Abstract
Background
Programmed cell death 1 (PD-1)-based treatments are approved for several cancers. CheckMate 648, a global, phase 3 trial, showed that first-line nivolumab (anti-PD-1 antibody) plus ipilimumab (NIVO + IPI) or nivolumab plus chemotherapy (NIVO + Chemo) significantly increased survival in advanced esophageal squamous cell carcinoma (ESCC) without new safety signals versus chemotherapy alone (Chemo).
Methods
We evaluated the Japanese subpopulation of CheckMate 648 (n = 394/970), randomized to receive first-line NIVO + IPI, NIVO + Chemo, or Chemo. Efficacy endpoints included overall survival (OS) and progression-free survival assessed by blinded independent central review in Japanese patients with tumor-cell programmed death-ligand 1 (PD-L1) expression ≥ 1% and in all randomized Japanese patients.
Results
In the Japanese population, 131, 126, and 137 patients were treated with NIVO + IPI, NIVO + Chemo, and Chemo, and 66, 62, and 65 patients had tumor-cell PD-L1 ≥ 1%, respectively. In patients with tumor-cell PD-L1 ≥ 1%, median OS was numerically longer with NIVO + IPI (20.2 months; hazard ratio [95% CI], 0.46 [0.30–0.71]) and NIVO + Chemo (17.3 months; 0.53 [0.35–0.82]) versus Chemo (9.0 months). In all randomized patients, median OS was numerically longer with NIVO + IPI (17.6 months; 0.68 [0.51–0.92]) and NIVO + Chemo (15.5 months; 0.73 [0.54–0.99]) versus Chemo (11.0 months). Grade 3–4 treatment-related adverse events were reported in 37%, 49%, and 36% of all patients in the NIVO + IPI, NIVO + Chemo, and Chemo arms, respectively.
Conclusion
Survival benefits with acceptable tolerability observed for NIVO + IPI and NIVO + Chemo treatments strongly support their use as a new standard first-line treatment in Japanese patients with advanced ESCC.
ClinicalTrials.gov ID
NCT03143153.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Esophageal squamous cell carcinoma (ESCC) is the dominant (~ 85%) histological subtype of esophageal cancer globally [1]. In 2018, the age-standardized incidence rate of ESCC per 100,000 person-years was 5 times higher in Japan than in America [1]. ESCC has a poor prognosis, with a 5-year relative survival rate of ~ 40% in 2016, and 1-year relative survival rate of 45% in patients treated with first-line 5-fluorouracil + cisplatin therapy in Japan [2, 3], highlighting the need for more effective treatment options. Until recently, the first-line treatment for advanced ESCC was limited to fluoropyrimidine + platinum-based chemotherapy in Japan [4]. In 2021–2022, the survival benefit of five different first-line treatments with anti-programmed cell death 1 [PD-1] antibodies-plus-chemotherapy over chemotherapy alone was verified by five phase 3 trials, namely KEYNOTE-590 (pembrolizumab) [5], CheckMate 648/ONO-4538-50 (nivolumab) [6], ESCORT-1st (camrelizumab) [7], JUPITER-06 (toripalimab) [8], and ORIENT-15 (sintilimab) [9]. Pembrolizumab + chemotherapy received approval in various countries and has become the standard first-line treatment for ESCC [10]. Based on KEYNOTE-590 results, which included Japanese patients, pembrolizumab + chemotherapy was recommended as the first-line treatment regimen in the Japanese esophageal cancer guidelines [5, 11, 12]. In the global, phase 3, CheckMate 648 study, nivolumab administered along with ipilimumab (anti-cytotoxic T lymphocyte-associated protein 4 antibody [anti-CTLA4 antibody]) or chemotherapy resulted in significantly longer overall survival (OS) versus chemotherapy alone in advanced ESCC [6]. No new safety signals were identified for nivolumab combination therapies [6].
A few phase 3 studies provide evidence for advanced ESCC treatments in the Japanese subgroup. Japanese subpopulation data from phase 3 trials for advanced esophageal cancer are limited to KEYNOTE-181 and ATTRACTION-3 trials that assessed second-line pembrolizumab or nivolumab monotherapy, respectively [13, 14]. Survival outcomes of ESCC were different for Japanese population compared with global clinical trial populations, as seen in ATTRACTION-3, where median OS for nivolumab was numerically longer in the Japanese subpopulation (13.4 months) versus the global intent-to-treat population (10.9 months) [14, 15]. Subsequent anticancer treatment rates were also different between the Japanese and global intent-to-treat population in ATTRACTION-3, suggesting that treatment practices including approval/reimbursement systems may differ between Japan and other countries [3, 14,15,16]. Therefore, analyzing the efficacy and safety data specific to the Japanese subpopulation from the global phase 3 trials for first-line treatment in patients with advanced ESCC is important. Thus, we evaluated the efficacy and safety of nivolumab combination therapies in the Japanese subpopulation of CheckMate 648, and compared these findings with the global population.
