Abstract
Aim
This research aims to identify response strategies that non-profit organizations (NPOs) can apply to overcome the barriers that hamper the sustainable use of mobile health (mHealth) interventions in low-resource environments (LREs), such as in Sub-Saharan Africa (SSA).
Subject and method
A qualitative study on mHealth initiatives in SSA is conducted through semi-structured interviews with 15 key informants of NPOs that operate and manage mHealth interventions in this region. The interviews focus on identifying existing barriers and response strategies that NPOs apply to enable sustainable and long-term running interventions.
Results
Building on grounded theory techniques, the collected data guided us towards a process model that identifies four aggregated categories of challenging areas that require response strategies (economy, environment, technology, and user acceptance).
Conclusion
This study provides contributions from and implications for NPOs and researchers. Health practitioners are provided with a knowledge base of what barriers to expect and how to overcome them, to strive for sustainable implementation from the very beginning of an intervention. A process model is identified that structures the response strategies in a time-based agenda of mHealth initiatives and thus makes a theoretical contribution. Overall, this study addresses the need for a theoretical consideration of the “pilotitis” phenomenon, which currently hampers the sustainable implementation and scaling up of mHealth initiatives. While the focus is specifically on mHealth initiatives, the overall findings help prevent discontinuance of projects in the future after the pilot, and help facilitate LREs on their way to sustainable health interventions and universal health coverage.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mobile healthcare (mHealth) enables healthcare service provision via mobile technology, most prominently via smartphone applications (Latif et al. 2017; Silva et al. 2015). Hence, mHealth interventions increase the overall healthcare access of citizens in a cost-efficient manner, while at the same time enhancing patient care (Istepanian and AlAnzi 2020). Furthermore, it offers the opportunity for real-time communication and data transmission and shows promise to improve users’ education, empower them, and increase autonomy (Mechael 2009; Vesel et al. 2015). In a broader scope, mHealth facilitates technological development, improves the country’s overall wealth, and ultimately saves lives (Arief et al. 2013; Wicklund 2019).
These advantages of mHealth can be realized in any context but are specifically valuable in hard-to-reach areas or regions with low resources (Curioso and Mechael 2010; Sondaal et al. 2016). Such health interventions hold the promise to reach more people faster, thus improving healthcare provision in low-resource environments (LREs) through mobile technologies (Mechael 2009). This is vital since, for example, a disproportionate number of maternal and neonatal deaths occurs in LREs, particularly in rural areas (WHO 2004b, 2019).
However, to fully unfold the potential of mHealth implementations, several preconditions are required, including enabling policies, suitable funding opportunities, political stability, availability of experts, and a facilitating infrastructure (Barkman and Weinehall 2017; Lee et al. 2018; Stroetmann 2018). In the context of LREs, the following can be observed: (1) there is a desperate need for improvements in the healthcare system, rendering the application of mHealth to be imperative, and (2) LREs struggle to provide the facilitating factors to enable mHealth success because of the limited infrastructure, scarce resources, shortage of healthcare workers, and limited funding and support (Aranda-Jan et al. 2014; Mupela et al. 2011). These circumstances have led to the failure of many mHealth pilot projects (Clifford 2016; Wallis et al. 2017). A pilot refers to the implementation of a mHealth application at a small scale to test procedures, principles, design, and strategies to generally assess how feasible a scale-up would be (Moore et al. 2011; University of Manchester 2010). For instance, in Uganda, as an example for a LRE in sub-Saharan Africa (SSA), 23 of 36 mHealth projects between 2008 and 2009 did not progress past the pilot phase (Lemaire 2011; Tomlinson et al. 2013). Such failure rates are prevalent in many LREs, and provoked a phenomenon commonly known as “pilotitis,” describing the dissatisfaction of stakeholders with the low number of mHealth applications that went from pilots to prevalent and sustainable applications (Huang et al. 2017; Kuipers et al. 2008; Tomlinson et al. 2013). For example, dissatisfaction with the common “early death” of mHealth pilots leads the government (e.g., Uganda in 2012) to prohibit mHealth projects and require future mHealth applications to offer concepts of interoperability, sustainability, and compliance with laws and requirements in advance (Huang et al. 2017).
Against this background, project-based studies identify several barriers to the uptake of mHealth in LREs (Mechael et al. 2010; van Olmen et al. 2020) or developing countries (Kruse et al. 2019; Latif et al. 2017), while the scale-up research focuses on factors influencing the dissemination of mHealth applications (Sanner et al. 2012; Sundin et al. 2016; Wilson et al. 2014). Scholars who examine the topic of sustainability in LREs focus on single projects and particularly address the respective stakeholders (Chirambo et al. 2019; Dharmayat et al. 2019), policymakers (Opoku et al. 2019), or government (Littman-Quinn et al. 2013; Ndlovu et al. 2014). The conducted studies lack a clear focus on the main initiators and facilitators of mHealth projects: non-profit organizations (NPOs). These organizations often operate and manage mHealth applications, and thus are the main actors in mHealth projects (Banks and Hulme 2012; Botha and Booi 2016; Novillo-Ortiz 2017). Overall, existing research considers a variety of project-based studies that generally display a limited scope, which does not exceed the confines of the defined project, and a limited timeframe that often only addresses the trial phase of the project (Krah and de Kruijf 2016). Research merely focuses on mHealth implementation and scaling, while neglecting how these applications can be sustained (Aranda-Jan et al. 2014; Gutierrez et al. 2017; Tomlinson et al. 2013), meaning that research should focus on the ability of mHealth to function effectively and efficiently in the long term through seamless integration within local technological, economic, social, and environmental conditions (Musango and Brent 2011; Olsen 1998; WHO 2004a). Hence, the related research background reveals a knowledge gap of research focusing on the NPOs’ actions to enable sustainable mHealth interventions.
This study addresses this gap by exploring the phenomenon of “pilotitis” of mHealth interventions in LREs, as well as deriving the successfully applied strategies of NPOs from sustainable mHealth applications as a response to existing barriers to answer the following research question:
-
How can NPOs overcome the barriers of a sustainable and scaled use of mHealth in LREs?
An inductive qualitative research approach is applied to answer this question by conducting interviews with 15 key informants of mHealth projects by NPOs in the SSA region. This region is selected to provide a regional focus, and as SSA is the world’s most impoverished region, it can significantly benefit from mHealth technology to increase healthcare provision to its citizens (United Nations 2018). The research approach is based on grounded theory techniques to analyze the data attained. The aim is to identify response strategies towards the barriers that hamper the sustainable use of mHealth and hence support NPOs with guidance to enable sustainable mHealth interventions.
Research approach
Since research on mHealth is still limited in scope, this study follows a qualitative approach to offset the scarcity of available literature on sustainable mHealth interventions (Silva et al. 2015; Yin 2016). Qualitative research has proven especially useful in unveiling new phenomena in mHealth (Arino et al. 2016).
