Abstract
Aim
To investigate the relationship between neighbourhood school environment and dental care needs of 5-to-11-year-olds attending a local dental facility in Portsmouth, South-East England.
Methods
Secondary analyses were undertaken using three cross-sectional, open-access datasets. Data included 4 years of children’s electronic dental records from the University of Portsmouth Dental Academy comprising age, gender, tooth extraction history and residential postcodes converted to Index of Multiple Deprivation (IMD) quintiles for census-based geographies called middle-layer super output areas (MSOAs). Additionally, overall effectiveness scores (OES) (1=Outstanding to 4=Inadequate) from Office for Standards in Education, Children’s Services and Skills of neighbouring schools were computed to ‘population-weighted mean OES’. Descriptive, univariate logistic regression and multilevel-modelling analyses investigated contextual-level influence of school-OES on tooth extraction.
Results
There were 429-patients [mean-age 7.78 years (SD 1.97 years), female 50.1%] living across 23-MSOAs. Seventy had undergone tooth extraction treatment. Population-weighted mean OES range was 1.74–3.00, while 3.5% and 48% of patients belonged to the most and least deprived IMD-quintiles, respectively. Univariate models revealed age and population-weighted mean OES as statistically significant predictors of tooth extraction (p < 0.05). Multilevel modelling, controlling for age and population-weighted mean OES indicated likelihood of tooth extraction increased by 15% with increasing age and by 161% for patients living in MSOAs with higher population-weighted mean OES (i.e. poor school-performance).
Conclusions
School effectiveness scores remained a significant predictor of tooth extraction in our study when controlling for individual predictors of dental health. Further research is required to assess the role of neighbourhood school environment in predicting child dental health at the national level.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the period 2019–2020, tooth extractions accounted for 14.3% of all clinical treatments provided to children within the primary dental care sector of the National Health Service (NHS) in England (NHS Digital 2020). Tooth extraction is an undesired treatment option for dental caries. Generally, preventive and restorative measures are preferred to maintain a natural dentition for as long as possible (Public Health England et al. 2021). Often, children who have extensive untreated tooth decay will require speciality care for extraction of single or multiple teeth under general anaesthesia (GA) or sedation within hospital services (National Health Service 2020). This is challenging for parents and children and costly to the NHS. In 2019–2020, a total of 55,137 completed consultant episodes were recorded for tooth extractions in children and adolescents aged 0 to 19 years in NHS secondary care hospitals in England (Public Health England 2020a). Approximately 64% of these extractions were related to untreated dental caries (Public Health England 2020a). Untreated dental caries is also associated with geographical inequalities. Despite the free dental care provision within the NHS (2021), the highest rates for tooth extractions have been consistently observed amongst children living in the most disadvantaged regions and localities within England (NHS Digital 2020; Public Health England 2020a).
Children living in deprived neighbourhoods are four times more likely to undergo tooth extractions as compared to those living in affluent communities (Public Health England 2020a, 2021). These patterns mirror the dental caries prevalence through routine national surveys and also with the patterns observed in the uptake of care (Wanyonyi et al. 2016; Wanyonyi et al. 2013; Public Health England 2018a, b, 2019, 2020b). Although, there is considerable evidence that verifies the link between where an individual lives and their dental health (Jamieson et al. 2013; Wanyonyi et al. 2016; Wanyonyi et al. 2017), exact mediators of this relationship remain underexplored. Authors suggest that the unequal distribution of mediating socio-environmental factors, including neighbourhood deprivation, level of urbanisation and distance from dental services, could explain these patterns (Pattussi et al. 2006; Cabral et al. 2015; Nobrega et al. 2017; Peres et al. 2019).
Schools are one of the social environments of interest and have been an important setting for promoting various oral health interventions such as the prevention of excessive sugar consumption, supervised tooth brushing with fluoridated toothpaste and routine dental check-ups (Public Health England et al. 2021). Children spend a large amount of time in schools, where they use facilities such as school canteens and snack centres accessing sugary foods, a risk factor for tooth decay (Sheiham and Watt 2000; Moynihan and Kelly 2014). To a lesser or greater extent, they are supervised by teachers and staff which may have an influence on their sugar consumption (World Health Organisation 2015; Moynihan 2016). This influence can be a result of various school-related factors such as quality of education, teachers’ support and involvement in pupils’ development, pupils’ academic attainment, school-based health policies and school governance.