Methods
Study design and patients
CheckMate 648 is an open-label, phase 3 trial to assess nivolumab-plus-ipilimumab (NIVO + IPI) and nivolumab-plus-chemotherapy (NIVO + Chemo) combinations compared with chemotherapy alone (Chemo) as a first-line treatment in patients with advanced ESCC. Detailed methods are published elsewhere [6]. Briefly, patients aged ≥ 18 years who had advanced (unresectable, recurrent, or metastatic), histologically confirmed ESCC or adenosquamous cell carcinoma (predominant squamous differentiation) and measurable disease per Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1 were enrolled, irrespective of their PD-L1 expression status. Patients had no prior systemic therapy for advanced disease and were not amenable to cancer-directed curative therapies. Patients were stratified according to tumor-cell PD-L1 expression (PD-L1: ≥ 1% vs. < 1%, or indeterminate), region (East Asia [Japan, Korea, Taiwan] vs. rest of Asia vs. rest of the world), Eastern Cooperative Oncology Group performance status (ECOG PS) (0 vs. 1), and number of organs with metastases (≤ 1 vs. ≥ 2). Eligible patients were randomized (1:1:1) to receive nivolumab (3 mg/kg every 2 weeks) plus ipilimumab (1 mg/kg every 6 weeks), nivolumab (240 mg every 2 weeks) plus chemotherapy (4-week cycle of fluorouracil 800 mg/m2 on days 1–5 and cisplatin 80 mg/m2 on day 1), or chemotherapy alone (same dose as described above). Treatment continued until disease progression, unacceptable toxicity, consent withdrawal, or end of trial. Nivolumab or NIVO + IPI was administered for up to 2 years in the absence of disease progression or unacceptable toxicity. The current analyses focus on the Japanese racial subpopulation enrolled at Japanese sites, with data cutoff identical to that for the global trial population (January 18, 2021).
Pre-specified outcomes
The primary endpoints were OS and progression-free survival (PFS) assessed by blinded independent central review (BICR) per RECIST version 1.1 in patients with tumor-cell PD-L1 expression ≥ 1%. Secondary endpoints comprised OS and PFS (BICR) in all randomized patients, and objective response rate (ORR) per BICR in patients with tumor-cell PD-L1 expression ≥ 1% and all randomized patients. Key exploratory endpoints included investigator-assessed PFS, subgroup analyses for OS based on demographics and clinical factors for all patients, duration of response (BICR), and safety. Efficacy endpoints were assessed for the global intent-to-treat population. Adverse events (AEs) were assessed in all the patients who had received ≥ 1 dose of the assigned treatment, and were graded according to the National Cancer Institute Common Terminology Criteria for Adverse Events, v4.0.
Statistical analyses
Descriptive analyses were conducted for the Japanese subpopulation. Hazard ratios (HRs) for OS and PFS were calculated using unstratified Cox proportional hazards model with treatment as the sole covariate. Two-sided 95% confidence intervals (CIs) for the HR were provided. Median OS, PFS, and duration of response for each treatment arms were estimated using the Kaplan–Meier method, and the corresponding 95% CIs were constructed based on a log–log transformed CI for the survivor function. OS and PFS rates at fixed time points were derived from the Kaplan–Meier estimate. The 95% CIs for proportions were calculated using the Clopper–Pearson method. Statistical analyses were performed using SAS software v9.2 to v9.4 (SAS Institute, Cary, USA) and R statistical software package.
Results
Characteristics of the Japanese subpopulation
Overall, 394 of 970 patients from CheckMate 648 trial were enrolled in Japan (NIVO + IPI, n = 131; NIVO + Chemo, n = 126; Chemo, n = 137). Baseline patient characteristics were generally balanced between the treatment arms (Table 1). Of the 394 patients, 386 (98%) received ≥ 1 dose of the study drug (NIVO + IPI, n = 130; NIVO + Chemo, n = 121; Chemo, n = 135). Among the treated patients, the primary reason for treatment discontinuation was disease progression (NIVO + IPI: 55% [71/130]; NIVO + Chemo: 65% [79/121]; Chemo: 69% [93/135]; Online Resource 1). Subsequent therapies were administered to 73% (96/131), 67% (85/126), and 82% (112/137) of the patients in the NIVO + IPI, NIVO + Chemo, and Chemo arms, respectively, with 9.2% (12/131), 9.5% (12/126), and 26.3% (36/137) of the patients receiving subsequent therapy comprising immune checkpoint inhibitors (anti-PD-1 or anti-CTLA4 antibody), respectively (Online Resource 2).
