Abstract
Background
Jackhammer esophagus (JE) is a hypercontractile esophageal motility disorder diagnosed using high-resolution manometry (HRM). We sought to determine the clinical presentation and therapeutic data of patients with JE in Japan.
Methods
The study included patients with JE, diagnosed through HRM performed for suspicious esophageal motility disorders. Demographics, esophagogastroduodenoscopy, radiology, and therapy data were collected from patient charts.
Results
Among the 4,412 HRM tests performed, 89 patients (61.6 ± 13.4 years; 64 males, 25 females) were diagnosed with JE (2.0%). Dysphagia was the most frequent symptom (80%), followed by chest pain (40%) and heartburn (25%). Esophagogastroduodenoscopy showed abnormal findings in 32% of patients: corkscrew/rosary beads appearance in 26%, narrowing in 11%. Eosinophilic infiltration (> 15 eosinophils/high power field) was diagnosed in 21%. Esophagography showed abnormal findings in 9% of the patients. For the initial therapy, 47 patients received medical treatment followed by peroral endoscopic myotomy (21 patients) and laparoscopic myotomy (two patients). Thirteen patients did not receive any treatment and 10 of those (77%) reported spontaneous resolution of symptoms. Patients who required invasive treatment experienced severe disability in their quality of life and greater maximal distal contractile integral than those who did not.
Conclusions
HRM showed that the prevalence of JE was very low (2%). Esophagogastroduodenoscopy revealed some characteristic features of JE in patients. Some patients showed improvement of symptoms without invasive treatments. Follow-up with/without medical treatment should be considered before performing invasive treatment in patients whose distal contractile integral is relatively low and the quality of life is not impaired.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Jackhammer esophagus (JE) is a hypercontractile esophageal motility disorder diagnosed using high-resolution manometry (HRM). This disorder is defined by the Chicago Classification as a strong contraction, at least two swallows with a distal contractile integral (DCI) > 8,000 mm Hg.s.cm during HRM using the ManoScan system (ManoScan™, Medtronic, Minneapolis, MN, USA).(HRM). [1,2,3]. The prevalence of JE is very low, and a standard treatment has not been established thus far [1, 4]. Although the pathogenesis of JE remains unclear, cases of eosinophilic infiltration of the esophageal mucosa [4, 5] and eosinophilic myositis have been reported [6, 7]. However, the frequency and etiological significance of eosinophilic infiltration have not been clarified. The low incidence of this disorder renders the accumulation of cases at a single institution difficult. Thus, we conducted this multicenter study to determine the frequency of JE in Japan. The aim of this study was to determine the clinical presentation, findings using esophagogastroduodenoscopy (EGD), radiology, and manometry, and therapy performed in patients with JE in a multicenter retrospective cohort.
Methods
Study design and patients
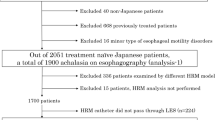
This was a retrospective observational study conducted by the Jackhammer Esophagus Study Group formed by the Japan Esophageal Society. The study involved the review of consecutive HRM studies performed in 16 hospitals in Japan from January 2008 to June 2017. Usual indications for HRM were the detection of esophageal motility disorder in patients with or without symptoms or preoperative analysis of patients with hiatus hernia or gastroesophageal reflux surgery. Patients diagnosed with JE were included in the study. JE was defined based on a DCI cutoff value ≥ 20% of wet swallow according to the Chicago Classification version 3.0 [3]. The cutoff value of DCI was determined according to the HRM systems used: 8,000 mmHg‧s‧cm with the ManoScan system and InSIGHT system (InSIGHT Ultima®, Diversatek, Milwaukee, WI, USA) [8] and DCI > 10,000 mmHg‧s‧cm with the Starlet system (Starlet®, Star Medical, Inc., Tokyo, Japan) [9, 10]. Patients with a history of esophageal surgery were excluded. This study was approved by the research ethics committee of the Japan Esophageal Society and the ethics committee of each participating institution in the study group.