A few studies have linked some aspects of the school environment to dental health. da Franca et al. (2020) suggested that a favourable school academic climate, as defined by higher educational aspirations of students, is linked to tooth loss prevalence amongst adolescents. These results are in line with other research suggesting a causal link between the duration of school education and tooth loss in later life (Matsuyama et al. 2019). Moysés et al. (2003) proposed that the comprehensiveness of the school curriculum and school support are associated with the percentage of caries-free children. Whilst food policies and interventions are endorsed by the school leadership and management, support offered by teachers have shown to shape children’s dietary behaviour, and therefore significantly influence their dental health (Maliderou et al. 2006; Freeman and Oliver 2009; Carvalho et al. 2014; Thornley et al. 2017; Marshman et al. 2019; Samuel et al. 2020). Although the individual impacts of various school-level determinants on child dental health have been explored previously, the collective influence of all these determinants on advanced treatment needs such as tooth extractions remains unexamined.
This study explores the hypothesis that the school environment extends to the geographical environment and contributes to the disparity in dental needs in small geographies, in this case, as demonstrated by the need for advanced dental treatment in the local dental facility. This assertion is supported by the understanding that in England, children live and attend schools within a 3-mile radius (Department for Education 2014). Therefore, it is highly likely that children living in deprived communities attend schools in deprived areas. Studies have shown that school location is important in relation to child dental health. Rajab et al. (2014), revealed that the children attending schools in disadvantaged areas of Jordan had higher dental caries prevalence than those going to schools in affluent areas. Edasseri et al. (2017) recorded a similar association in Quebec. With this in mind, the overall aim of this study was to investigate the relationship between school environment within neighbourhoods in a Local Authority (LA) in South-East England and the dental care needs of 5 to 11-year-old children attending a primary dental care facility in the area.
Methods
This research involved secondary analyses of cross-sectional and open-access data (Thyer 2009).
Study population
Children aged 5 to 11 years living across small areas within Portsmouth LA, England were considered as a study population for this research. In England, geographical dental health inequalities are most common amongst this age group (Public Health England 2018a, b, 2020b). Children of this age group are most likely to attend primary schools in England.
Data collection
Three datasets were acquired from published and open-access resources.
The first dataset was acquired from an open-access publication (Wanyonyi et al. 2017) and comprised the electronic dental records (2008-2012) of children attending the University of Portsmouth Dental Academy (UPDA), an NHS primary dental care service and training centre, located within Portsmouth LA in South-East England. Details of the data collection, cleaning and validation can be found in previous publications (Wanyonyi et al. 2017, 2019). The data included completed or closed courses of both emergency and planned care provided over four years (Wanyonyi et al. 2017). They included information on paediatric patients’ age, gender and treatment records, including any provision of tooth extraction treatment.
The second dataset was the latest full inspection reports of state-funded primary schools in England (28 September 2006 – 31 October 2020), generated by the Office for Standards in Education, Children’s Services and Skills (Ofsted) (Office for Standards in Education 2020). Ofsted is a non-ministerial and independent department that serves a responsibility to inspect all educational organisations and training services, including state funded-primary schools within England, as per the education inspection framework under section 5 and section 8 of the Education Act 2005 (The Stationary Office Limited 2005; The Office for Standards in Education 2019). The Department of Education (DfE) and schools are legally obliged to provide relevant information such as school records and individual pupils’ data to Ofsted. Whilst section 8 inspections are carried out only under special circumstances, Ofsted is required to conduct full-scale section 5 inspections within an interval of five school years. This allows for comprehensive and regular monitoring of schools.
Ofsted publishes evaluation data and reports the ‘Overall Effectiveness Score (OES)’ of each inspected school on a monthly basis (The Office for Standards in Education 2019). The OES has four categories, including a score of 1 to 4 with 1 outstanding and 4 inadequate (The Office for Standards in Education 2019). This score is evaluated by highly trained inspectors based on four key aspects: 1.‘quality of education’ encompassing factors such as curriculum design, delivery, and its impact on pupil attainment, 2.‘behaviour and attitudes’ incorporating assessment of the general behaviour and attendance of pupils in schools, 3.‘personal development’ comprising indicators associated with the overall health and wellbeing of pupils, and 4.‘leadership and management’ including school vision, ethos, governance, and staff development. Each aspect is judged according to pre-defined criteria for maintaining the reliability of inspection procedures (The Office for Standards in Education 2019).