For this study, mHealth is defined as healthcare interventions characterized by using a mobile device (e.g., cellphones, tablets) to provide health information and services (Bonnell et al. 2018; WHO 2017). This also aligns with the approach from van Dyk (2014), who characterizes mHealth as part of electronic health, telehealth, and telemedicine, with the addition that mHealth uses mobile devices to deliver health-related services. Hence, NPOs that operate and manage mHealth intervention include a wide range of functionalities and purposes. Because the technology enables the communication and real-time data transfer with participants such as patients or primary health facilities anytime from anywhere, the healthcare service quality increases at a lower cost (Bajwa 2014; Iribarren et al. 2017; Marcolino et al. 2018; Steinhubl et al. 2015). Possible application areas of mHealth include managing chronic diseases, improving access to health services, clinical diagnosis, treatment adherence, and patient communication and education (Marcolino et al. 2018).
It is crucial to consider the environmental setting when investigating mHealth initiatives in LRE. The qualitative data is collected in natural settings, and thus indicates a realistic perspective (Miles et al. 2014). Overall, the research approach comprises three steps (see Fig. 1) described in the following.
Data collection
A qualitative empirical study was conducted to identify the response strategies of NPOs that have been successfully applied in the context of sustainable mHealth projects as a reaction to the barriers. Conducting this research through semi-structured key informant interviews offers the opportunity to generate valuable and insightful information on this unfamiliar topic, to obtain data based on the research participants’ retrospective knowledge (Adams 2015; Gioia et al. 2013; Kumar 1989).
For the study, representatives of NPOs were interviewed with regard to factors influencing mHealth projects’ success in LREs. Respondents are key informants who are knowledgeable about their organization’s mHealth projects. It was ensured that each key informant interviewed has several years of professional experience in the domain, and is mainly involved in their organization’s mHealth projects to guarantee the informants’ statements quality. It was also assured that the selected key informants are experts from organizations of health interventions. Therefore, it can be assumed that this group can assess the impact of mHealth and evaluate barriers and obstacles and corresponding successful response strategies in the health context.
A stepwise research approach was conducted to select the final sample of key informants. Along with an environmental scan of mHealth initiatives in SSA, in the first step, personal contacts, social, and career networks were used to attract potential key informants with an interview request. The four-point approach suggested by Robinson (2014) was applied to guarantee a meaningful sample. Firstly, the sample universe was defined as the following: employees of NPOs who have valuable knowledge or manage mHealth applications for development in the SSA region. By defining a broad possible sample universe, the selection process did not significantly restrict the potential sample, to consider a heterogeneous group of participants and strengthen generalizability (Robinson 2014). Secondly, it was aimed to obtain a sample size that reaches the saturation limit to ensure validity (Corbin and Strauss 2015; Guest et al. 2006). Thirdly, the targeted sampling technique was used as a strategy to identify open-ended and thus information-rich research topics based on the pre-defined sample universe by pre-screening the mHealth landscape in SSA, e.g., US Aid (2015) (Palinkas et al. 2015; Patton 2002). Fourthly, the identified potential key informants were contacted via email or digital platform with an interview request and a flyer that summarized the research project.
In the second step of the data collection process, a preliminary questionnaire was sent to the key informants to prepare for the interviews, along with a privacy statement. An interview was scheduled if the interview request was answered positively. The interviews were conducted between February and September 2020 using online communication software, recorded with the respondents’ consent, and transcribed immediately after completion. On average, the dialogues lasted about 45 min, with a minimum length of 28 min and a maximum length of 66 min. The interviews were based on a semi-structured interview guide so that the respondents had room to express their ideas. The interview was structured around four different areas — please see Table 1.
Following Yin (2016), the interview questions were designed to be free of suggestive elements to avoid influencing the respondents. The questions mentioned were considered as leading questions to provide a basic structure. However, the participants’ responses guided the interview, and revealed further aspects and follow-up questions.
After the first interviews, a theoretical sample was drawn based on simultaneous data analysis, which allowed for concept development and further data collection (Corbin and Strauss 2015; Urquhart et al. 2010). The interviews were conducted until no new viable information was obtained, and thus information saturation was reached (Corbin and Strauss 2015). After the privacy statement had been signed, all interviews were recorded and transcribed. The selected sample is heterogeneous in several respects. As shown in Table 2, the sample includes four project managers, four technical specialists, four medical specialists, two operation managers, and one funding manager. Together, the NGOs considered are primarily involved in mHealth projects in 23 sub-Saharan countriesFootnote 1 (Ethiopia, Eswatini, Kenya, Uganda, Madagascar, South Africa, etc.). The end-user of the discussed mHealth projects include health workers (e.g., an app to support automated diabetes risk calculation and patient management), the general public (e.g., automated symptom checking through a digital assistant), employees of companies (e.g., real-time stock management of vaccines and health supply chain management), and the government (e.g., a platform for health education content that governments can provide to health workers). The mHealth interventions mentioned had several users ranging from 30 to over 127,000. However, the number of users is not yet collected for some applications because they are still in the development or testing phas
Data analysis
After collecting the data, the transcripts were analyzed in the third step using an inductive approach. This means that the collected data leads to the emergence of concepts without ex-ante theorizing or conceptualization before the data collection (Yin 2016). Grounded theory techniques are used to generate insights (Charmaz 1990; Gioia et al. 2013; Miles et al. 2014). Additionally, to avoid influences on informants the development of new theories is encouraged, instead of staying within patterns and applying data to known theories (Gioia et al. 2013). Instead of relying on the basic assumption of social constructivism as described by Charmaz (1990), this study also takes up the proposal of Gioia et al. (2013) and assumes that people within an organization are knowledgeable agents. This assumption emphasizes the agents’ point of view and places the researcher in the role of a neutral narrator who collects the agent’s knowledge and experience without influencing them.
The data were coded to structure, extract, and categorize the rich information of the interviews. The coding was performed simultaneously with the data collection for analytical purposes. This approach enables reflecting the ongoing data collection and cleaning it for potential blind spots (Miles et al. 2014). In the first analysis, first-order concepts were developed close to the underlying information without accumulating it (Gioia et al. 2013). This open coding provides an overview of the rich data and interpretation (Saldaña 2015). The second-order analysis then focused on aggregating first-order concepts based on similarities and differences to reduce coding and classify them into conceptual categories (Gioia et al. 2013; Saldaña 2015). In the following step, the commonalities in second-order topics were brought together in the aggregated dimensions. This process resulted in a data structure that illustrated the progress of aggregation from raw data to an empirical structure (Gehman et al. 2018; Gioia et al. 2013). A conceptual framework was established at the same time as the data analysis. While the coding progressed, the framework was iteratively redesigned, and alternatives were generated.
Results
The data analysis guided towards four aggregated dimensions that depict the thematic areas of the response strategies towards barriers to sustainable mHealth interventions.
The aggregated dimensions are based on the 1st-order concepts that define specific responses. As depicted in Fig. 2, several specific response strategies belong to one 2nd-order theme. For each dimension, the data indicated two themes.
The process of response strategies
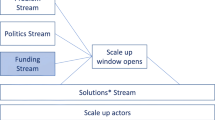
Furthermore, the data identified a relationship between the four dimensions (see Fig. 3). The assigned strategies of the themes are necessary for different stages of a mHealth project.
In the project setup stage, the strategies regarding the economy and environment play an essential role. These response strategies ensure financing, consider costs, ensure the government’s involvement, and establish partnerships. As soon as these strategies are successfully addressed, the implementation contains barriers concerning the application itself; therefore, response strategies address the technology by ensuring a customized design and data management. Lastly, during the application process, the users play an essential role in deriving a sustainable use of the mHealth application. Hence response strategies concern user acceptance through user involvement and provision of training to them.
