Abstract
Aim
Identifying risk factors associated with mortality in elderly patients hospitalized with COVID-19 can be helpful in managing the disease in this age group. Therefore, the aim of this study was to determine the risk factors of death in elderly patients hospitalized with COVID-19 in Hamadan in 2020.
Subject and methods
This cross-sectional study was performed on the medical records of 1694 patients aged 60 years and older who were diagnosed with COVID-19 disease between March and August 2020 and were admitted to Shahid Beheshti and Sina Hospitals. A researcher-made checklist included demographic information, clinical information, laboratory results, type of procedures performed for the patient in the hospital, and the number of hospitalization days.
Results
The results showed that 30% of the elderly patients died due to COVID-19 complications. The results of adapted logistic regression showed that the variables of gender, age, inpatient ward and laboratory indices of albumin, hemoglobin, ESR, and LDH were the main predictors of COVID-19 related death in elderly patients (p < 0.05).
Conclusion
The rate of COVID-19 related death in the hospitalized elderly patients is remarkable. The death rate increased among male patients, age older than 75 years, hospitalization in the ICU, increased ESR and HDR levels, and decreased albumin and hemoglobin.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although most patients with COVID-19 are thought to have a favorable prognosis, elderly patients and those with chronic diseases may have worse outcomes (Cucinotta and Vanelli 2020; Wu et al. 2020). Older patients with COVID-19 show relatively higher mortality and disease severity than younger patients (Ruan et al. 2020; Wang et al. 2020). In other words, the elderly represent a special group of patients at high risk for contracting COVID-19 with rapidly progressive clinical deterioration, and their lives are in serious danger (Perrotta et al. 2020).
Compared to patients with a single disease, the hospitalization rate and mortality rate of patients with co-morbidities are higher, and the clinical prognosis is significantly poor (Dai et al. 2021; Nikpouraghdam et al. 2020; Noor and Islam 2020). This is despite the fact that the co-morbidity of chronic diseases in the elderly is a common problem in the field of global public health (Coventry et al. 2015). It has been reported that more than half of the elderly in developed countries have more than three chronic diseases, which means that a person suffers from two or more diseases with different pathologies (American Geriatrics Society Expert Panel on the Care of Older Adults with Multimorbidity 2012).
Elderly patients due to many reasons, including weak immune system, underlying chronic diseases of multi-drug regimen, lack of attention, and lack of ability to fully and correctly observe the principles of personal hygiene and self-care, inappropriate hygiene of the living environment, loneliness and being single, and lack of sufficient support from other family members and late visit to the doctor, are among the most vulnerable sections of the society in the face of the coronavirus epidemic (Cervellati et al. 2020; Jannat 2020; Rastad et al. 2020; Zuin et al. 2021). Patients with COVID-19 primarily have fever, dry cough, fatigue, or myalgia (Huang et al. 2020). However, the clinical characteristics of elderly patients with COVID-19 include fever, sputum and cough, and the ratio of multiple lobe involvement and pneumonia severity index score are significantly higher in elderly patients compared to middle-aged and young people (Liu et al. 2020). Considering the noticeable growth rate of the elderly population in Iran (3.9%) and 9.2% of the Iranian population are in the elderly age, as well as the high prevalence of underlying diseases in the elderly, more attention should be paid to this age group (Farokhnezhad Afshar 2020).
Nearly 9% of the worldwide population are aged 65 and over. Projections estimated that this proportion will increase to nearly 17% of the world’s population by 2050 (National Institute on Aging 2016). According to the statistics of the Welfare Department, 9.8% of the population of Hamedan province is elderly, and in this respect, it ranks fourth among the provinces of the country. Due to some complexities in treatment of these patients such as non-adherence of medication, adverse effects of medication, need for a medication review, and complex medication regimen due to suffering from chronic diseases, conducting specific research in these patients is unavoidable. Identifying the risk factors related to COVID-19 related deaths in elderly patients can be helpful in the management of the disease in this age group and help the physicians to identify patients with a poor prognosis in the early stages. Therefore, the present study was conducted with the aim of determining the risk factors associated with death in elderly patients with COVID-19 in Hamadan City in the year 2020.