In this study, school OES has been used as a comprehensive measure of school performance. This score is based on a robust theoretical framework and is evaluated by the trained inspectors, using multiple off-site and on-site evaluation methods (The Office for Standards in Education 2019). It has previously been used to study health behaviours such as the uptake of vaccines (Fletcher et al. 2019). Being commonly used in the government’s education sector for monitoring purposes (Department for Education 2019a; b), and to ensure parents’ reliability in selecting children’s schools (The UK Government 2021), data on OES are regularly published and updated (Office for Standards in Education 2020), making it a reliable source of information and a useful indicator to assess overall school performance.
The third dataset contained information on area-level deprivation across small areas in England based on the national Indices of Multiple Deprivation (IMD) 2019 (Ministry of Housing Communities and Local Government 2019b, c). The IMD is a relative measure of deprivation, providing cumulative deprivation scores for small areas known as Lower-layer Super Output Areas (LSOAs), census-based geographies with 400–1200 households, located within England (Office for National Statistics 2019). This measure has been widely used in the public health field to account for contextual deprivation (Wanyonyi et al. 2016; Wanyonyi et al. 2017; Public Health England 2018a, 2020a, 2021).
Data processing
For the purposes of this research, the Middle-layer Super Output Areas (MSOAs) were used to describe small area geographies for data analyses. The MSOAs are census-based statistical areas (Office for National Statistics 2019). Their population can range between 5000 and 15000 people. At present, there are 6791 MSOAs in England with a mean population of 7200 people. Similar to the LSOAs, each MSOA has a unique code and a name.
All data were processed using Statistical Package for the Social Sciences (SPSS) version 26 (IBM_Corporation 2019). First, the UPDA dataset was processed, and electronic dental records of patients aged between 5 and 11 years were extracted. Patients’ residential LSOA codes, available within the data, were matched with the Census 2011 MSOA codes using GeoConvert, a tool facilitating matching and transforming of census-based geographies (2015). MSOAs within Portsmouth LA were selected for further analysis using a lookup table for the census 2011 (UK Data Service 2018).
Second, the Ofsted dataset was processed, and data on the state-funded primary schools of all types, including community, voluntary (aided and controlled), academy (converter and sponsor led), foundation and free schools, located within Portsmouth LA, were extracted out. School postcodes were initially matched with LSOAs using the Indices of Multiple Deprivation (IMD) Postcode Lookup 2015 application (Ministry of Housing Communities and Local Government 2015) and then with MSOAs using GeoConvert (UK Data Service 2015). The data contained full inspection reports of 46 schools in total.
A new variable called ‘population-weighted mean overall effectiveness score (OES)’ of schools within each MSOA was derived to quantify the neighbourhood school environment. Weighting was carried out to accommodate the different number of schools per MSOA and the different number of pupils per school (Buckley and King-Hele 2014).
The following formula was used to configure this variable:
Population-weighted mean overall effectiveness score of schools within MSOA = ∑ (Overall effectiveness score of each school in MSOA* Total number of pupils in each school in MSOA) / Total number of pupils per MSOA.
This variable was then linked to the UPDA patients’ records via MSOA codes.
Third, the MSOA-level population-weighted mean IMD scores were derived, where LSOA-level IMD scores were aggregated using denominators provided in the IMD data (Ministry of Housing Communities and Local Government 2019a, c). These scores were then ranked and categorized into quintiles, where quintiles 1 and 5 represented the highest and the lowest level of deprivation, respectively (Ministry of Housing Communities and Local Government 2019a). These IMD quintiles were linked to the UPDA paediatric patients’ records using MSOA codes.
Data analyses
Initially, data were descriptively analysed to outline the sociodemographic characteristics of the study sample and other variables of interest (Hanneman et al. 2012). Bar charts were plotted to assess the distribution of patients’ age and gender, population-weighted mean OES of schools in MSOA, IMD quintiles, number of patients living across MSOAs, and number of patients who have undergone tooth extraction treatment. Then, univariate logistic regression analyses were carried out to determine the influence of each predictor variable, i.e. age, gender, population-weighted mean OES, and IMD quintile on the outcome variable, i.e. tooth extraction (Menard 2002; Lewis-Beck et al. 2011; Hanneman et al. 2012). Both descriptive and logistic regression analyses were carried out using the SPSS version 26 (IBM_Corporation 2019).