Economic strategies
Based on the data, economic strategies are identified that can be clustered into two types of actions. First, it is crucial to ensure financing for the mHealth intervention, while second, it is also vital to consider the project’s costs.
Ensuring financing for mHealth interventions is one of the most significant challenges for sustainable implementation. Since the development and scale-up of the mHealth project are dependent on sufficient funds for the NPOs, the lack of financial support leads to a difficult situation, and is a substantial barrier. Hence, fundraising, which is often not their most robust competence, becomes an fundamental task for NPOs.
One beneficial strategy is to engage with international NPOs to acquire funding and support. They can ensure donation-based funding through their financial standing, and provide a network of possible donors. Furthermore, not restricting the donation requests also embraces the possibility of integrating small donations from other sources and hence increases funds and helps raise the intervention’s vulnerability. To ensure such long-term financial support and strategic orientation, the key informants emphasized the importance of a business model to cope with the challenges of LRE. “Now we have a sustainable model that works with the state. The state is now paying; the state is actually the one managing their project” (MH11). As many key informants point out, there is the possibility of transitioning the project to the state so that the government takes the lead. This ensures long-term commitment and sustainability, and carries the burden of financial expenses. Nonetheless, convincing governments or other stakeholders to invest in the mHealth application is a challenging task, since financial resources and income are limited in LRE, and the state must choose between various investment opportunities. A project manager (MH9) states that as a “[…] low-middle income country, we are struggling to implement evidence-based, cost-effective interventions such as vaccinations [...]. So, if you imagine that we are struggling to deliver those services to people, the government’s willingness to take the risk on an unproven health application with uncertain health benefits is… there is a very low appetite for that. […] It’s just that they can’t make an investment decision unless there is compelling evidence” (MH9). It is vital to underpin the proposal with compelling evidence to reallocate scarce health budgets from proven interventions to new implementations. This evidence allows stakeholders to invest in new technologies.
In addition to ensuring finance, mHealth interventions also need to consider the specific cost occurring at the start and during the project, especially with regard to the technological infrastructure. Mobile devices represent resources that are not commonly available; however, they pose as basic requirements for the use of digital applications. A project manager (MH9) adds that “[…] 60% of the population live on less than $1.90 a day” and thus are not able to afford a basic mobile device. Therefore, mobile devices are often the initial cost drivers in the project. It is fundamental for the NPOs to examine the potential intervention target group and analyze how many of those own or have access to a mobile device before implementing a mHealth project. The mobile devices operate with a battery, but the battery’s capacity is limited, and thus a need for charging options occurs. Even if mobile devices are available to the users, the fundamental precondition is the power supply because “[…] the rates of electrical penetration are low […]” (MH12). When healthcare workers cannot use the application because the battery is low, this runs counter to the project’s whole purpose and value. Providing a response strategy to this issue is quite difficult for users who live in or travel to distant rural areas. Substituting power supply through alternative mobile charging equipment (e.g., solar) enables traveling to rural areas. When the mHealth application targets healthcare workers, it is possible to provide charging options for remote charging, including solar panels and power banks.
Environmental strategies
While it is important to consider economic strategies, there is also a need to develop strategies that consider the environment in which the mHealth interventions take place. In this environment, the most important stakeholder is “definitely the government” (MH1). They can decide which projects are enabled to be implemented and which projects are neglected. A technical specialist (MH15) also emphasized that “whenever there is something new that we are about to implement in this area, they [the government] have to know.” Therefore, involving the government and thus the ministries of health and their representatives is vital in establishing mHealth applications in LREs, and often the only way to involve health facilities such as clinics and hospitals and corresponding personnel, such as doctors, nurses, and health workers. In conjunction with this, the government also formulates requirements and needs that the mobile application must fulfill to be accepted and sustained. Thus, as MH11 states, they need to “look at all the requirements and build a dashboard and build an application tool for them […].” Furthermore, “policies can change. We have different policymakers because you are working with the state, with the government, you know. If you are working with the government, it’s always difficult because you get people... new people like every 4 years or every 3 years, and they come with their policy. That can affect the project as a whole as well” (MH11). Considering these requirements is critical to ensure the sustainable use of technology. Responding strategies include constant communication with officials to gather their feedback on requirements and needs. It is vital to ensure compliance with national technology standards and align with federal programs and the national health information system in order to react to changing demands promptly. Hence, contextualizing the application for the target country is a necessary action to avoid sanctions and failure. Another issue mentioned by the key informants is the lack of sufficient knowledge by the government employees, departments, and health workers. This leads to a limited understanding of the value and functionality of the mHealth application, but also inhibits the transfer of applications or tasks to the state. It is necessary to increase the employees’ knowledge level, which is scarce in these departments, to solve this issue and preserve the option to transition the application to the state. Training allows the teaching of basic software development or management. Retaining the management of the application and infrastructure within the NPO while building government employee capability can facilitate the government during a transition phase and result in a layered transition, starting with handing over management and coordination activities while keeping technical operations in the NPO for a prolonged time.
In addition to engaging with the government, collaboration between health initiatives and local partners is necessary. If there are various mHealth applications available, all should keep in mind that they drive for the same objective: “[…] to really expand this implementation to a larger patient group […]” (MH2). Collaboration with other initiatives results in diffusion and increases the value and relevance of each project. Therefore, cooperation with local partners increases the distribution as it enhances the connections to the local community.
“And the other approach is to work via local partners in [name of country]. For example, with [name of a local company]. They are digitizing pharmacy shops and are therefore a natural contact partner because, on the one hand, they are directly connected to the supplier, but on the other hand, they also have direct contact to patients where they can present new digital solutions” (MH1).
The problem of high data costs is one barrier that can be overcome through partnership. This barrier prevents potential users from using the application or blocks data transfer and the installation of updates. One key informant describes that an essential point for scale-up is the cost consideration. For example, they do not load data costs on the user’s SIM card but have donors pay for data costs.
Therefore, to prevent overburdening costs for users, establishing partnerships to shift users’ fees to other stakeholders ensures that users can utilize the application. In this instance, possible stakeholders include NPO, network providers, or other organizations or institutions that can cover the accrued data costs.
Even though the local corporate landscape offers a wealth of partners, there is also the need to consider the competition in the SSA region to understand that “[…] ecosystems have developed in the meantime, where they don’t appreciate every new application and say ‘Oh yes, great that you thought of us,’ but of course, they develop their own solutions on the domestic market”(MH1). MH5 further elaborates, “[…] I think the biggest issue in this field of work is, as you said, there are many mHealth solutions […].” Engaging with competing mHealth projects to explore collaboration methods to leverage existing applications or features enables mHealth interventions by NPOs to focus on their application’s essential parts. Through this, a direct value for the user is created while saving costs and time. Furthermore, collaboration with other mHealth projects offers the possibility to engage in in-depth partnerships, merging the mHealth applications to provide a more comprehensive service without straining the user with too many applications.