Efficacy in the Japanese subpopulation
Analyses of the NIVO + IPI versus Chemo arm
OS was numerically longer for the NIVO + IPI versus the Chemo arm in patients with tumor-cell PD-L1 ≥ 1% and in all randomized patients. In patients with tumor-cell PD-L1 ≥ 1%, NIVO + IPI had an OS benefit: the median OS increased by 11.2 months versus Chemo (20.2 vs. 9.0 months [refer to the figures for 95% CIs; hereinafter the same]), reducing the risk of death by 54% (HR 0.46 [0.30–0.71]) (Fig. 1a). The corresponding 12-month OS rate doubled for the NIVO + IPI (70%) versus the Chemo (36%) arm. In all randomized patients, NIVO + IPI had numerically longer median OS versus Chemo (17.6 months vs. 11.0 months; HR 0.68 [0.51–0.92]); the 12-month OS rate was 63% versus 47%, respectively (Fig. 1b). In patients with tumor-cell PD-L1 < 1%, median OS was comparable between NIVO + IPI and Chemo (14.5 vs. 14.2 months; HR 1.01 [0.66–1.54]) (Online Resource 3). Median PFS (BICR) in patients with tumor-cell PD-L1 ≥ 1% was numerically longer in the NIVO + IPI versus the Chemo arm (5.4 vs. 4.2 months); however, the risk of progression or death was comparable between the arms (HR 0.84 [0.54–1.32]) (Fig. 1c). In all randomized patients, median PFS (BICR) was comparable between NIVO + IPI versus Chemo arm (4.2 vs. 4.3 months; HR 1.16 [0.85–1.57]) (Fig. 1d). In patients with tumor-cell PD-L1 < 1%, median PFS was 3.2 months in NIVO + IPI versus 5.6 months in Chemo (HR 1.51 [95% CI 0.99–2.31]) (Online Resource 3). The HR trends for PFS per investigator assessment and BICR were similar; per investigator assessment, NIVO + IPI showed PFS benefit versus Chemo in patients with tumor-cell PD-L1 ≥ 1% (5.4 vs. 3.0 months; HR 0.57 [0.38–0.87]) and was comparable with Chemo in all randomized patients (4.1 vs. 4.2 months; HR 0.84 [0.64–1.11]) (Online Resource 4). ORR per BICR was higher, with the complete response rate ~ 4 times higher for NIVO + IPI versus Chemo in patients with tumor-cell PD-L1 ≥ 1% and in all randomized patients (Table 2). Objective (complete or partial) responses were also more durable for NIVO + IPI versus Chemo in patients with tumor-cell PD-L1 ≥ 1% and in all randomized patients (Fig. 1e and f).
Overall survival, progression-free survival per BICR, and duration of response per BICR with NIVO + IPI versus Chemo in patients with tumor-cell PD-L1 ≥ 1% (left panel: a, c, e) and all randomized patients (right panel: b, d, f) in the Japanese subpopulation. BICR blinded independent central review, Chemo chemotherapy, DOR duration of response, HR hazard ratio, IPI ipilimumab, NIVO nivolumab, OS overall survival, PFS progression-free survival, PD-L1 programmed death-ligand 1. Note: Kaplan–Meier estimates are shown, and HRs were calculated using unstratified Cox proportional hazard regression model. DOR was calculated for patients whose best overall response was complete or partial
Analyses of the NIVO + Chemo versus Chemo arm
In patients with tumor-cell PD-L1 ≥ 1%, NIVO + Chemo numerically increased the median OS versus Chemo (17.3 vs. 9.0 months) and reduced the risk of death by 47% (HR 0.53 [0.35–0.82]); the 12-month OS rate was 64% versus 36%, respectively (Fig. 2a). In all randomized patients, NIVO + Chemo extended the median OS by 4.5 months versus Chemo (15.5 vs. 11.0 months), reducing the risk of death by 27% (HR 0.73 [0.54–0.99]); the 12-month OS rate also increased (61% vs. 47%, respectively) (Fig. 2b). In patients with tumor-cell PD-L1 < 1%, median OS was comparable between NIVO + Chemo and Chemo (14.4 vs. 14.2 months; HR 0.99 [0.65–1.51]) (Online Resource 3). PFS benefit (BICR) was observed in patients with tumor-cell PD-L1 ≥ 1% with NIVO + Chemo versus Chemo (median PFS, 7.0 vs. 4.2 months; HR 0.56 [0.36–0.89]) (Fig. 2c). Though the median PFS was numerically higher in the NIVO + Chemo versus the Chemo arm in all randomized patients (6.8 vs. 4.3 months), the risk of progression or death was not different between the two arms (HR 0.76 [0.56–1.03]) (Fig. 2d). In patients with tumor-cell PD-L1 < 1%, median PFS (BICR) was comparable between NIVO + Chemo and Chemo (5.8 vs. 5.6 months; HR 0.96 [0.63–1.47]) (Online Resource 3). By investigator assessment, NIVO + Chemo showed PFS benefit versus Chemo in patients with tumor-cell PD-L1 ≥ 1% (8.0 vs. 3.0 months; HR, 0.36 [0.23–0.56]) and in all randomized patients (6.8 vs. 4.2 months; HR 0.58 [0.44–0.76]) (Online Resource 4). ORR per BICR was higher in the NIVO + Chemo arm than in the Chemo arm, with the complete response rate increasing > 5 times for patients with tumor-cell PD-L1 ≥ 1% and > 4 times for all randomized patients (Table 2). The duration of response was also longer in the NIVO + Chemo arm than in the Chemo arm for both, tumor-cell PD-L1 ≥ 1% cases and all randomized patients (Fig. 2e and f).