Lastly, multilevel modelling analysis was conducted to determine the contextual level significance of population-weighted mean OES in predicting tooth extractions in paediatric patients while adjusting for other predictor variables. This was undertaken using the MLwiN software package (version 3.05) (Centre of Multilevel Modelling 2020). As the sample size was small, all models were initially estimated using iterative generalised least squares (IGLS) and then by Markov chain Monte Carlo (MCMC) techniques (Browne et al. 2017). Up to 150,000 iterations were completed to ensure the stability of the final model, achieved when the Raftery–Lewis diagnostic condition was satisfied (Spiegelhalter et al. 2002).
Results
Study participants
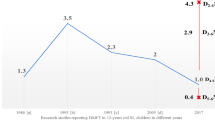
A total of 429 patients aged 5 to 11 years were included in the analyses. Table 1 provides details on sociodemographic characteristics relating to the study participants and other variables of interest. The mean age was 7.78 years (SD= 1.97 years). Most patients were 6-year-olds (17.50%). Around half of all child patients were females (50.10%). A total of 70 patients had undergone tooth extractions during the 4 years (16.30%). The patients lived across 23 out of the 25 MSOAs within Portsmouth LA. There were between 6 and 47 patients across the MSOAs (Fig. 1). The population-weighted mean OES of schools within each MSOA ranged from 1.74 to 3.00. Most patients (70.60%) were living in MSOAs with a population-weighted mean OES of 2.00. The number of patients belonging to the least deprived IMD quintiles was much higher (48%) than those belonging to the most deprived IMD quintiles (3.5%).
Univariate logistic regression results
The univariate logistic regression results are presented in Table 2. Models 1 and 3 showed that age and population-weighted mean OES were significantly associated (p < 0.05), with tooth extraction, respectively. Model 1 revealed that the risk of tooth extraction rose by 16% with each year of increase in age [(p = 0.02), odds ratio 1.16 (CI = 1.02, 1.32)]. Model 3 demonstrated that the chances of undergoing tooth extraction soared by 166% for patients living in MSOAs with higher population-weighted mean OES [(p = 0.03), odds ratio 2.66 (CI = 1.06, 6.64)]. Higher population-weighted mean OES meant the MSOA had a comparatively greater proportion of children attending poor performing schools. Models 2 and 4 indicated no significant difference in the possibility of undergoing tooth extraction by gender and IMD quintiles, respectively.
Multilevel modelling results
The final multilevel models are presented in Table 3. In model 1, all predictor variables were included. This model indicated that population-weighted mean OES was a significant predictor of tooth extraction at the MSOA level (p < 0.05), even though all predictor variables, i.e. age, gender and IMD quintiles were adjusted. In model 2, only age and population-weighted mean OES variables were included. Both variables remained significantly associated with tooth extraction (p < 0.05). Deviance informative criterion (DIC) was reduced by 3.39, suggesting model 2 was better than the previous model. The odds ratio for age remained nearly the same as compared to the one obtained through univariate logistic regression (Table 2). This model revealed that the probability of tooth extraction raised by 15% with increasing age and by 161% with increasing population-weighted mean OES.
Discussion
This is the first study to our knowledge, to determine the influence of neighbourhood school environment on small-area level inequalities in children’s tooth extraction rates using NHS patient management and Ofsted OES data. The findings suggest that tooth extractions are associated with patients’ age and neighbourhood level school overall effectiveness score derived from Ofsted scoring, but not with the patient’s gender or area-level deprivation scores. Whilst the predictive relationship between age and tooth extraction is representative of a national trend (Public Health England 2020a), the relationship between schools OES scores and dental extractions within a neighbourhood proposes a pervasive impact of a school on a child’s dental health right to the home environment.
This research has four important strengths. First, the study involves the use of validated and published data on patient management (Wanyonyi et al. 2017, 2019), which helps to avoid patient recall and selection biases (Hennekens et al. 1987). Similarly, Ofsted inspects all state-funded primary schools of various types (Office for Standards in Education 2020). Therefore, these data provide a complete picture of the primary educational environment within England and reduce selection bias (Hennekens et al. 1987). Second, the study has considered primary school-age children only. Exclusion of the secondary school-age population has allowed the investigators to minimise the confounding effects occurring due to other influencing factors such as peer pressure. Third, this study examines the overall school environment at the neighbourhood level rather than analysing individual school influence on dental health. This enhances the relevance of the study in understanding area-level inequalities in child dental health. Last, the use of weighted OES variable accounts for the different number of schools per MSOA and the different number of pupils per school (Buckley and King-Hele 2014).