Technological strategies
The need for mHealth projects to respond to technological barriers was further identified. A part of these challenges includes that “this landscape is moving very quickly. The operating systems on the mobile devices, hacking, all of that stuff moves very quickly” (MH14). The fast-paced evolving and changing of the technological landscape need to be dealt with because otherwise, “within a year or 2 years, whatever it is, the app will just stop working” (MH14). Therefore, it is vital to ensure the continuous maintenance of the application. Updates can be supplied fast and frequently to guarantee the application’s stability and availability, while allowing incremental refinements to follow the dynamic environment.
“We also have these constant changes on the app because we have to keep following the dynamic of the new approaches. So, every time we decide to implement a new approach, it means to change [update] the app” (MH15).
Such maintenance can also include the optimization of a design. To avoid overwhelming users, the key informants emphasize designing simple applications that follow a user-centric design approach. Implementing and scaling up with a simple application allows ensuring operability and ease of use.
“[…] based on that we learned to make simple apps, to do one thing very good, make a simple app that works perfectly and from there you can add features. And that’s why [name of the application] is so simple, and it works” (MH8).
To ensure usability for every user and address illiteracy, alternative forms of design and interfaces should be incorporated. While a user-centric design is important to ensure adoption, a stable background functionality ensures retention. A limiting factor is a weak network or mobile internet connection in the SSA region. It can impede the success of mHealth applications; as MH11 points out, “we have connectivity issues. ‘Cause you know they need internet to send the reports, so there are some communities, remote communities, right, that... they don’t have network and that “[…] sometimes it [the connection] is like stopping for some hours or 1 hour or 2 hours” (MH7). Therefore, the application should incorporate missing internet access or limited connectivity. Integrating offline functionality in the mHealth intervention resolves this issue. Assuring a synchronization feature that synchronizes the data when the internet connection is available again also enables the mHealth project to stay connected with delayed data transmission. Moreover, allowing the application to send data through different channels, mobile networks, or mobile data allows for substitution of the network depending on the availability.
Even if the data is stored and synchronized, key informants argue that data quality is an issue of most mHealth applications, which leads to incorrect and meaningless data and reporting. Frequently, users do not manage “to read properly because they fill the form [out] without reading it” (MH15). Equally concerning is when “[…] regarding data quality, we have the challenge that the user can insert data, like fake data, and if we don’t open our eyes to that, we will report data that is not accurate” (MH15). Several approaches are prevalent to increase the data quality to match the expected reporting standards. First, implementing a step-by-step design to guide users through the process and prohibit them from skipping fields or leaving blanks facilitates data quality. Second, communicating the data’s value to users can help raise support for data collection and improve the quality of the inserted data. These solutions can be supplemented with further training and a supportive design approach.
“You know, more dropdowns, more selections, select options than having to write text. So, things of that nature. I guess, you know, checkboxes, things of that nature. I guess things they try to do to make it more user-friendly” (MH12).
The interviewees explain that collecting and analyzing technical meta-data leads to a better understanding by the users and tracks their application behavior. Since meta-data do not require the user’s attention, they can be continuously compiled and provide uninfluenced insights on the user’s work process and utilization of the mHealth application. This is incredibly impactful in circumventing people’s cultural habits from the SSA region, as they are not accustomed to providing negative feedback.
“Just by having a look, for example, at when someone opens up the app and how much time they spend on the app, we have found amazing information. For example, [if] they [are] not using it during their office hours, they’re using it from between 6 o’clock and 8 o’clock in the morning and after 7 o’clock at night. They are not using it as a guide, they are using it to read up or to refresh their memories about information. So, by feeding that information back to the content providers, we say to them [the developing team]: ‘don’t aim this as a quick reference guide, aim this as a tool that people are using after-hours.’ And we build for them [the users] just a simple function that allows you to create favorites. So, if you open up the app, you can click on a page and mark it as a favorite. That has become such a hit because we understand how the user is using the app” (MH14).
Analyzing the data to refine the application and learn about the usage increases the value of the mHealth intervention. Nonetheless, it is also necessary to offer value to the government and cooperating partners. Providing data and reports enable governments to monitor the current healthcare situation. By providing dashboards to the representatives, the impact of the mHealth application becomes visible and quantifiable, and informed decisions can be made. Reporting data can often be done in real-time, increasing the quality and pace of decisions and enabling the government to react to incidents promptly. Furthermore, ensuring harmonized data through the mHealth application and conducting analysis and visualization steps to generate reports further increases the value of the tool for the government.
User acceptance strategies
An application must serve and maintain a large number of users to thrive. Therefore, it is vital to consider the user demands for interacting with the application because “if there is nothing in it [if there is no impact] for the user, then you can be sure that […] they won’t use it at all” (MH5).
If this is not the case, they will be reluctant to embrace it and stop using it promptly. The main focus while developing and refining the application is promoting its value and making it visible to the target group. Thereby, the value can take different shapes, ranging from providing incentives for the uptake and sustained usage to facilitate work and data collection. When a direct value can be illustrated to the user, there is also the need to ensure that the value is being promoted and maintained permanently. If the mHealth intervention does not suitably address the user’s needs, the initially promised value will not convince them to use the application consistently.
An iterative design approach with constant updates allows the application to change to increase the fit between the user and the application. Adjustments of features should be based on data as well as on experience. This experience can be derived through user feedback. Repeating demand for feedback supports the refinement of the application and ensures the acceptance of updates by users. Establishing an agile work methodology makes it possible to promote and facilitate this style of work. The collected feedback is valuable, but should always be considered holistically and be dependent on financial resources. Prioritization is necessary, and the refinements need to be subordinated to the overarching idea of a user-centric application.
“So we launched this app 2 weeks ago, so now that’s why I had this one intern who was supposed to go to [country] to talk to the users, the end-users, to understand their feedback and what can change, what is good, what is not because of course, we realize that this is just the first version and based on feedback we can, of course, change it and make it better” (MH8).
Involving users in refining the application and ensuring their value is vital for the success of the mHealth project. In addition, there is also the need to develop their capabilities. As MH12 points out, “I guess, with the lack of phone management skills, as I mentioned, some of them are a bit resistant to use the technology.” This problem leads to the fact that “[…] we have the challenges of people accepting to use the application” (MH13).
Dealing with the low technical knowledge of users increases the adoption rate and prevents rejection of the application. Providing training opportunities at the intervention’s initial deployment ensures that users understand the application and use it correctly. Furthermore, the training offers the possibility to ensure that users can utilize a mobile device and fulfill or achieve the necessary requirements to execute the demanded tasks successfully. The training also provides a point of interaction and enables the project to ensure that users have a common understanding of the mHealth intervention.
“Yes, we have a 5-day training for when we give them the devices. Yes, we make a follow-up after the 5 days, maybe a week, just to make sure everyone understands everything and why they are using the devices. So, once we support them, then it becomes easier, second week, third week, people will have caught up, and they are able to enter the data” (MH13).
Educating users to ensure technical literacy facilitates the uptake of the mHealth application. However, one should not neglect the fact that “[t]he health worker can decide not to use the tool because it’s not part of... it’s not embedded in his work process” (MH11). Users need to be convinced to utilize the application and integrate it into their work. If the mHealth project does not manage to ensure the application’s sustainable use, it will be unsuccessful.