Fundamental data obtained from each hospital
The total number of patients who underwent HRM during the study period and that of patients with JE were reported from each hospital to calculate the frequency. In addition, the type of HRM equipment was reported.
Clinical data of patients with JE
Clinical data, manometric, endoscopic, and radiographic findings, and treatment data were collected. Patient charts were reviewed to collect clinical, examination, and therapeutic data. Clinical variables included age, sex, symptoms, and comorbidities. Quality of life (QOL) was rated as no interference with daily life, mild disability, and severe disability (which rendered patients unable to work).
Endoscopic and radiographic findings
Endoscopic data were reviewed to detect the findings of erosive or eosinophilic esophagitis, and potential findings of esophageal dysmotility (e.g., corkscrew/rosary beads appearance or narrowing). Among the patients who underwent esophageal mucosal biopsy, the detection of > 15 eosinophils/high power field was indicative of eosinophilic infiltration. Radiographic data (i.e., esophagograms) were analyzed to determine the presence of corkscrew/rosary beads appearance in patients. Esophageal wall thickening was assessed by either endoscopic ultrasound or thoracic computer tomography. A total thickness of the esophagus wall > 5 mm indicated wall thickening [11].
HRM
HRM studies were performed using three types of solid-state HRM systems, i.e., ManoScan system, Starlet system, and InSIGHT system. The catheter was introduced nasally into the esophagus and positioned to record pressures from the hypopharynx to the stomach. The recording was performed with the patient in a supine position; notably, for patients who had difficulty in swallowing, an incline of ≤ 30 degrees was acceptable. HRM was usually performed with a calibration and baseline period without deglutition. Subsequently, ten water swallows (5 mL) were performed with an interval of ≥ 30 s between swallows.
For the calculation of the DCI, only pressures > 20 mmHg were used by the software of each HRM system, i.e., the ManoView™ ESO Analysis Software (Medtronic, Minneapolis, MN, USA, Starlet analysis software (Starmedical, Tokyo, Japan), and BioView Software (Diversatek, Milwaukee, WI, USA). Normal DCI values varied according to the HRM systems, and the cutoff values were extracted from the references. As stated above, we selected 8000 mmHg‧s‧cm for ManoScan [3] and InSIGHT [8], and 10,000 mmHg‧s‧cm for Starlet [10]. Similarly, normal integrated relaxation pressure (IRP) values differed between systems. Concomitant esophagogastric junction (EGJ) outflow obstruction was diagnosed if the median IRP value was higher than the upper limit of each system (i.e., 15 mmHg with ManoScan, 20 mmHg for InSIGHT [8], and 26 mmHg with Starlet [9]). The Chicago Classification separates elevated IRP as EGJ outflow obstruction from JE. However, in cohort studies conducted to date, elevated IRP has also been considered a subtype of JE (i.e., JE with elevated IRP) [12, 13].
Treatment and clinical outcomes
Information on the treatment and follow-up was also collected. The treatment selection was based on the preference of each treating physician. The treatment efficacy was evaluated by reviewing the patients’ charts using a four-point scale ranging from 1 (complete response) to 4 (no response). Complete response was defined as total disappearance of symptoms. Sufficient/insufficient efficacy was defined as persistence of symptoms, but with sufficient/insufficient improvement. No efficacy was defined as lack of improvement of symptoms after treatment.
Data and statistical analysis
Statistical analyses were performed using the SPSS version 25.0 (IBM Corp., Armonk, NY, USA) software. Frequency data (sex and symptoms) are expressed as percentages. Continuous data with normal distribution (age and HRM parameters) are expressed as the mean ± standard deviation. Non-normally distributed data are shown as the median with lower and upper quartiles. Student’s t test was used for the comparison of parametric data. Continuous parameters were analyzed using analysis of variance, and the Kruskal–Wallis test was utilized as a non-parametric test. Categorical variables were analyzed using Fisher’s exact test. The statistical significance level for all analyses was set at p ≤ 0.05.