Materials and methods
In this cross-sectional study, all elderly patients (60 years old and older) with a definite diagnosis of COVID-19 who were admitted to Shahid Beheshti Hospital and Sina Hospital (Farshchian) of Hamadan University of Medical Sciences from March 2020 to the end of 2021 were included in the study. Inclusion criteria were old patients with the definitive diagnosis of COVID-19 based on the result of PCR test and complete medical records. Patients whose treatment outcome was unclear were excluded from the study. In order to collect information, a researcher-made checklist was used, and all information was extracted from the patient’s files. The checklist includes demographic information (age, gender, place of residence, marital status, education, and occupation) and clinical information (underlying disease, disease symptoms, SPO2, and vital signs), radiological symptoms (CT scan result, radiology result), laboratory results (creatinine level, ferritin, white blood cells, etc.), smoking history, drug use, the type of procedures performed for the patient in the hospital, and the number of days of hospitalization.
The independent t-test was used to compare the treatment result (recovery or death) for quantitative variables, and the chi-square test was used to compare qualitative variables. In order to simultaneously predict and examine factors affecting death in patients, crude and adjusted logistic regression models were used. Data analysis was done using Stata software version 14 and the statistical significance level was considered less than 5%.
Results
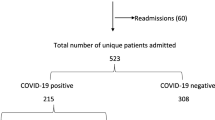
In the present study, a total of 1694 patients with COVID-19, whose age was 60 years and older, were examined. Among them, 1180 patients recovered (69.7%) and 514 patients died (30.3%). The demographic characteristics of the patients are presented in Table 1. As shown, the results of the chi-square test showed that the outcome of the disease had a statistically significant relationship with the gender (p = 0.009) and age group (p < 0.001) of the patients. Moreover, the outcome of the disease is significantly related to heart disease (p = 0.002) and nervous system morbidity (p = 0.001).
As Table 2 shows, the outcome of the disease (recovery or death) was significantly different based on the mean of systolic and diastolic blood pressure, SPO2, ESR, BUN, BS, PT, Albumin, CPK, SGPT, Alp, hemoglobin, Troponin, LDH, and Lym (p < 0.05).
Demographic predictors of death in the hospitalized COVID-19 positive elderly are presented in Table 3. According to Table 4, the results of the crude logistic regression test showed that the odds of death in elderly males was 1.31 times higher than in women (p = 0.009) and in the age group over 75 years old was 2.43 times higher than in the age group 75–60 years old (p < 0.001).
The results of the logistic regression test showed that the clinical and biochemical variables of systolic and diastolic blood pressure, albumin, hemoglobin, troponin, SPO2, ESR, BUN, BS, PT, Cpk, SGPT, Alp, LDH, and Lym were significantly associated with death in elderly COVID-19 positive patients (p < 0.05) (Table 4).
Based on Table 5, the results of the adjusted logistic regression showed that the variables of gender, age, hospital ward and the laboratory indicators of albumin, hemoglobin, ESR and LDH in the presence of other variables in the model, were as the main predictors of death in the COVID-19 positive elderly patients (p < 0.05).
Discussion
The results of the present study showed that the gender, age, hospitalization ward of the patient, and the laboratory indicators of albumin, hemoglobin, ESR, and LDH in the presence of all other investigated variables were the main predictors of COVID-19 related death in elderly patients.
In line with the results of the present study, the results of the study by Team et al. in the epidemiology team of the emergency response to the new coronavirus pneumonia showed that the death rate in the age group of 70–79 years was 8% and in the age group above 80 years was 14%, while it was less than 1% in age groups under 50 (Team 2020).
In this regard, Papadopoulos et al. and Guan et al. reported a higher rate of death in elderly male patients (Guan et al. 2020; Papadopoulos et al. 2021). Also, Leung et al. concluded that age is a major risk factor for mortality among elderly patients of different ages (Leung 2020).
In line with the results of the present study, in Zali et al.’s study, the highest mortality rate was reported in patients over 65 years of age and patients with diabetes, cardiovascular diseases, and cancer patients (Zali et al. 2020). In the present study, older age was identified as an independent risk factor for death, and heart disease had a significant effect on the rate of death in the elderly, although this relationship was not significant in the adjusted model. In Zali et al.’s study, contrary to the results of the present study, diabetes and cancer was reported to be among the risk factors for mortality. This difference could be due to the difference in the samples. In our study, we only investigated elderly patients and only 2.5% of the elderly were diagnosed with cancer, and therefore these results cannot be generalized to the entire population. Contrary to the results of Mendes et al.’s study, which reported lung crackle as an independent risk factor for death in patients with COVID-19, we could not observe a significant relationship in this connection (Mendes et al. 2020). Moreover, unlike the study of Sousa et al. that stated chronic obstructive pulmonary disease and cardiovascular diseases were associated with a significant increase in the risk of death in these patients (Sousa et al. 2020), in the present study, in the adjusted model, the aforementioned variables did not have a significant relationship with an increase in the risk of death in these patients.