Overall survival, progression-free survival per BICR, and duration of response per BICR with NIVO + Chemo versus Chemo in patients with tumor-cell PD-L1 ≥ 1% (left panel: a, c, e) and all randomized patients (right panel: b, d, f) in the Japanese subpopulation. BICR blinded independent central review, Chemo chemotherapy, DOR duration of response, HR hazard ratio, NIVO nivolumab, OS overall survival, PFS progression-free survival, PD-L1 programmed death-ligand 1. Note: Kaplan–Meier estimates are shown, and HRs were calculated using unstratified Cox proportional hazard regression model. DOR was calculated for patients whose best overall response was complete or partial
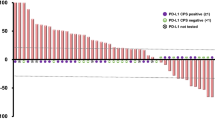
Subgroup analyses of OS in all randomized Japanese patients
Subgroup analyses were performed for age, sex, ECOG PS, tumor-cell PD-L1 expression status, disease status at study entry, number of organs with metastases, and smoking history using unstratified Cox proportional hazards modeling with treatment as the only covariate (Online Resource 5). OS numerically favored NIVO + IPI or NIVO + Chemo versus Chemo alone across multiple prespecified subgroups in all randomized patients. In both, NIVO + IPI and NIVO + Chemo arms, the OS prolongation effect was numerically larger with the higher tumor-cell PD-L1 expression subgroup, with no further enrichment of efficacy observed in any of the cutoff values higher than 1% (Online Resource 5).
Exposure and safety in all-treated Japanese patients
The median treatment duration was longer with NIVO + Chemo (5.6 months), while the values were similar for NIVO + IPI (2.7 months) and Chemo (2.9 months) (Online Resource 6). Among the treated patients, 48 (37%), 59 (49%), and 49 (36%) patients reported grade 3–4 treatment-related AEs (TRAEs) in the NIVO + IPI, NIVO + Chemo, and Chemo arms, respectively; correspondingly, serious TRAEs of any grade occurred in 55 (42%), 25 (21%), and 16 (12%) patients (Table 3). TRAEs led to treatment discontinuation in 32 (25%), 44 (36%), and 32 (24%) patients in the NIVO + IPI, NIVO + Chemo, and Chemo arms, respectively (Table 3). TRAEs led to death in 1 (1%), 2 (2%), and 0 patients in the NIVO + IPI, NIVO + Chemo, and Chemo arms, respectively (Table 3). Most TRAEs with potential immunologic etiology were grade 1–2; grade 3–4 events occurred in ≤ 10% of the patients across organ categories (Online Resource 7).
Discussion
First-line NIVO + IPI and NIVO + Chemo treatments resulted in a substantial survival advantage over Chemo in Japanese patients with advanced ESCC. The efficacy and safety of NIVO + IPI and NIVO + Chemo were consistent between the CheckMate 648 Japanese subpopulation and the global population (including Japan) [6]. For NIVO + IPI and NIVO + Chemo, the median OS and median PFS (BICR) were numerically longer, with higher ORR for the Japanese subpopulation versus the global population. Specifically, in the chemotherapy-free combination (NIVO + IPI), the Japanese subpopulation had numerically longer median OS than the global population (17.6 [12.7–22.8] vs. 12.7 [11.3–15.5] months) [6]. Baseline patient characteristics of the Japanese subpopulation and the global population were generally similar. However, more patients in the Japanese subpopulation had an ECOG PS of 0 in the NIVO + IPI (71% vs. 46%), NIVO + Chemo (71% vs. 47%), and Chemo (69% vs. 48%) arms versus the global population [6]. It is plausible that a better functional status may have contributed to the survival benefit in the Japanese subpopulation compared with the global population. This hypothesis is supported by findings of NIVO + IPI phase 3 trials for non-small cell lung cancer (NSCLC) suggesting that better performance status was correlated with greater NIVO + IPI efficacy [17, 18].
Patients with better clinical condition are generally more likely to receive subsequent treatment. This may explain the higher rates of subsequent anticancer therapies in the current study across all arms in the Japanese subpopulation (63%–75%) versus the global population (51–63%), especially the rate of subsequent systemic anticancer therapies received [6]. Differences in ECOG PS scores and subsequent treatment rates may have affected the OS benefit observed. These findings are concordant with a phase 3 nivolumab monotherapy versus chemotherapy trial (ATTRACTION-3) in advanced ESCC [14, 15]. In ATTRACTION-3, compared with the global population, the Japanese subpopulation had higher rates of ECOG PS 0 (nivolumab, 61% vs. 48%; Chemo, 64% vs. 51%), subsequent systemic anticancer therapies (nivolumab, 59% vs. 53%; Chemo, 47% vs. 47%), and longer median OS (nivolumab, 13.4 vs. 10.9 months; Chemo, 9.4 vs. 8.4 months) [14, 15]. Subsequent chemotherapy after anti-PD-1/PD-L1 therapy improved efficacy outcomes in other types of cancers [19,20,21], which may have contributed to the higher efficacy of the nivolumab combination treatments in the Japanese subpopulation in this study.