However, we also acknowledge a few limitations. First, data were analysed based on an assumption that children attend a nearby school located within their MSOA of home residence. The UPDA data contains information on LSOA codes of patients’ residences, but no such data have been collected about paediatric patients’ schools. However, statutory walking distance regulations within England mean that children are more likely to attend the schools nearby their residence (Department for Education 2014). Second, data did not contain information on patients’ baseline oral health, their chief complaints, or history of previous dental treatments, which restricted a deeper understanding of causal pathways of tooth extraction. Even so, the UPDA data, representing patients’ expressed and normative needs, were proven valuable in understanding disparities in child dental health as they contained information on children’s area of residence contrary to the national data (Office of National Statistics 2015). Last, whilst this research did not investigate individual school influence, it is possible that schools of outstanding and inadequate rankings simultaneously exist within an area. However, the use of area-level variables can help recognise the average school environment within a particular area.
Interestingly, area deprivation was not a significant predictor of tooth extraction in this study. Whilst the previous study based on UPDA adult patient data revealed a significant relationship between tooth extraction and area deprivation (Wanyonyi et al. 2017), the present study involved paediatric patients aged 5 to 11 years. Additionally, the p-value could have been affected by the small sample size (Thiese et al. 2016). All IMD quintiles were not represented in the sample population. No patients belonged to quintile 2. Also, the proportion of patients belonging to the most deprived quintile was only 3.5%, whereas 48% of patients belonged to the least deprived quintile. However, this reflects the national pattern of dental attendance, where the proportion of the individuals from the most deprived quantiles (14.5%) attending the dental service is smaller compared to those from the less deprived areas (90%) (Wanyonyi et al. 2013). Such a pattern in healthcare access, described as the inverse care law, has been persistently observed across England (Gulliford and Morgan 2003; Petti and Polimeni 2011; West Sussex City Council 2018). It can be further argued that the poorest access levels of those belonging to the lowest quintiles could have been the result of children of these groups getting care in the local hospitals rather than in the primary care facilities such as the UPDA. This assumption indicates higher unmet dental needs and far more severe dental health conditions amongst children belonging to the lowest quintiles. This explanation is further reflected in the national data confirming the significant association between the IMD quintiles and hospital tooth extraction rates (Public Health England 2020a, 2021).
This research has several implications. First, it signifies the role of the neighbourhood school environment in understanding geographical inequalities in child dental health. Second, this study confirms the usefulness of the Ofsted OES in dental research. Third, it highlights the need to maximise the use of and enhance the quality of school performance and dental outcomes data to further understand and monitor dental health inequalities. Information on small area characteristics related to children’s homes as well as schools should be routinely collected and openly accessible to the researchers to enable further progress in this research area. Fourth, policymakers should consider promoting and facilitating equal opportunities across all schools to tackle inequalities in child dental health. Fifth and final, further research is required to test the efficacy of the school OES in predicting child dental outcomes at the national level.
Conclusions
A school overall effectiveness score, although a contextual measure, remained a significant predictor of tooth extraction in our study when controlling for individual predictors of dental health. The findings confirm the influence of the neighbourhood school environment on child dental health. Further research is required to assess the role of the neighbourhood school environment in predicting child dental health at the national level.
Data availability
All datasets used for the purposes of this study are open-access datasets and their references are provided in the manuscript. Additionally, all relevant data are provided within the manuscript.