Based on the results of the present study, albumin was among the independent risk factors for increasing the odds of death in the COVID-19 positive elderly patients. In line with the results of the present study, Violi et al. concluded that low human serum albumin and old age were independently associated with an increase in mortality rate in patients with COVID-19 (Violi et al. 2021). Also, in a review study by Acharya et al. in line with the results of the present study, low serum albumin during the onset of COVID-19 infection was associated with serious consequences such as kidney damage, cardiac damage, hypercoagulability, post-viral physical disability, and encephalopathy (Acharya et al. 2021). The results of the study by Li et al. in confirmation of the results of the present study showed that the increase in the severity of COVID-19 pneumonia had a positive relationship with the lower levels of platelets and albumin, and therefore the level of albumin can be used as an independent predictor of the risk of death in critically ill COVID-19 positive patients (Li et al. 2020).
Albumin is an important defense factor in the body that protects host cells against oxidative burst that occurs against infection or inflammation (Caraceni et al. 2013; Galley 2011; Rabbani and Ahn 2019). The plasma albumin level during acute inflammation decreases rapidly due to transcapillary leakage, and other mechanisms (Artigas et al. 2016; Caraceni et al. 2013), and in such conditions, the low level of serum albumin can make the body more vulnerable and in this field, there is a need to conduct interventional studies to reach a definite result.
The results of the present study showed that one of the independent predictors of death in the elderly with COVID-19 is ESR level. In line with the results of the present study, Alwafi et al. reported that one of the independent risk factors for increased mortality in patients with COVID-19 was an ESR level of 10 mm/h (Alwafi et al. 2021). In line with the results of the present study, in a study conducted by Tian et al., the level of red blood cell sedimentation (ESR) in people who died was higher than in those who recovered from the disease of COVID-19 (Tian et al. 2020). In the present study, the average ESR in patients who died was higher than in patients who recovered.
The results of the present study showed that a higher LDH level is an independent risk factor for increased mortality in the elderly with COVID-19. In line with the results of the present study, in the study of Li et al., the results showed that male gender, older age, and high LDH level are associated with increased death in patients with severe COVID-19, and therefore patients with older age and high LDH level need careful observation and early intervention is essential to prevent the potential progression of severe COVID-19 (Li et al. 2020). In this regard, Tian et al. reported that LDH levels were higher in deceased people compared to those who recovered from COVID-19 (Tian et al. 2020).
In the present study, the results showed that the decrease in hemoglobin level as an independent factor was associated with the increased risk of mortality in the elderly with COVID-19. In line with the results of the present study, Oh et al. reported that anemia during hospitalization was independently associated with an increased probability of death from all causes in hospitalized patients with COVID-19 (Oh et al. 2021).
Hemoglobin concentration is one of the most important indicators of oxygen-carrying capacity in the blood. In conditions of compromised breathing and an increased need for oxygen in a hypermetabolic state such as COVID-19, anemia can further reduce oxygen delivery to surrounding tissues (Chu et al. 2020).
The retrospective nature of the study and the nonexistence of the disease severity in the patient’s medical records can be considered as the limitations of the study.
Conclusion
The results showed that the rate of deaths in the elderly with COVID-19 is high. The death rate among males, age older than 75 years, hospitalization in the ICU, increased ESR and HDR levels, and decreased albumin and hemoglobin levels is significantly higher. Therefore, it is recommended to all health care workers, especially in older patients, to take seriously the presence of any of these risk factors and take early intervention to prevent the severe progression of the disease.