Also, the Japanese subpopulation had a relatively higher percentage of smokers than the global population (89% vs. 80%) [6]. The subgroup analyses of CheckMate 648 global population suggested a longer OS in smokers versus nonsmokers in the NIVO + IPI arm [6]. In contrast, nonsmokers tended to have longer OS in the NIVO + Chemo arm, possibly because the concomitant chemotherapy may override any advantage of nivolumab in smokers. Reportedly, immune checkpoint inhibitors are more effective in patients with a smoking history in NSCLC and several other cancers [22, 23]. These results suggest that the difference in the proportion of smokers may have enhanced the efficacy of NIVO + IPI in the Japanese population.
The HRs for death for NIVO + IPI or NIVO + Chemo versus Chemo were < 1, suggesting overall survival advantage irrespective of increasing tumor-cell PD-L1 cutoff values (≥ 1%, ≥ 5%, ≥ 10%; HRs 0.46, 0.45, 0.50 for NIVO + IPI and 0.54, 0.51, 0.54 for NIVO + Chemo, respectively). In contrast, HRs for death in NIVO + IPI or NIVO + Chemo arms versus Chemo were close to 1 for tumor-cell PD-L1 < 1% (HR 1.01 for NIVO + IPI and 0.99 for NIVO + Chemo, respectively). The relatively smaller efficacy of NIVO + IPI or NIVO + Chemo at tumor-cell PD-L1 < 1% suggests that tumor-cell PD-L1 expression might be one of the predictors of response; however, the magnitude of efficacy did not increase in patients with higher tumor-cell PD-L1 expression levels (≥ 1%, ≥ 5%, ≥ 10%). Therefore, there seems to be a limitation to performing response prediction with only PD-L1.
In the four anti-PD-1 phase 3 studies, namely, KEYNOTE-590 (pembrolizumab), ESCORT-1st, (camrelizumab), JUPITER-06 (toripalimab), and ORIENT-15 (sintilimab), the anti-PD-1 antibody + chemotherapy combination significantly prolonged median OS compared with placebo + chemotherapy [5, 7,8,9]. Similar findings were noted for the NIVO + Chemo arm in both the Japanese (current study) and global population of the CheckMate 648 trial [6].
In the NIVO + IPI arm, the incidence of serious TRAEs was higher than that in the NIVO + Chemo and Chemo arms, whereas the incidence of any TRAEs was lower. Similar trends were observed in the global population [6]. However, in the NIVO + IPI arm, TRAEs with potential immunologic etiology of endocrine, pulmonary, and skin were slightly more common in the Japanese than in the global population [6]. This concurs with reports on renal cell carcinoma or NSCLC treated with NIVO + IPI, where rates of these AE categories were similarly higher in the Japanese or Asian population than in the global population [24,25,26].
The NIVO + IPI and NIVO + Chemo arms were not compared statistically as this study was not designed to compare these 2 arms. It was also not possible to speculate advantage of one or the other nivolumab combination treatment for specific study subgroups. In clinical practice, the choice of cancer treatment regimen is governed by several considerations including disease status, patients’ requirements and preferences, and capacity to tolerate specific immunotherapy or chemotherapy. Future studies and exploratory post hoc analyses are warranted to determine prognostic predictors for each of the nivolumab combination regimen.
Conclusion
NIVO + IPI and NIVO + Chemo in the Japanese subpopulation showed efficacy benefits compared with Chemo and had an acceptable safety profile, similar to reports from the global population. This Japanese sub-analysis showed that both NIVO + IPI and NIVO + Chemo treatments can become a new standard first-line treatment option for Japanese patients with advanced ESCC.
References
Arnold M, Ferlay J, van Berge Henegouwen MI, Soerjomataram I. Global burden of oesophageal and gastric cancer by histology and subsite in 2018. Gut. 2020;69(9):1564–71. https://doi.org/10.1136/gutjnl-2020-321600.
Center for Cancer Control and Information Services. Monitoring of cancer incidence in Japan—Survival 2009–2011 report. 2020. https://ganjoho.jp/en/professional/statistics/table_download.html. Accessed 8 Feb 2022.
Hiramoto S, Kato K, Shoji H, et al. A retrospective analysis of 5-fluorouracil plus cisplatin as first-line chemotherapy in the recent treatment strategy for patients with metastatic or recurrent esophageal squamous cell carcinoma. Int J Clin Oncol. 2018;23:466–72. https://doi.org/10.1007/s10147-018-1239-x.
Kitagawa Y, Uno T, Oyama T, et al. Esophageal cancer practice guidelines 2017 edited by the Japan Esophageal Society: part 1. Esophagus. 2019;16(1):1–24. https://doi.org/10.1007/s10388-018-0641-9.
