yaghobi N, Nasr M, Shahmohammadi D (1995) Epidemiological survey of mental disorders in rural areas of Someah Sara, Guilan. Article in Farsi Andeesheh va Raftar J 2:55–65
Yohannes AM (2020) Depression and anxiety in patients with interstitial lung disease. Expert Rev Respiratory Med 14:859–862
Zenebe Y, Akele B, W/Selassie M, Necho M (2021) Prevalence and determinants of depression among old age: a systematic review and meta-analysis. Annals Gen Psychiat 20:55
Zimmerman M, Ellison W, Young D, Chelminski I, Dalrymple K (2015) How many different ways do patients meet the diagnostic criteria for major depressive disorder? Comprehensive Psychiat 56:29–34
Acknowledgments
The authors wish to thank all staff of the PERSIAN Guilan cohort study (PGCS) for their kind help in data collection.
Author information
Authors and Affiliations
Contributions
Adeleh Isanazar, Farahnaz Joukar, and Robabeh Soleimani contributed substantially to the conception or design of the work and approved the version to be published.
Saman Maroufizadeh contributed substantially to the analysis or interpretation of data.
Niloofar Faraji and Tahereh Zeinali drafted the work and revised it critically for important intellectual content.
Mohammadreza Naghipour and Fariborz Mansour-Ghanaei agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Consent to participate
Written consent was obtained from each participant after they were informed of the purpose and importance of the study. To ensure confidentiality of participants' information, codes were used whereby the name of the participant and any personally identifiable information was not written on the questionnaire.
Consent for publication
All participants gave their consent to publication.
Ethics approval
This study was approved by the ethics committees at the Guilan University of Medical Sciences [IR.GUMS.REC.1398.183]. Informed consent was obtained from all individual participants.
Conflicts of interest
The authors declare that they have no competing interests in this work.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Isanazar, A., Joukar, F., Maroufizadeh, S. et al. Prevalence of depression and associated factors among adults: The PERSIAN Guilan cohort study (PGCS). J Public Health (Berl.) (2023). https://doi.org/10.1007/s10389-023-01898-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10389-023-01898-1