Abbreviations
- Systolic BP:
-
systolic blood pressure
- ECG :
-
electrocardiogram
- CRP :
-
c-reactive protein
- ESR :
-
erythrocyte sedimentation rate
- BUN :
-
blood urea nitrogen
- Cr :
-
creatinine
- PT :
-
prothrombin time
- PTT :
-
partial thromboplastin time
- WBC :
-
white blood cells
- HCT :
-
hematocrit
- Hb :
-
hemoglobin
- LDH :
-
lactate dehydrogenase
- CPK :
-
creatine phosphokinase
- SGOT :
-
serum glutamic-oxaloacetic transaminase
- SGPT :
-
serum glutamic-pyruvic transaminase
- Alp :
-
alkaline phosphatase
- BS :
-
blood sugar
- SPO2 :
-
peripheral oxygen saturation with pulse oximeter
- K :
-
potassium
- Na :
-
Sodium
References
Acharya R, Poudel D, Bowers R et al (2021) Low serum albumin predicts severe outcomes in COVID-19 infection: a single-center retrospective case-control study. J Clin Med Res 13(5):258. https://doi.org/10.14740/jocmr4507
Alwafi H, Naser AY, Qanash S et al (2021) Predictors of length of hospital stay, mortality, and outcomes among hospitalised COVID-19 patients in Saudi Arabia: a cross-sectional study. J Multidiscip Healthc 14:839. https://doi.org/10.2147/JMDH.S304788
American Geriatrics Society Expert Panel on the Care of Older Adults with Multimorbidity (2012) Guiding principles for the care of older adults with multimorbidity: an approach for clinicians. J Am Geriatr Soc 60(10):E1–E25. https://doi.org/10.1111/j.1532-5415.2012.04188.x
Artigas A, Wernerman J, Arroyo V et al (2016) Role of albumin in diseases associated with severe systemic inflammation: pathophysiologic and clinical evidence in sepsis and in decompensated cirrhosis. J Crit Care 33:62–70. https://doi.org/10.1016/j.jcrc.2015.12.019
Caraceni P, Tufoni M, Bonavita M-E (2013) Clinical use of albumin. Blood Transfus 11(Suppl 4):s18. https://doi.org/10.2450/2013.005s
Cervellati C, Trentini A, Pecorelli A et al (2020) Inflammation in neurological disorders: the thin boundary between brain and periphery. Antioxid Redox Signal 33(3):191–210. https://doi.org/10.1089/ars.2020.8076
Chu H, Chan JF-W, Yuen T-T et al (2020) Comparative tropism, replication kinetics, and cell damage profiling of SARS-CoV-2 and SARS-CoV with implications for clinical manifestations, transmissibility, and laboratory studies of COVID-19: an observational study. Lancet Microbe 1(1):e14–e23. https://doi.org/10.1016/S2666-5247(20)30004-5
Coventry P, Lovell K, Dickens C et al (2015) Integrated primary care for patients with mental and physical multimorbidity: cluster randomised controlled trial of collaborative care for patients with depression comorbid with diabetes or cardiovascular disease. BMJ 350. https://doi.org/10.1136/bmj.h638
Cucinotta D, Vanelli M (2020) WHO declares COVID-19 a pandemic. Acta Bio Medica: Atenei Parmensis 91(1):157. https://doi.org/10.23750/abm.v91i1.9397
Dai S-P, Zhao X, Wu J-h (2021) Effects of comorbidities on the elderly patients with COVID-19: clinical characteristics of elderly patients infected with COVID-19 from Sichuan, China. J Nutr Health Aging 25(1):18–24. https://doi.org/10.1007/s12603-020-1486-1
Farokhnezhad Afshar P (2020) COVID-19 pandemic in the community-dwelling and nursing home older adults in Iran. J Gerontol 5(3):26–28
Galley H-F (2011) Oxidative stress and mitochondrial dysfunction in sepsis. Br J Anaesth 107(1):57–64. https://doi.org/10.1093/bja/aer093
Guan W-J, Ni Z, Hu Y et al (2020) Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 382(18):1708–1720. https://doi.org/10.1056/NEJMoa2002032
Huang C, Wang Y, Li X et al (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395(10223):497–506. https://doi.org/10.1016/S0140-6736(20)30183-5
Jannat Z (2020) COVID-19 and the elderly with chronic diseases: narrative review. J Military Med 22(6):632–640
Leung C (2020) Risk factors for predicting mortality in elderly patients with COVID-19: a review of clinical data in China. Mech Ageing Dev 188:111255. https://doi.org/10.1016/j.mad.2020.111255
Li J, Li M, Zheng S et al (2020) Plasma albumin levels predict risk for nonsurvivors in critically ill patients with COVID-19. Biomark Med 14(10):827–837. https://doi.org/10.2217/bmm-2020-0254
Liu K, Chen Y, Lin R et al (2020) Clinical features of COVID-19 in elderly patients: a comparison with young and middle-aged patients. J Inf Secur 80(6):e14–e18. https://doi.org/10.1016/j.jinf.2020.03.005
Mendes A, Serratrice C, Herrmann F-R et al (2020) Predictors of in-hospital mortality in older patients with COVID-19: the COVIDAge study. J Am Med Dir Assoc 21(11):1546–1554. https://doi.org/10.1016/j.jamda.2020.09.014