Code availability
Not Applicable
References
Browne WJ, Chris C, Mike K, Rebecca P (2017) MCMC estimation in MLwiN. Centre for Multilevel Modelling University of Bristol, United Kingdom. http://www.bristol.ac.uk/cmm/media/software/mlwin/downloads/manuals/3-00/mcmc-web.pdf
Cabral D, de Melo MM, de Souza WV, Tavares MC, de Lima ML, Jamelli S, Couto GB (2015) Social conditions and high levels of dental caries in five-year-old children in Brazil. J Dent Child (Chic) 82:29–35
Carvalho JC, Silva EF, Vieira EO, Pollaris A, Guillet A, Mestrinho HD (2014) Oral health determinants and caries outcome among non-privileged children. Caries Res 48:515–523
Centre of Multilevel Modelling University of Bristol (2020) MLwiN Version 3.05 (Windows)
da Franca C, Bandeira, Ferreira, Fabiana G, Aparecida MV, Viviane C, Maria ZP, Conceição FR, Ichiro K (2020) School academic climate and oral health (tooth loss) in adolescents. Plos One 15:e0233505
Department for Education DoE (2014) New home to school travel and transport guidance. https://www.gov.uk/government/publications/home-to-school-travel-and-transport-guidance
Department for Education DoE (2019a) Find and compare schools in England: all schools and colleges in England. https://www.compare-school-performance.service.gov.uk/schools-by-type?step=default&table=schools®ion=all-england&for=ofsted [Accessed 24-03-21]
Department for Education DoE. (2019b) Primary school accountability in 2019: technical guide - A technical guide for primary maintained schools, academies and free schools. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachmpent_data/file/854515/Primary_school_accountability_in_2019_technical_guide_2_Dec_2019.pdf
Edasseri A, Barnett TA, Kâ K, Henderson M, Nicolau B (2017) Oral health-promoting school environments and dental caries in Québec children. Am J Prev Med 53:697–704
Fletcher R, Wilkinson E, Cleary P, Blagden S, Farmer S (2019) Did school characteristics affect the uptake of meningococcal quadrivalent vaccine in Greater Manchester, United Kingdom? Public Health 171:24–30
Freeman R, Oliver M (2009) Do school break-time policies influence child dental health and snacking behaviours? An evaluation of a primary school programme. Br Dent J 206:619–625 discussion 616
Gulliford M, Morgan M (2003) Access to Health Care. Routledge, London
Hanneman R, Kposowa AJ, Mark R (2012) Basic statistics for social research. Jossey-Bass, San Francisco
Hennekens CH, Mayrent SL, Buring JE (1987) Epidemiology in medicine. Little, Brown, Boston
IBM_Corporation (2019) IBM SPSS statistics for windows - Version 26.0
Jamieson LM, Do LG, Bailie RS, Sayers SM, Turrell G (2013) Associations between area-level disadvantage and DMFT among a birth cohort of Indigenous Australians. Aust Dent J 58:75–81
Jen B, Sarah, K-H (2014) What is weighting? https://ukdataservice.ac.uk/media/285227/weighting.pdf
Lewis-Beck MS, Alan B, Futing LT (2011) The SAGE encyclopedia of social science research methods. Thousand Oaks, California
Maliderou M, Reeves S, Noble C (2006) The effect of social demographic factors, snack consumption and vending machine use on oral health of children living in London. Br Dent J 201:441–444 discussion 437; quiz 466
Marshman Z, Ainsworth H, Chestnutt IG, Day P, Dey D, El Yousfi S, Fairhurst C, Gilchrist F, Hewitt C, Jones C, Kellar I, Pavitt S, Robertson M, Shah S, Stevens K, Torgerson D, Innes N (2019) Brushing RemInder 4 Good oral HealTh (BRIGHT) trial: does an SMS behaviour change programme with a classroom-based session improve the oral health of young people living in deprived areas? A study protocol of a randomised controlled trial. Trials 20:452
Matsuyama Y, Jürges H, Listl S (2019) The Causal Effect of Education on Tooth Loss: Evidence From United Kingdom Schooling Reforms. Am J Epidemiol 188:87–95
Menard S (2002) Applied Logistic Regression Analysis. Thousand Oaks, California
Ministry of Housing Communities and Local Government MHCLG (2015) English indices of deprivation 2015. https://www.gov.uk/government/statistics/english-indices-of-deprivation-2015
Ministry of Housing Communities and Local Government MHCLG. (2019a) English indices of deprivation 2019- Research report. Available: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/833947/IoD2019_Research_Report.pdf
Ministry of Housing Communities and Local Government MHCLG. (2019b) English indices of deprivation 2019 (IoD2019)- Statistical Release. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/835115/IoD2019_Statistical_Release.pdf
Ministry of Housing Communities and Local Government MHCLG. (2019c) National Statistics - English indices of deprivation 2019. https://www.gov.uk/government/statistics/english-indices-of-deprivation-2019
Moynihan P (2016) Sugars and dental caries: evidence for setting a recommended threshold for intake. Adv Nutr 7:149–156