Results
Esophageal manometric findings obtained using each of the three solid-state HRM systems
Based on the 4412 HRM tests performed, 89 patients were diagnosed with JE (2.0%). HRM findings are shown in Table 1. Of the 89 patients with JE, 29, 40, and 20 were diagnosed by ManoScan, Starlet, and InSIGHT, respectively. Mean DCI values for these groups were 8,120.9 mmHg‧s‧cm, 12,041.6 mmHg‧s‧cm, and 7267 mmHg‧s‧cm, respectively. Twenty-one patients (24%) had high IRP over the upper normal limit. Although direct comparison of absolute values was not possible, because each device yields different normal values, there were no significant differences between the devices in the rate of elevated IRP or number of swallows with DCI higher than the normal limit.
Patient characteristics
Patient characteristics are shown in Table 2. The mean age was 61.6 ± 13.4 years; 64 males (72%) and 25 females (28%). Dysphagia was the most frequent symptom (80%), followed by chest pain (40%) and heartburn (25%).
Endoscopic and radiographic features of JE
EGD was performed in 87 patients (98%); abnormal findings were detected in 32% of the patients: corkscrew/rosary beads appearance in 26% and narrowing in 11% (Table 3). Eosinophilic esophagitis-like findings were observed in seven patients (8%), linear furrows in three patients, rings in one patient, and white exudates in five patients. Biopsies were performed in 58 patients (67%), and esophageal eosinophilia (> 15 eosinophils/high power field) was diagnosed in 12 patients (21%).
Esophagography was performed in 71 patients (80%), and abnormal findings were found in 35 of those patients (49%): corkscrew/rosary beads appearance in 25 patients (34%) and narrowing in 15 patients (21%). Esophageal wall thickening, examined by endoscopic ultrasound or chest computed tomography, was observed in 40 patients (55%).
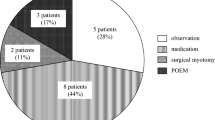
Treatment and clinical course
Initial treatment is shown in Table 4. Six patients were lost to follow-up and were excluded from the analysis. Forty-seven patients received medical treatment as initial therapy, and sufficient efficacy was recorded in 30 of those (64%). The drugs used in these patients ranged considerably from proton pump inhibitors to antiallergic agents (Table 5). Twenty-one patients (25%) underwent per-oral endoscopic myotomy (POEM), and sufficient efficacy was recorded in 16 of those (76%). Two patients (2%) underwent laparoscopic myotomy; 13 patients (16%) did not receive any treatment and 10 of those (77%) experienced spontaneous improvement of their symptoms.
Sub-analysis of the group that required invasive treatment
Patients who required invasive treatment, namely POEM or laparoscopic myotomy, were compared with others (Table 6). The rate of requirement of invasive treatment was significantly higher in patients with severe disability in QOL who had difficulty in continuing to work versus others (37% versus 15%, respectively, p 0.026). Comparison of HRM parameters obtained from each device showed that the maximal DCI was significantly higher in patients who required invasive treatment and underwent HRM with the Starlet and InSIGHT systems.
Discussion
This was the first multicenter cohort study on JE conducted in Asia. We found that the prevalence of JE in patients undergoing HRM examination in Japan was 2.0%. This is similar to the prevalence (1.7–4.0%) reported in cohort studies from western countries [12,13,14]. Furthermore, it is almost identical to that reported in a recent meta-analysis [15].
Regarding sex dominance, 72% of the patients analyzed in the present study were males. Numerous previous studies showed that JE was more frequent among females; however, the largest study on JE conducted thus far (227 patients) included mostly males [12]. Hence, our results are not surprising.
The present analysis included endoscopic data for almost all cases. Thirty patients (38%) had findings suggestive of some form of abnormal tonic contraction. The findings of dysmotility observed on barium were also observed on endoscopy. HRM is the gold standard diagnostic test for esophageal motility disorder. However, HRM is still only performed in specialized facilities. Patients with dysphagia or non-cardiac chest pain typically visit general hospitals and undergo EGD. One-third of patients with JE had an abnormal contraction which could be detected by EGD; this would be a good reason for referral to HRM examination. However, since two-thirds of the patients did not have abnormalities detected through endoscopy, it is recommended that patients with long-lasting symptoms undergo HRM.