“And when that’s not the case, and even when it is the case, we always provide training on the app itself, what the goal of the app is, how you can use it, and then we also provide refresher courses to make sure that people stick to it and really integrate it into their routine” (MH5).
“I mentioned we did a continuous capacity-building. Because training a health worker once and just let them then use the application is never going to work because we tried that in 2015” (MH11).
To solve the problem of abandoning the application, continuous and holistic training is necessary. After the initial training, regular training sessions and constant reminders to users are fundamental to guarantee that they “[…] stick to it and really integrate it into their routine” (MH5). The training can be provided through different channels, including eLearning opportunities, training in cooperation with the government, and on-site training. Continuous training is critical, because constant refinement and addition to the application are necessary. Thus, follow-up training provides the opportunity to ensure sustainable use while also facilitating the user in properly operating the application with the added features.
Discussion
This study provides insights into the strategic behavior of NPOs and derives strategies to cope with existing barriers to mHealth sustainability. The results enable other NPOs and stakeholders for mHealth in low-resource environments (LREs) to go beyond the pilot phase and ensure sustainable dissemination of mHealth interventions. Thus, the results contribute to addressing the prevention of the failure to sustain mHealth applications, which is costly and slows down the inevitable goal of controlling and defeating disease (Mukisa et al. 2017; Tomlinson et al. 2013). The key contributions are identifying the action that leads to a sustainable mHealth initiative that develops beyond the pilot stage. However, the individual barriers that hamper sustainability and scalability are not the focus of this paper. The paper rather acknowledges the problemizing areas in general, but indentifies response strategies that suit as practical guidance for NPOs. In the following, the process model and its theoretical contributions are discussed shortly before alluding to the practical implications of how NPOs can ensure that their mHealth project exceeds the pilot state and reaches scalability and sustainability.
Theoretical contributions
This study adds new knowledge to the existing literature and provides a theoretical contribution. By identifying response strategies for long-term mHealth success, the results contribute to fight back prevalent “pilotitis” and provide a knowledge foundation for future mHealth success. This adds knowledge to the existing literature (e.g., Chib et al. (2015)) by providing precise response strategies tailored to the operating NPOs, as such organizations are the facilitators that cope with mHealth sustainability barriers in LREs. The identified strategies underpin the literature’s solutions, e.g., the call that mHealth projects collaborate with and be integrated into the national health information systems (Labrique et al. 2018; Lemaire 2011) or the call for user-centric design (Clifford 2016) and generation of evidence (Källander et al. 2013). The interviewed key informants further complement past research by emphasizing the need for continuous holistic training for sustained use, increasing data quality, and the appropriate use of the generated data for refinement and analysis. Thus, this study contributes by adding new response strategies and providing a more holistic set of response strategies to cope with the existing barriers of mHealth in LREs. This allows for a more informed decision regarding the strategic direction of mHealth projects, and facilitates the NPOs in successfully establishing a mHealth intervention in the area.
The main focus on NPOs extends the emerging research on sustainability by offering new insights to the hitherto neglected perspective of the effect of NPOs on mHealth project success and sustainability. Previous research on sustainability centers on policymakers (Opoku et al. 2019) while neglecting those actors that develop and implement sustainability response strategies. The focus on NPOs makes it possible to examine the actors affected by the existing barriers but who cannot change or influence them; thus, there is a need to develop strategies to cope with these barriers. In the primary step, the study extends the existing literature by illuminating context-specific obstacles that impede the sustainability of mHealth in LRE. Barriers specific to LREs include missing charging options through the lack of electricity supply and power outages, insufficient network connectivity for the transmission of data and updates, illiteracy, and low technical knowledge impeding the use of the mHealth applications. After that, through examining the NPOs, new insights and response strategies can be derived. The response strategies’ interrelations and processes are structured and illustrated within a process model for mHealth sustainability.
Further, this study contributes to mHealth research by establishing a process model towards achieving universal health coverage. The introduced dimensions are derived from the mHealth experts’ knowledge, and extend existing frameworks with regard to the identified barrier dimensions (Fanta and Pretorius 2018; Leon et al. 2012) and advance the research of Braa et al. (2004) and Madon et al. (2009), who argue for the value of scalability and sustainability while emphasizing the diverging needs to achieve it. This study provides a new perspective on the sequential importance of response strategies to reduce the barriers for mHealth applications in LREs. The illustrated phases enable researchers to benefit from a more differentiated process of reaching sustainable mHealth, making progress towards universal health coverage, and narrowing their scope of examination to a single phase to understand this topic better.
Practical implications
The findings of this study highlight the importance of collaboration, which results from the desired shift from establishing a new mHealth intervention — which often remains stuck in the pilot stage — towards extending and improving the existing sustainable applications to provide value to as many users as possible (Braa et al. 2004; Walsham 2020). Implementers are confronted with manifold barriers, as mHealth requires an enabling environment with interplay between technology, society, and institutions to achieve positive results and make a lasting impact (Walsham 2020). These barriers often overwhelm stakeholders and result in an early-stage failure of the initiative (Huang et al. 2017). It is critical for NPOs to know which areas are likely to face barriers and where they stand in the process flow to achieve sustainability.. This study identifies a sequential process model with different dimensions of response strategies at each stage of the process. The specific response strategies are fundamental best-practices that proactively address the existing barriers. Based on the findings, NPOs are advised to include these four identified dimensions into their overall business strategies. This, for example, involves taking into account the multiple stakeholders who need to be involved when implementing a mHealth application. With regard to the application’s design, it is advised to focus on the user to ensure adoption and sustain usage through an iterative design approach that involves the user from the beginning onwards. In addition, contrary to many applications, mHealth applications have multiple sides that need to be considered in the design process. Governments or supervisors demand data, while users demand features and usability. The funding parties and donors request evidence, and the mHealth project NPO gathers feedback through data. Thus, it is possible to argue for a stakeholder-centric design rather than a user-centric design because all stakeholders use the application and need to be equally satisfied. Overall, all stakeholders must be proactive and collaborative in their efforts for continuous progress to improve the general healthcare in the LRE and for digital health. MHealth can assist in these inter-organizational communication efforts (Asi and Williams 2018).
Limitations and future research
This study is not free of limitation, and provides a reference for future research.
First, the study selected Sub-Saharan Africa (SSA) as one region of LREs. However, this region distinguishes itself from other developing areas like South Asia and Latin America. LREs share similarities in income, low availability of technology, poorly developed institutions, and low education (Nafziger 2012). Nonetheless, there are apparent differences that need to be considered and lead to unique preconditions in every area (Nafziger 2012). Especially with regard to mHealth, SSA has a unique position due to the lack of smartphone ownership, limited internet connectivity, high mobile data costs, and little consumer readiness (GSMA 2019b). These essential preconditions for mHealth diverge strongly between the areas. Thus, future research is needed to confirm the findings of the study in other contexts.