Sun J-M, Shen L, Shah MA, et al. Pembrolizumab plus chemotherapy versus chemotherapy alone for first-line treatment of advanced oesophageal cancer (KEYNOTE-590): a randomised, placebo-controlled, phase 3 study. Lancet. 2021;398(10302):759–71. https://doi.org/10.1016/S0140-6736(21)01234-4.
Doki Y, Ajani JA, Kato K, et al. Nivolumab combination therapy in advanced esophageal squamous-cell carcinoma. N Engl J Med. 2022;386(5):449–62. https://doi.org/10.1056/NEJMoa2111380.
Luo H, Lu J, Bai Y, et al. Effect of camrelizumab vs placebo added to chemotherapy on survival and progression-free survival in patients with advanced or metastatic esophageal squamous cell carcinoma: the ESCORT-1st randomized clinical trial. JAMA. 2021;326(10):916–25. https://doi.org/10.1001/JAMA.2021.12836.
Wang Z-X, Cui C, Yao J, et al. Toripalimab plus chemotherapy in treatment-naïve, advanced esophageal squamous cell carcinoma (JUPITER-06): a multi-center phase 3 trial. Cancer Cell. 2022. https://doi.org/10.1016/j.ccell.2022.02.007.
Shen L, Lu Z-H, Wang J-Y, et al. LBA52 Sintilimab plus chemotherapy versus chemotherapy as first-line therapy in patients with advanced or metastatic esophageal squamous cell cancer: first results of the phase III ORIENT-15 study. Ann Oncol. 2021;32:S1330. https://doi.org/10.1016/j.annonc.2021.08.2132.
MERCK. Merck’s KEYTRUDA® (pembrolizumab) Approved in Japan in combination with chemotherapy for first-line treatment of patients with radically unresectable, advanced or recurrent esophageal carcinoma. 2021. https://www.merck.com/news/mercks-keytruda-pembrolizumab-approved-in-japan-in-combination-with-chemotherapy-for-first-line-treatment-of-patients-with-radically-unresectable-advanced-or-recurrent-esophageal-car/. Accessed 8 Feb 2022.
Pharmaceuticals and Medical Devices Agency, Japan. List of Approved Products—New Drugs, FY 2021. 2022. https://www.pmda.go.jp/english/review-services/reviews/approved-information/drugs/0002.html. Accessed 5 Mar 2022.
The Japanese Esophageal Society. KEYNOTE-590 study outline and comments from the Japan Esophageal Society Guidelines Committee on pembrolizumab in the treatment of advanced esophageal cancer. 2021. https://www.esophagus.jp/files/guideline_20211130_02.pdf. Accessed 8 Feb 2022.
Muro K, Kojima T, Moriwaki T, et al. Second-line pembrolizumab versus chemotherapy in Japanese patients with advanced esophageal cancer: subgroup analysis from KEYNOTE-181. Esophagus. 2022;19:137–45. https://doi.org/10.1007/s10388-021-00877-3.
Takahashi M, Kato K, Okada M, et al. Nivolumab versus chemotherapy in Japanese patients with advanced esophageal squamous cell carcinoma: a subgroup analysis of a multicenter, randomized, open-label, phase 3 trial (ATTRACTION-3). Esophagus. 2021;18(1):90. https://doi.org/10.1007/S10388-020-00794-X.
Kato K, Cho BC, Takahashi M, et al. Nivolumab versus chemotherapy in patients with advanced oesophageal squamous cell carcinoma refractory or intolerant to previous chemotherapy (ATTRACTION-3): a multicentre, randomised, open-label, phase 3 trial. Lancet Oncol. 2019;20(11):1506–17. https://doi.org/10.1016/S1470-2045(19)30626-6.
Muro K, Lordick F, Tsushima T, et al. Pan-Asian adapted ESMO Clinical Practice Guidelines for the management of patients with metastatic oesophageal cancer: a JSMO–ESMO initiative endorsed by CSCO, KSMO, MOS. SSO and TOS Ann Oncol. 2019;30:34–43. https://doi.org/10.1093/annonc/mdy498.
Hellmann MD, Paz-Ares L, Bernabe Caro R, et al. Nivolumab plus ipilimumab in advanced non-small-cell lung cancer. N Engl J Med. 2019;381(21):2020–31. https://doi.org/10.1056/NEJMoa1910231.
Barlesi F, Audigier-Valette C, Felip E, et al. Nivolumab plus low-dose IPILIMUMAB as first-line treatment of advanced NSCLC: overall survival analysis of checkmate 817. Ann Oncol. 2019;30:xi33–4. https://doi.org/10.1093/ANNONC/MDZ451.001.
Kato K, Narita Y, Mitani S, et al. Efficacy of cytotoxic agents after progression on anti-PD-(L)1 antibody for pre-treated metastatic gastric cancer. Anticancer Res. 2020;40(4):2247–55. https://doi.org/10.21873/ANTICANRES.14187.
Sasaki A, Kawazoe A, Eto T, et al. Improved efficacy of taxanes and ramucirumab combination chemotherapy after exposure to anti-PD-1 therapy in advanced gastric cancer. ESMO Open. 2020. https://doi.org/10.1136/ESMOOPEN-2020-000775.