A notable finding of this study was that a high percentage of patients with JE had eosinophilic infiltration in esophageal mucosa. It has been reported that eosinophilic esophagitis causes a variety of esophageal motility disorders, ranging from aperistalsis to strong contractions and achalasia-like dysmotility [16, 17]. Roman et al. reported eosinophilic infiltration into the esophageal mucosa in three of 41 patients (7%) with JE [1]. Philonenko et al. reported eosinophilic infiltration into the esophageal mucosa in three of 63 (4.7%) patients with JE who underwent esophageal biopsy [12]. Furthermore, there is an increasing number of case reports of JE accompanied by eosinophilic esophagitis [5, 18] and eosinophilic myositis [6, 7]. In many of these cases, eosinophilic myositis is detected by muscle layer biopsy during POEM [6, 7, 19]. Furthermore, from the therapeutic perspective, treatment with steroids has been successfully utilized in these patients [18, 20]. In the present study, we found eosinophilic infiltration (i.e., > 15 eosinophils/high power field) in 12 of the 58 patients (21%) with JE who underwent esophageal mucosal biopsies. Since the frequency of eosinophilic esophagitis among those undergoing examination with EGD in Japan is < 1% [21, 22] eosinophil infiltration in patients with JE appears to be more common. Of the 12 cases with proven eosinophil infiltration, 9 were treated with steroid therapy (5 systemic and 4 local), and 5 of those (56%) had satisfactory improvement of symptoms.
Although a standard treatment for JE has not been established, POEM is increasingly being used. According to a meta-analysis, 82% of patients treated with POEM showed improvement in symptoms [15]. In this study, 76% of patients who underwent POEM as initial treatment reported satisfactory symptom improvement. Nevertheless, 77% of patients who did not receive treatment also experienced improvement in symptoms during the follow-up. In terms of QOL among these 13 patients, 12 patients had mild disability or no interference and one patient experienced severe disability.
The selection of treatment for patients with JE appears to be a challenging task, as some of them in the present study improved without receiving medical treatment. Based on the characteristics of patients who required invasive treatment, POEM and myotomy were necessary in those with severe disability in terms of QOL as well as higher maximal DCI, who underwent HRM examination with the Starlet and InSIGHT systems. It has been reported that high DCI is an indicator for the requirement of POEM in JE [23]. Notably, there was no difference in the highest DCI among patients examined with the ManoScan system. Although the reason for this observation is unclear, it may be attributed to the low number of cases which required invasive treatment among those examined with this system, as well as inconsistent treatment selection across hospitals. Only six (21%) of those tested with the ManoScan system received invasive treatment versus 15 (38%) and six (30%) of those tested with the Starrett system and InSIGHT system, respectively. The present data showed that patients with mild symptoms and mild elevation in DCI may not require invasive therapy during the follow-up period. Therefore, our results indicate that POEM is not applicable to all cases of JE; medical observation, including follow-up, is an option for patients with mild impairment of QOL.
This study revealed that the types of medical treatment administered varied. Steroids and antiallergic drugs can be used to treat eosinophilic involvement, while other agents can be utilized to reduce smooth muscle contractility. Calcium blockers were the most commonly used pharmacological agents, and their efficacy was good in approximately 60% of patients in this study. It has been proposed that the pathogenesis of JE is based on an imbalance between inhibitory and excitatory innervation. Some studies reported that JE may develop due to possible injury to the vagus nerve during lung transplantation and radiofrequency catheter ablation for atrial fibrillation [24, 25]. A physiological study also demonstrated that cholinergic nerve excitation is associated with strong contractions, providing evidence that anticholinergic agents may be effective in the treatment of JE [26].
Shakuyakukanzo-to, a Japanese herbal medicine, is widely used for the treatment of muscle cramps in Japan. Some case reports have also shown its effectiveness in JE [23, 27]. It has been demonstrated that shakuyakukanzo-to exerts an antispasmodic effect on smooth muscle and inhibits peristalsis of the digestive tract in animals [28]. Moreover, in humans, it inhibits gastrointestinal motility when sprayed directly into the intestinal tract during endoscopy [29]. Therefore, this agent may be a new treatment option for JE.