National Institute on Aging (2016) World’s older population grows dramatically. Available at: https://www.nih.gov/news-events/news-releases/worlds-older-population-grows-dramatically. Accessed Mar 2022
Nikpouraghdam M, Farahani A-J, Alishiri G et al (2020) Epidemiological characteristics of coronavirus disease 2019 (COVID-19) patients in IRAN: a single center study. J Clin Virol 127:104378. https://doi.org/10.1016/j.jcv.2020.104378
Noor F-M, Islam M (2020) Prevalence and associated risk factors of mortality among COVID-19 patients: a meta-analysis. J Community Health 45(6):1270–1282. https://doi.org/10.1007/s10900-020-00920-x
Oh S-M, Skendelas J-P, Macdonald E et al (2021) On-admission anemia predicts mortality in COVID-19 patients: a single center, retrospective cohort study. Am J Emerg Med 48:140–147. https://doi.org/10.1016/j.ajem.2021.03.083
Papadopoulos V, Li L, Samplaski M (2021) Why does COVID-19 kill more elderly men than women? Is there a role for testosterone? Andrology 9(1):65–72. https://doi.org/10.1111/andr.12868
Perrotta F, Corbi G, Mazzeo G et al (2020) COVID-19 and the elderly: insights into pathogenesis and clinical decision-making. Aging Clin Exp Res 32(8):1599–1608. https://doi.org/10.1007/s40520-020-01631-y
Rabbani G, Ahn S-N (2019) Structure, enzymatic activities, glycation and therapeutic potential of human serum albumin: a natural cargo. Int J Biol Macromol 123:979–990. https://doi.org/10.1016/j.ijbiomac.2018.11.053
Rastad H, Karim H, Ejtahed M et al (2020) Risk and predictors of in-hospital mortality from COVID-19 in patients with diabetes and cardiovascular disease. Diabetol Metab Syndr 12(1):1–11. https://doi.org/10.1186/s13098-020-00565-9
Ruan Q, Yang K, Wang W et al (2020) Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med 46(5):846–848. https://doi.org/10.1007/s00134-020-05991-x
Sousa G, Garces T, Cestari V et al (2020) Mortality and survival of COVID-19. Epidemiol Infect 148. https://doi.org/10.1017/S0950268820001405
Team E (2020) The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19)—China, 2020. China CDC weekly 2(8):113
Tian W, Jiang W, Yao J et al (2020) Predictors of mortality in hospitalized COVID-19 patients: a systematic review and meta-analysis. J Med Virol 92(10):1875–1883. https://doi.org/10.1002/jmv.26050
Violi F, Cangemi R, Romiti G-F, et al (2021) Is albumin predictor of mortality in COVID-19? Antioxid Redox Signal 35(2):139–142. https://doi.org/10.1089/ars.2020.8142
Wang D, Hu B, Hu C et al (2020) Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA 323(11):1061–1069. https://doi.org/10.1001/jama.2020.1585
Wu C, Chen X, Cai Y et al (2020) Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med 180(7):934–943. https://doi.org/10.1001/jamainternmed.2020.0994
Zali A, Gholamzadeh S, Mohammadi G et al (2020) Baseline characteristics and associated factors of mortality in COVID-19 patients; an analysis of 16000 cases in Tehran, Iran. Arch Acad Emerg Med 8(1):e70.
Zuin M, Guasti P, Roncon L, et al (2021) Dementia and the risk of death in elderly patients with COVID-19 infection: Systematic review and meta-analysis. Int J Geriatric Psych. https://doi.org/10.1002/gps.5468
Acknowledgments
The authors would like to express their gratitude to the Vice-Chancellor of the Research and Technology from Hamadan University of Medical Sciences who financially supported the project (project number: 140002281404 and ethics code: IR.UMSHA.REC.1400.165).
Funding
Vice-Chancellor of the Research and Technology from Hamadan University of Medical Sciences financially supported the project (project number: 140002281404).
Author information
Authors and Affiliations
Contributions
SK, SS, and SB participated in the design of the manuscript, SK, performed the analyses, all authors, participated in the writing and critically reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The ethical approval of the study was obtained from Ethics Committee of Hamadan University of Medical Sciences (ethics code: IR.UMSHA.REC.1400.165).
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sharifi, S., Bashirian, S., Soltanian, A. et al. Predictors of COVID-19 related death in elderly patients hospitalized due to COVID-19 infection: a cross-sectional study in the west of Iran. J Public Health (Berl.) 32, 813–818 (2024). https://doi.org/10.1007/s10389-023-01868-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10389-023-01868-7