Park SE, Lee SH, Ahn JS, Ahn MJ, Park K, Sun JM. Increased response rates to salvage chemotherapy administered after PD-1/PD-L1 inhibitors in patients with non-small cell lung cancer. J Thorac Oncol. 2018;13(1):106–11. https://doi.org/10.1016/J.JTHO.2017.10.011.
Mo J, Hu X, Gu L, et al. Smokers or non-smokers: who benefits more from immune checkpoint inhibitors in treatment of malignancies? An up-to-date meta-analysis. World J Surg Oncol. 2020;18(1):15. https://doi.org/10.1186/s12957-020-1792-4.
Kim J, Ha H, Park J, Cho J, Lim JH, Lee MH. Association of smoking status with efficacy of first-line immune checkpoint inhibitors in advanced non-small cell lung cancers: a systematic review and meta-analysis. J Cancer. 2022;13(2):364–72. https://doi.org/10.7150/jca.65374.
Motzer RJ, Rini BI, McDermott DF, et al. Nivolumab plus ipilimumab versus sunitinib in first-line treatment for advanced renal cell carcinoma: extended follow-up of efficacy and safety results from a randomised, controlled, phase 3 trial. Lancet Oncol. 2019;20(10):1370–85. https://doi.org/10.1016/S1470-2045(19)30413-9.
Tomita Y, Kondo T, Kimura G, et al. Nivolumab plus ipilimumab versus sunitinib in previously untreated advanced renal-cell carcinoma: analysis of Japanese patients in CheckMate 214 with extended follow-up. Jpn J Clin Oncol. 2020;50(1):12. https://doi.org/10.1093/JJCO/HYZ132.
Nishio M, O'Byrne KJ et al. First-line nivolumab (NIVO)+ ipilimumab (IPI) in advanced NSCLC: CheckMate 227 Asian subanalysis. The 61st Annual Meeting of the Japan Lung Cancer Society. PS-03
Acknowledgements
We thank all the study participants and their families, investigators, and study teams. Medical writing support was provided by MedPro Clinical Research, and was funded by Ono Pharmaceutical Co., Ltd. and Bristol Myers Squibb. The authors also thank Minal Jaggar, PhD, Vidula Bhole, MD, MHSc, and Ivan D’Souza, MS, of MedPro Clinical Research for providing medical writing support for this manuscript.
Funding
This study was supported by Ono Pharmaceutical Co., Ltd., Japan, and Bristol Myers Squibb, USA.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Statement
All procedures followed in this study were in accordance with the Declaration of Helsinki and Good Clinical Practice guidelines, and were approved by the institutional review board at each study site. All patients provided their informed consent for being included in this study.
Conflict of interest
Ken Kato has received research grants from AstraZeneca, Bayer, BeiGene, Bristol Myers Squibb, Chugai Pharmaceutical Co., Ltd., Merck & Co., Oncolys BioPharma Inc., Ono Pharmaceutical Co., Ltd., Shionogi & Co., Ltd., and Taiho Pharmaceuticals Co., Ltd.; received honoraria and consulting fees from Bristol Myers Squibb, Chugai Pharmaceutical Co., Ltd., Merck & Co., Ono Pharmaceutical Co., Ltd., and Taiho Pharmaceuticals Co., Ltd.; and received consulting fees from AstraZeneca, Bayer, and BeiGene. Yuichiro Doki has received research grants and speaker engagement fees from Abbott, Ajinomoto Pharmaceuticals, Astellas Pharma Inc., AstraZeneca, Chugai Pharmaceutical Co., Ltd., Daiichi-Sankyo Co., Ltd.; Eisai Co., Ltd., Eli Lilly & Co., Johnson & Johnson Health Care Systems Inc., Kaken Pharmaceutical Co., Ltd., Ono Pharmaceutical Co., Ltd., Shionogi & Co., Ltd., Taiho Pharmaceuticals Co., Ltd., Takeda Pharmaceutical Co., Ltd., and Yakult Honsha Co. Ltd.; received research grants from CSL Behring, Nestle HealthCare Nutrition Inc., Nippon Kayaku, Novartis Pharma, and Pfizer; and received speaker engagements fees from Asahi Kasei Pharma Corporation, Intuitive Surgical, Medtronic, Merck & Co., Olympus Corporation, Otsuka Pharmaceutical Co., Ltd., Sanofi, and Teijin Pharma Ltd. Takashi Ogata has received honoraria for lectures from Bristol Myers Squibb and Ono Pharmaceutical Co., Ltd. Satoru Motoyama has received institutional research grants from Kaken Pharmaceutical Co., Ltd., Ono Pharmaceutical Co., Ltd., Otsuka Pharmaceutical Co., Ltd., Otsuka