Moynihan PJ, Kelly SAM (2014) Effect on caries of restricting sugars intake: systematic review to inform WHO guidelines. J Dent Res 93:8–18
Moysés ST, Moysés SJ, Watt RG, Sheiham A (2003) Associations between health promoting schools' policies and indicators of oral health in Brazil. Health Promot Int 18:209–218
National Health Service NHS (2020) Dental treatment for people with special needs. https://www.nhs.uk/nhs-services/dentists/dental-treatment-for-people-with-special-needs/ [Accessed 21-03-21]
National Health Service NHS (2021) Who is entitled to free NHS dental treatment in England? https://www.nhs.uk/nhs-services/dentists/who-is-entitled-to-free-nhs-dental-treatment-in-england/ [Accessed 21-03-21]
NHS Digital Primary Care Domain (2020) NHS dental statistics for England - 2019-20 annual report. https://digital.nhs.uk/data-and-information/publications/statistical/nhs-dental-statistics/2019-20-annual-report
Nobrega J, Dantas E, Ferreira-Filho JC, Limao N, Rodrigues-de-Melo AC, Protasio AP, Valenca AM, Santiago B (2017) Contextual social inequities and occurrence of dental caries in adolescents: a systematic review. Oral Health Prev Dent 15:329–336
Office for National Statistics ONS (2019) Census geography - an overview of the various geographies used in the production of statistics collected via the UK census. https://www.ons.gov.uk/methodology/geography/ukgeographies/censusgeography [Accessed 01-12-2019].
Office for Standards in Education Children's Services and Skills (Ofsted) (2020) Statistical dataset - State-funded school inspections and outcomes: management information. Available: https://www.gov.uk/government/statistical-data-sets/monthly-management-information-ofsteds-school-inspections-outcomes [Accessed 10-09-20]
Office of National Statistics Social Survey Division (2015) Statistical dataset - Children’s Dental Health Survey 2013. https://doi.org/10.5255/UKDA-SN-7774-1
Pattussi MP, Hardy R, Sheiham A (2006) The potential impact of neighborhood empowerment on dental caries among adolescents. Commun Dent Oral Epidemiol 34:344–350
Peres MA, Ju X, Mittinty M, Spencer AJ, Do LG (2019) Modifiable factors explain socioeconomic inequalities in children’s dental caries. J Dent Res 98:1211–1218
Petti S, Polimeni A (2011) Inverse care law. Br Dent J 210:343–343
Public Health England PHE (2018a) Local authority area variation in the oral health of five-year-olds. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/707179/Local_authority_area_variation_in_the_oral_health_of_five-year-olds.pdf
Public Health England PHE. (2018b) National Dental Epidemiology Programme for England: oral health survey of five-year-old children 2017 - A report on the inequalities found in prevalence and severity of dental decay. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/768368/NDEP_for_England_OH_Survey_5yr_2017_Report.pdf
Public Health England PHE (2019) Oral health survey of three-year-old children 2013 - A report on the prevalence and severity of dental decay. https://www.gov.uk/government/publications/oral-health-survey-of-3-year-old-children-2013
Public Health England PHE (2020a) Hospital tooth extractions of 0 to 19 year olds: Episodes of children being admitted to hospital for tooth extractions from 2016 to 2020. https://www.gov.uk/government/publications/hospital-tooth-extractions-of-0-to-19-year-olds [Accessed 13-03-21]
Public Health England PHE (2020b) Oral health survey of 5-year-old children 2019. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/873492/NDEP_for_England_OH_Survey_5yr_2019_v1.0.pdf.
Public Health England PHE (2021) Inequalities in oral health in England. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/970380/Inequalities_in_oral_health_in_England.pdf
Public Health England PHE, Department of Health and Social Care DoHSC., National Health Service England NHS. & NHS Improvement NHS (2021) Delivering better oral health: an evidence-based toolkit for prevention. https://www.gov.uk/government/publications/delivering-better-oral-health-an-evidence-based-toolkit-for-prevention
Rajab LD, Petersen PE, Baqain Z, Bakaeen G (2014) Oral health status among 6- and 12-year-old Jordanian schoolchildren. Oral Health Prev Dent 12:99–107
Samuel SR, Acharya S, Jeevika CR (2020) School Interventions–based Prevention of Early-Childhood Caries among 3–5-year-old children from very low socioeconomic status: two-year randomized trial. J Public Health Dentistry 80:51–60
Sheiham A, Watt RG (2000) The Common Risk Factor Approach: a rational basis for promoting oral health. Community Dent Oral Epidemiol 28:399–406
Spiegelhalter DJ, Best NG, Carlin BP, Van Der Linde A (2002) Bayesian measures of model complexity and fit. J Royal Stat Soc: Series B64:583-639.