Second, it is feasible to assume that some response strategies apply to other fields of Information and Communication Technology for Development (ICT4D), such as financial technologies, agricultural technologies, and logistic technologies. Still, several findings closely correspond to mHealth (GSMA 2019a; Walsham 2012). For example, governmental involvement is also crucial for mHealth because the state constructs clinics, employs doctors, and provides the mobile network as part of the basic infrastructure, and thus a close collaboration is necessary to ensure optimal healthcare delivery. Since mHealth can only support the goal of universal healthcare coverage by the government and transitioning the application to the state for sustainability is a widely considered option for NPOs, mHealth is in a unique position, thus relying on particular response strategies to achieve its goals (Opoku et al. 2019; Sanner et al. 2012; World Bank 2016). However, future research should explore whether these strategies are also applicable in different ICT-based industries, since certain strategies target specific conditions that are equally detrimental to other ICT4D interventions (e.g., infrastructural constraints, lack of technological literacy). However, quantitative research approaches, such as that of Alaiad et al. (2019), could further validate the results.
Third, the response strategies provide first-step actions to cope with barriers to sustain mHealth applications. Nevertheless, the proposed techniques can lead to new problems. In this instance, providing devices to healthcare workers can lead to adding personal content to these devices or putting their lives in danger through crime and robbery (Aranda-Jan et al. 2014). Another example is the data itself. It is vital to generate, use, and provide data, but as collaboration increases and partnerships ascend, the question of data ownership arises (Kostkova et al. 2016). Thus, second-step response strategies should be developed to deal with the emerging barriers. This provides a possibility for scholars to apply response strategies and examine the emerging barriers to derive new strategies for mHealth sustainability.
Conclusion
This study investigates response strategies for NPOs to cope with barriers that impede the uptake of mHealth applications in LRE to operate a sustainable mHealth application. The response strategies are derived from mHealth applications at different stages of their respective development to reach sustainability or already established sustainability, and thus contradict the prevalent pilotitis. The strategies can be assigned to the economic, political, technological, and user acceptance dimensions. All four dimensions cope with two precise areas that classify the derived response strategies in a process model. The results contribute to research as they derive results from the NPO perspective and systematically structure response strategies. Further, the derived response strategies put NPOs in a position to self-reflect on their current state of operations with regard to sustainability and to derive suitable response strategies for the situation. This enables project managers to make informed decisions and proactively consider potential barriers in their business strategy. Overall, this study contributes to preventing pilotitis in the future and facilitates LREs on their way to achieving universal health coverage.
Availability of Data
Not applicable.
Code Availability
Not applicable.
Notes
The SSA region comprises a total of 46 countries located south of the Sahara, i.e., half of all countries were covered by interviews.
References
Adams WC (2015) Conducting semi-structured interviews. In: Hatry HP, Wholey JS, Newcomer KE (eds) Handbook of practical program evaluation, 4th edn. Jossey–Bass, San Francisco, CA, USA, pp 492–505
Alaiad A, Alsharo M, Alnsour Y (2019) The determinants of M-health adoption in developing countries: an empirical investigation. Appl Clin Inform 10:820–840. https://doi.org/10.1055/s-0039-1697906
Aranda-Jan CB, Mohutsiwa-Dibe N, Loukanova S (2014) Systematic review on what works, what does not work and why of implementation of mobile health (mHealth) projects in Africa. BMC Public Health 14:188. https://doi.org/10.1186/1471-2458-14-188
Arief M, Hai, Thanh NT, Saranto K (2013) Barriers to and advantages of e-health from the perspective of elderly people: a literature review. FinJeHeW 5
Arino A, LeBaron C, Milliken FJ (2016) Publishing qualitative research in academy of management discoveries. Academy of Management Discoveries 2(2):109–113. https://doi.org/10.5465/amd.2016.0034
Asi YM, Williams C (2018) The role of digital health in making progress toward sustainable development goal (SDG) 3 in conflict-affected populations. Int J Med Inform 114:114–120. https://doi.org/10.1016/j.ijmedinf.2017.11.003
Bajwa M (2014) mHealth security. Pak J Med Sci 30:904–907. https://doi.org/10.12669/pjms.304.5210
Banks N, Hulme D (2012) The role of NGOs and civil society in development and poverty reduction. Brooks World Poverty Institute Working Paper 171:1–38. https://doi.org/10.2139/ssrn.2072157
Barkman C, Weinehall L (2017) Policymakers and mHealth: roles and expectations, with observations from Ethiopia, Ghana and Sweden, Global Health Action 10(sup3):1337356. https://doi.org/10.1080/16549716.2017.1337356
Bonnell S, Griggs A, Avila G, Mack J, Bush RA, Vignato J, Connelly CD (2018) Community health workers and use of mHealth: improving identification of pregnancy complications and access to care in the Dominican Republic. Health Promot Pract 19:331–340. https://doi.org/10.1177/1524839917708795
Botha A, Booi V (2016) mHealth implementation in South Africa. In: Cunningham P, Cunningham M (eds) 2016 IST-Africa Conference: 11–13 May 2016, Durban, South Africa. IEEE, Piscataway, pp 1–13
Braa J, Monteiro E, Sahay S (2004) Networks of action: sustainable health information systems across developing countries. MISQ 28:337–362. https://doi.org/10.2307/25148643
Charmaz K (1990) ‘Discovering’ chronic illness: using grounded theory. Soc Sci Med 30:1161–1172. https://doi.org/10.1016/0277-9536(90)90256-R
Chib A, van Velthoven MH, Car J (2015) mHealth adoption in low-resource environments: a review of the use of mobile healthcare in developing countries. J Health Commun 20:4–34. https://doi.org/10.1080/10810730.2013.864735
Chirambo GB, Muula AS, Thompson M (2019) Factors affecting sustainability of mHealth decision support tools and mHealth technologies in Malawi. Inform Med Unlocked 17:100261. https://doi.org/10.1016/j.imu.2019.100261
Clifford GD (2016) E-health in low to middle income countries. J Med Eng Technol 40:336–341. https://doi.org/10.1080/03091902.2016.1256081
Corbin JM, Strauss AL (2015) Basics of qualitative research: techniques and procedures for developing grounded theory, 4th edn. Sage, Los Angeles, CA, USA
Curioso WH, Mechael PN (2010) Enhancing M-health with South-to-South collaborations. Health Aff (Millwood) 29:264–267. https://doi.org/10.1377/hlthaff.2009.1057