Pharmaceutical Factory Inc., Shionogi & Co., Ltd., Taiho Pharmaceuticals Co., Ltd., and Takeda Pharmaceutical Co., Ltd.; received advisory board fees and honoraria from Bristol Myers Squibb, Chugai Pharmaceutical Co., Ltd., Merck & Co., and Ono Pharmaceutical Co., Ltd.; and honoraria from Kaken Pharmaceutical Co., Ltd., Otsuka Pharmaceutical Co., Ltd., and Otsuka Pharmaceutical Factory Inc. Hisato Kawakami has received institutional research grants from Chugai Pharmaceutical Co., Ltd., Eisai Co., Ltd., Kobayashi Pharmaceutical. Co., Ltd., and Taiho Pharmaceuticals Co., Ltd.; consulting fees from Daiichi-Sankyo Co., Ltd.; and honoraria from Bayer, Bristol Myers Squibb, Chugai Pharmaceutical Co., Ltd., Daiichi-Sankyo Co., Ltd., Eli Lilly & Co., GlaxoSmithKline, Merck & Co., Ono Pharmaceutical Co., Ltd., Otsuka Pharmaceutical Co., Ltd., Taiho Pharmaceuticals Co., Ltd., Takeda Pharmaceutical Co., Ltd., Teijin Pharma Ltd., and Yakult Honsha Co. Ltd. Takashi Kojima has received institutional research grants from Amgen Inc., BeiGene, Chugai Pharmaceutical Co., Ltd., EPS Corporation, Merck & Co., Parexel International, Shionogi & Co., Ltd., and Taiho Pharmaceuticals Co., Ltd.; received honoraria from Bristol Myers Squibb, Covidien Japan, Inc., Merck & Co., Oncolys BioPharma Inc, Ono Pharmaceutical Co., Ltd., and Taiho Pharmaceuticals Co., Ltd.; and participated on data safety monitoring or advisory board of Astellas Pharma Inc., Bristol Myers Squibb, Merck & Co., and Oncolys BioPharma Inc. Morihito Okada has received institutional research grants and honoraria from AstraZeneca, Bristol Myers Squibb, Chugai Pharmaceutical Co., Ltd., Covidien Japan, Inc., Daiichi-Sankyo Co., Ltd., Johnson & Johnson, Kyorin Pharmaceutical Co., Ltd., Merck & Co., and Pfizer Inc.; and research grants from Clinipace, Eli Lilly & Co., Kissei Pharmaceutical Co., Ltd., Kyouwa Hakkou Kirin Co., Ltd., Mitsubishi Tanabe Pharma, Nihon Medi-Physics Co., Ltd., Ono Pharmaceutical Co., Ltd., Parexel International, and Taiho Pharmaceuticals Co., Ltd. Ryu Ishihara received honoraria from AstraZeneca, Daiichi-Sankyo Co., Ltd., EA Pharma Co., Ltd., Fujifilm, Olympus Corporation, and Ono Pharmaceutical Co., Ltd. Carlos Amaya Chanaga is an employee of Bristol Myers Squibb and has stocks of AbbVie and Bristol Myers Squibb. Tien Chen is an employee of Bristol Myers Squibb, and has stocks and a patent issued by Bristol Myers Squibb. Yasuhiro Matsumura is an employee and holds stocks of Ono Pharmaceutical Company Ltd. Yuko Kitagawa has received institutional research grants from Asahi Kasei Pharma Corporation, Chugai Pharmaceutical Co., Ltd., Dainippon Sumitomo Pharma Co., Ltd., EA Pharma Co., Ltd., Eisai Co., Ltd., Kaken Pharmaceutical Co., Ltd., Kyouwa Hakkou Kirin Co., Ltd., Medicon Inc., Merck & Co., Nihon Pharmaceuticals Co. Ltd., Nippon Covidien Inc., Ono Pharmaceutical Co., Ltd., Otsuka Pharmaceutical Co., Ltd., Otsuka Pharmaceutical Factory Inc., Taiho Pharmaceuticals Co., Ltd., Takeda Pharmaceutical Co., Ltd., Teijin Pharma Ltd., Tsumura & Co., and Yakult Honsha Co. Ltd.; and received honoraria from Asahi Kasei Pharma Corporation, Aska Pharmaceutical Co., Ltd., AstraZeneca, Bristol Myers Squibb, Chugai Pharmaceutical Co., Ltd., Ethicon Inc., Kaken Pharmaceutical Co., Ltd., Merck & Co., Nippon Covidien Inc., Olympus Corporation, Ono Pharmaceutical Co., Ltd., Otsuka Pharmaceutical Co., Ltd., Shionogi & Co., Ltd., Smith & Nephew KK, and Taiho Pharmaceuticals Co., Ltd. Masaki Ueno, Yutaro Kubota, and Yasuhiro Shirakawa have nothing to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kato, K., Doki, Y., Ogata, T. et al. First-line nivolumab plus ipilimumab or chemotherapy versus chemotherapy alone in advanced esophageal squamous cell carcinoma: a Japanese subgroup analysis of open-label, phase 3 trial (CheckMate 648/ONO-4538-50). Esophagus 20, 291–301 (2023). https://doi.org/10.1007/s10388-022-00970-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10388-022-00970-1