The Office for Standards in Education Children's Services and Skills (Ofsted) (2019) School inspection handbook- Handbook for inspecting schools in England under section 5 of the Education Act 2005
The Stationary Office Limited UK Government (2005) Education Act 2005. The Stationery Office Limited. https://www.legislation.gov.uk/ukpga/2005/18/contents [Accessed 02-08-21]
The UK Government GOV.UK (2021) School admissions [Part of: Get childcare: step by step]. https://www.gov.uk/schools-admissions [Accessed 24-03-21]
Thiese MS, Brenden R, Ulrike O (2016) P value interpretations and considerations. J Thoracic Disease 8:E928–E931
Thornley S, Marshall R, Reynolds G, Koopu P, Sundborn G, Schofield G (2017) Low sugar nutrition policies and dental caries: A study of primary schools in South Auckland. J Paediatr Child Health 53:494–499
Thyer, Bruce (2009) The handbook of Social Work Research Methods. SAGE Publications, Inc
UK Data Service Census Support. (2015) Geoconvert tool. 2015 ed.: UK Data Service
UK Data Service Census Support (2018) Look Up Tables: OA 2011 to LSOA 2011 to MSOA 2011 to LAD 2011. https://borders.ukdataservice.ac.uk/easy_download.html
Wanyonyi KL, Radford DR, Gallagher JE (2013) The relationship between access to and use of dental services following expansion of a primary care service to embrace dental team training. Public Health 127:1028–1033
Wanyonyi KL, Sandra W, Gallagher JE (2016) Conscious sedation: is this provision equitable? Analysis of sedation services provided within primary dental care in England, 2012-2014. BDJ open 2:16002
Wanyonyi KL, Radford DR, Gallagher JE (2017) Dental treatment in a state-funded primary dental care facility: contextual and individual predictors of treatment need? PLOS ONE 12:e0169004
Wanyonyi KL, Radford DR, Gallagher JE (2019) Electronic primary dental care records in research: a case study of validation and quality assurance strategies. Int J Med Informat 127:88–94
West Sussex City Council WSCC (2018) West Sussex oral health needs assessment in children and young people. https://jsna.westsussex.gov.uk/assets/starting-well/West%20Sussex%20OHNA%20in%20Children%20and%20Young%20People%202018.pdf
World Health Organisation WHO (2015) Guideline: Sugars intake for adults and children. https://apps.who.int/iris/bitstream/handle/10665/149782/9789241549028_eng.pdf [Accessed 09-12-2019].
Funding
Suruchi G Ganbavale received funding from the University of Portsmouth for a PhD studentship to undertake this research. The funders had no role in the study design, data collection and analyses, or manuscript preparation.
Author information
Authors and Affiliations
Contributions
All authors participated in study conceptualisation and design. Suruchi G Ganbavale curated the data, conducted the formal data analyses and wrote the first draft of the manuscript. Chris Louca, Liz Twigg and Kristina Wanyonyi Kay sought the funding, supervised the research and provided important inputs to the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
Chris Louca is the Director and Head of the University of Portsmouth Dental Academy, whilst Kristina Wanyonyi Kay formerly worked as a Senior Lecturer at this institution. The other authors declare that they have no competing interests.
Ethics approval
This study involved secondary analyses of cross-sectional and open-access data. The methodology did not involve any direct contact with human participants, or the use of any personal identifiers (name, contact number, etc.). Thus, university or external ethics committee approval was not required for this research (ETHICS-10161). This was evaluated using the University of Portsmouth Ethics Screening Tool.
Consent to participate and publication
Relevant ethical permissions including consent to participate and publish were taken as part of primary data collections.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Ganbavale, S.G., Louca, C., Twigg, L. et al. Neighbourhood school environment and dental care needs amongst 5-to-11-year-old children attending a local dental facility in South-East England. J Public Health (Berl.) 31, 1485–1493 (2023). https://doi.org/10.1007/s10389-022-01706-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10389-022-01706-2