Dharmayat KI, Tran T, Hardy V, Chirambo BG, Thompson MJ, Ide N, Carlsson S, Andersson B, O'Donoghue JM, Mastellos N (2019) Sustainability of 'mHealth' interventions in sub- Saharan Africa: a stakeholder analysis of an electronic community case management project in Malawi. Malawi Med J 31:177–183. https://doi.org/10.4314/mmj.v31i3.3
Fanta GB, Pretorius L (2018) A conceptual framework for sustainable eHealth implementation in resource-constrained settings. SAJIE 29:132–147. https://doi.org/10.7166/29-3-2055
Gehman J, Glaser VL, Eisenhardt KM, Gioia D, Langley A, Corley KG (2018) Finding theory–method fit: a comparison of three qualitative approaches to theory building. J Manag Inq 27:284–300. https://doi.org/10.1177/1056492617706029
Gioia DA, Corley KG, Hamilton AL (2013) Seeking qualitative rigor in inductive research. Organ Res Methods 16:15–31. https://doi.org/10.1177/1094428112452151
GSMA (2019a) The Mobile Economy - Sub-Saharan Africa 2019. GSMA, London. https://www.gsma.com/mobileeconomy/sub-saharan-africa/. Accessed 25 May 2020
GSMA (2019b) The State of Mobile Internet Connectivity Report 2019. GSMA, London. https://www.gsma.com/mobilefordevelopment/resources/the-state-of-mobile-internet-connectivity-report-2019/. Accessed 17 June 2020
Guest G, Bunce A, Johnson L (2006) How many interviews are enough? Field Methods 18:59–82. https://doi.org/10.1177/1525822X05279903
Gutierrez MA, Moreno RA, Rebelo MS (2017) Information and communication technologies and global health challenges. In: de Fátima Marin H, Massad E, Gutierrez MA, Rodrigues RJ, Sigulem D (eds) Global health informatics. Academic Press, Cambridge, MA, USA, pp 50–93
Huang F, Blaschke S, Lucas H (2017) Beyond pilotitis: taking digital health interventions to the national level in China and Uganda. Glob Health 13(1):49. https://doi.org/10.1186/s12992-017-0275-z
Iribarren SJ, Cato K, Falzon L, Stone PW (2017) What is the economic evidence for mHealth? A systematic review of economic evaluations of mHealth solutions. PLoS One 12:e0170581. https://doi.org/10.1371/journal.pone.0170581
Istepanian RS, AlAnzi T (2020) Mobile health (m-health): evidence-based progress or scientific retrogression. In: Feng DD (ed) Biomedical information technology. Academic Press, Cambridge, MA, USA, pp 717–733
Källander K, Tibenderana JK, Akpogheneta OJ, Strachan DL, Hill Z, ten Asbroek AHA, Conteh L, Kirkwood BR, Meek SR (2013) Mobile health (mHealth) approaches and lessons for increased performance and retention of community health workers in low- and middle-income countries: a review. J Med Internet Res 15:e17. https://doi.org/10.2196/jmir.2130
Kostkova P, Brewer H, Lusignan S de, Fottrell E, Goldacre B, Hart G, Koczan P, Knight P, Marsolier C, McKendry RA (2016) Who owns the data? Open data for healthcare. Front Public Health 4. https://doi.org/10.3389/fpubh.2016.00007
Krah EF, de Kruijf JG (2016) Exploring the ambivalent evidence base of mobile health (mHealth): a systematic literature review on the use of mobile phones for the improvement of community health in Africa. Digit Health 2:2055207616679264. https://doi.org/10.1177/2055207616679264
Kruse C, Betancourt J, Ortiz S, Valdes Luna SM, Bamrah IK, Segovia N (2019) Barriers to the use of mobile health in improving health outcomes in developing countries: systematic review. J Med Internet Res 21:e13263. https://doi.org/10.2196/13263
Kuipers P, Humphreys JS, Wakerman J, Wells R, Jones J, Entwistle P (2008) Collaborative review of pilot projects to inform policy: a methodological remedy for pilotitis? Aust New Zealand Health Policy 5. https://doi.org/10.1186/1743-8462-5-17
Kumar K (1989) Conducting key informant interviews in developing countries. Agency for International Development, Washington DC
Labrique AB, Wadhwani C, Williams KA, Lamptey P, Hesp C, Luk R, Aerts A (2018) Best practices in scaling digital health in low and middle income countries. Glob Health 14:103. https://doi.org/10.1186/s12992-018-0424-z
Latif S, Rana R, Qadir J, Ali A, Imran MA, Younis MS (2017) Mobile health in the developing world: review of literature and lessons from a case study. IEEE Access 5:11540–11556. https://doi.org/10.1109/ACCESS.2017.2710800
Lee S, Begley CE, Morgan R, Chan W, Kim S-Y (2018) M-health policy readiness and enabling factors: comparisons of sub-Saharan Africa and Organization for Economic Cooperation and Development countries. Telemed J E Health 24:908–921. https://doi.org/10.1089/tmj.2017.0278
Leon N, Schneider H, Daviaud E (2012) Applying a framework for assessing the health system challenges to scaling up mHealth in South Africa BMC Med Inform Decis Mak 12:123. https://doi.org/10.1186/1472-6947-12-123
Littman-Quinn R, Mibenge C, Antwi C, Chandra A, Kovarik CL (2013) Implementation of m-health applications in Botswana: telemedicine and education on mobile devices in a low resource setting. J Telemed Telecare 19:120–125. https://doi.org/10.1177/1357633x12474746
Madon S, Reinhard N, Roode D, Walsham G (2009) Digital inclusion projects in developing countries: processes of institutionalization. Inf Technol Dev 15:95–107. https://doi.org/10.1002/itdj.20108
Marcolino MS, Oliveira JAQ, D'Agostino M, Ribeiro AL, Alkmim MBM, Novillo-Ortiz D (2018) The impact of mHealth interventions: systematic review of systematic reviews. JMIR Mhealth Uhealth 6:e23. https://doi.org/10.2196/mhealth.8873
Mechael P, Batavia H, Kaonga N, Searle S, Kwan A, Goldberger A, Fu L, Ossman J (2010) Barriers and gaps affecting mHealth in low and middle income countries: policy white paper. Center for Global Health and Economic DevelopmentEarth Institute, Columbia University, New York
Mechael PN (2009) The case for mHealth in developing countries. Innov: Technol Govern Global 4:103–118
Miles MB, Huberman AM, Saldana J (2014) Qualitative data analysis: a methods sourcebook, 3rd Edition. Sage, Thousand Oaks, CA, USA
Moore CG, Carter RE, Nietert PJ, Stewart PW (2011) Recommendations for planning pilot studies in clinical and translational research. Clin Transl Sci 4:332–337. https://doi.org/10.1111/j.1752-8062.2011.00347.x
Mukisa MT, Ochieng DO, Waiganjo PW (2017) Evaluating the sustainability of mHealt h systems in developing countries: the knowledge gap. Int J Sci Res 6:1363–1367. https://doi.org/10.21275/art20175601
Mupela EN, Mustarde P, Jones HLC (2011) Telemedicine in primary health: the virtual doctor project Zambia. Philos Ethics Humanit Med 6:9. https://doi.org/10.1186/1747-5341-6-9
Musango JK, Brent AC (2011) A conceptual framework for energy technology sustainability assessment. Energy Sustain Dev 15:84–91. https://doi.org/10.1016/j.esd.2010.10.005
Nafziger EW (ed) (2012) Economic development, 5th edn. Cambridge University Press, Cambridge, UK
Ndlovu K, Littman-Quinn R, Park E, Dikai Z, Kovarik CL (2014) Scaling up a Mobile telemedicine solution in Botswana: keys to sustainability. Front Public Health 2:275. https://doi.org/10.3389/fpubh.2014.00275
Novillo-Ortiz D (2017) Intergovernmental collaboration in global health informatics. In: de Fátima Marin H, Massad E, Gutierrez MA, Rodrigues RJ, Sigulem D (eds) Global health informatics. Academic Press, Cambridge, MA, USA, pp. 264–287
Olsen IT (1998) Sustainability of health care: a framework for analysis. Health Policy Plan 13:287–295. https://doi.org/10.1093/heapol/13.3.287
Opoku D, Busse R, Quentin W (2019) Achieving sustainability and scale-up of Mobile health noncommunicable disease interventions in sub-Saharan Africa: views of policy makers in Ghana. JMIR Mhealth Uhealth 7:e11497. https://doi.org/10.2196/11497
Palinkas LA, Horwitz SM, Green CA, Wisdom JP, Duan N, Hoagwood K (2015) Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Admin Pol Ment Health 42:533–544. https://doi.org/10.1007/s10488-013-0528-y
Patton MQ (2002) Qualitative research & evaluation methods: integrating theory and practice, 3rd Edition. Sage, Thousand Oaks, CA, USA
Robinson OC (2014) Sampling in interview-based qualitative research: a theoretical and practical guide. Qual Res Psychol 11:25–41. https://doi.org/10.1080/14780887.2013.801543
Saldaña J (2015) The coding manual for qualitative researchers. Sage, Thousand Oaks, CA, USA
Sanner TA, Roland LK, Braa K (2012) From pilot to scale: towards an mHealth typology for low-resource contexts. Health Policy Technol 1:155–164. https://doi.org/10.1016/j.hlpt.2012.07.009
Silva BMC, Rodrigues JJPC, La Torre Díez I de, López-Coronado M, Saleem K (2015) Mobile-health: a review of current state in 2015. J Biomed Inform 56:265–272. https://doi.org/10.1016/j.jbi.2015.06.003
Sondaal SFV, Browne JL, Amoakoh-Coleman M, Borgstein A, Miltenburg AS, Verwijs M, Klipstein-Grobusch K (2016) Assessing the effect of mHealth interventions in improving maternal and neonatal care in low- and middle-income countries: a systematic review. PLoS One 11:e0154664. https://doi.org/10.1371/journal.pone.0154664
Steinhubl SR, Muse ED, Topol EJ (2015) The emerging field of mobile health. Sci Transl Med 7:283rv3. https://doi.org/10.1126/scitranslmed.aaa3487
Sundin P, Callan J, Mehta K (2016) Why do entrepreneurial mHealth ventures in the developing world fail to scale? J Med Eng Technol 40:444–457. https://doi.org/10.1080/03091902.2016.1213901
Tomlinson M, Rotheram-Borus MJ, Swartz L, Tsai AC (2013) Scaling up mHealth: where is the evidence? PLoS Med 10:e1001382. https://doi.org/10.1371/journal.pmed.1001382
United Nations (2018) The Least Developed Country Category: 2018 Country Snapshots. UN DESA, New York. https://www.un.org/development/desa/dpad/wp-content/uploads/sites/45/Snapshots2018.pdf. Accessed 15 April 2020
University of Manchester (2010) Assessing the effectiveness of communication therapy in the North West — the ACT NoW Study. http://research.bmh.manchester.ac.uk/actnow/glossary. Accessed 29 May 2020
Urquhart C, Lehmann H, Myers MD (2010) Putting the ‘theory’ back into grounded theory: guidelines for grounded theory studies in information systems. Inf Syst J 20:357–381. https://doi.org/10.1111/j.1365-2575.2009.00328.x
van Dyk L (2014) A review of telehealth service implementation frameworks. Int J Environ Res Public Health 11:1279–1298. https://doi.org/10.3390/ijerph110201279
van Olmen J, Erwin E, García-Ulloa AC, Meessen B, Miranda JJ, Bobrow K, Iwelunmore J, Nwaozuru U, Obiezu Umeh C, Smith C, Harding C, Kumar P, Gonzales C, Hernández-Jiménez S, Yeates K (2020) Implementation barriers for mHealth for non-communicable diseases management in low and middle income countries: a scoping review and field-based views from implementers. Wellcome Open Res 5:7. https://doi.org/10.12688/wellcomeopenres.15581.2
Vesel L, Hipgrave D, Dowden J, Kariuki W (2015) Application of mHealth to improve service delivery and health outcomes: opportunities and challenges. APS 29:1683–1698. https://doi.org/10.11564/29-1-718
Wallis L, Blessing P, Dalwai M, Shin SD (2017) Integrating mHealth at point of care in low- and middle-income settings: the system perspective. Glob Health Action 10(sup3):1327686. https://doi.org/10.1080/16549716.2017.1327686
Walsham G (2012) Are we making a better world with Icts? Reflections on a future agenda for the IS field. J Inf Technol 27:87–93. https://doi.org/10.1057/jit.2012.4
Walsham G (2020) Health information systems in developing countries: some reflections on information for action. Inf Technol Dev 26:194–200. https://doi.org/10.1080/02681102.2019.1586632
WHO (2004a) Guidelines and instruments for conducting an evaluation of the sustainability of CDTI projects. WHO, Geneva. https://www.who.int/apoc/publications/guidelinesevalsustainabilitycorrectedversionsept04.pdf?ua=1. Accessed 20 August 2020
WHO (2004b) Maternal Mortality - Factsheet. WHO, Geneva. https://apps.who.int/iris/bitstream/handle/10665/112318/WHO_RHR_14.06_eng.pdf?sequence=5. Accessed 31 May 2020
WHO (2017) Tuberculosis (TB): Frequently asked questions on Global Task Force on digital health for TB and its work. WHO, Geneva. https://www.who.int/tb/areas-of-work/digital-health/faq/en/. Accessed 15 April 2020
WHO (2019) Trends in maternal mortality: 2000 to 2017. WHO, Geneva
Wicklund E (2019) UK mHealth pilot program reportedly saves lives, will be expanded. mHealthIntelligence, Danvers, MA, USA. https://mhealthintelligence.com/news/uk-mhealth-pilot-program-reportedly-saves-lives-will-be-expanded? Accessed 4 June 2020
Wilson K, Gertz B, Arenth B, Salisbury N (2014) The journey to scale: Moving together past digital health pilots. PATH, Seattle, WA, USA. https://path.azureedge.net/media/documents/PATH_Journey_to_Scale_R2.pdf. Accessed 4 June 2020
World Bank (2016) UHC in Africa: a framework for action. World Bank, Washington DC. https://openknowledge.worldbank.org/handle/10986/26072. Accessed 18 July 2020
Yin RK (2016) Qualitative research from start to finish, 2nd edn. Guilford Press, New York
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Material preparation, data collection, and analysis were performed by Maike Greve, Nils van Osten and Alfred Benedikt Brendel. Maike Greve and Nils van Osten wrote the first draft of the manuscript. Alfred Benedikt Brendel commented on previous versions of the manuscript. All authors read and approved the final manuscript. The research was supervised by Alfred Benedikt Brendel and Lutz M. Kolbe. The corresponding author is Maike Greve.
Corresponding author
Ethics declarations
Ethical approval
This is an observational study where no ethical approval is required. All participants voluntarily participated and agreed to the data privacy agreement and the declaration of consent.
Consent to participate
Informed consent was obtained from all individual participants included in the study before conducting the interviews.
Consent for publication
Informed consent for publication of the results of the interviews was obtained prior to the interview from all participants.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Greve, M., Brendel, A.B., van Osten, N. et al. Overcoming the barriers of mobile health that hamper sustainability in low-resource environments. J Public Health (Berl.) 30, 49–62 (2022). https://doi.org/10.1007/s10389-021-01536-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10389-021-01536-8