This study had several limitations. Firstly, there was no uniform treatment strategy, and the selection of treatment depended on each treating physician. Since this was a retrospective study, it was difficult to objectively evaluate subjective data (e.g., symptoms and treatment efficacy). Moreover, we could not evaluate the effect of each drug, because several drugs were used simultaneously in combination. Prospective studies are warranted to determine the most appropriate treatment strategies. Second, this study examined three different HRM devices. We could not compare the parameters of HRM obtained for all patients together, as the values of the measured parameters depend on the type of device used.
In conclusion, the present data demonstrate that the prevalence of JE in Japan is almost identical to that reported in western countries. Patients showed some characteristic features of JE during examination with EGD. Many patients showed improvement in their symptoms without undergoing invasive treatments, such as POEM. We suggest that follow-up with or without the administration of medical treatment should be considered prior to performing invasive treatment in patients with a relatively low DCI and not severe impairment in QOL. Further prospective study is warranted to determine the most appropriate treatment strategy.
References
Roman S, Pandolfino JE, Chen J, Boris L, Luger D, Kahrilas PJ. Phenotypes and clinical context of hypercontractility in high-resolution esophageal pressure topography (EPT). Am J Gastroenterol. 2012;107(1):37–45.
Hébert PC, Wells G, Blajchman MA, Marshall J, Martin C, Pagliarello G, et al. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care transfusion requirements in critical care. Investigators, canadian critical care trials group. N Engl J Med. 1999;340(6):409–17.
Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S, Smout AJ, et al. The Chicago classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015;27(2):160–74.
Roman S, Kahrilas PJ. Management of spastic disorders of the esophagus. Gastroenterol Clin North Am. 2013;42(1):27–43.
Tanaka S, Toyonaga T, Kawara F, Watanabe D, Hoshi N, Abe H, et al. A case of Jackhammer esophagus caused by eosinophilic esophagitis in which per-oral endoscopic myotomy resulted in symptom improvement. Clin J Gastroenterol. 2018;11(5):377–81.
Sato H, Takeuchi M, Takahashi K. Eosinophilic infiltration of the muscularis propria in a patient with jackhammer esophagus treated with per-oral endoscopic myotomy. Clin Gastroenterol Hepatol. 2015;13(4):e33–4.
Tang Y, Xiong W, Yu T, Wang M, Zhang G, Lin L. Eosinophilic esophageal myositis a plausible cause of histological changes of primary jackhammer esophagus: a case report. Am J Gastroenterol. 2018;113(1):150–2.
do Carmo GC, Jafari J, Sifrim D, de Oliveira RB. Normal esophageal pressure topography metrics for data derived from the Sandhill-Unisensor high-resolution manometry assembly in supine and sitting positions. Neurogastroenterol Motil. 2015;27(2):285–92.
Kuribayashi S, Iwakiri K, Kawada A, Kawami N, Hoshino S, Takenouchi N, et al. Variant parameter values-as defined by the Chicago criteria-produced by ManoScan and a new system with unisensor catheter. Neurogastroenterol Motil. 2015;27(2):188–94.
Kuribayashi S, Iwakiri K, Shinozaki T, Hosaka H, Kawada A, Kawami N, et al. Clinical impact of different cut-off values in high-resolution manometry systems on diagnosing esophageal motility disorders. J Gastroenterol. 2019;54(12):1078–82.
Desai RK, Tagliabue JR, Wegryn SA, Einstein DM. CT evaluation of wall thickening in the alimentary tract. Radiographics. 1991;11(5):771–83.
Philonenko S, Roman S, Zerbib F, Gourcerol G, Gault N, Ropert A, et al. Jackhammer esophagus: Clinical presentation, manometric diagnosis, and therapeutic results-Results from a multicenter French cohort. Neurogastroenterol Motil. 2020;32(11): e13918.
Herregods TV, Smout AJ, Ooi JL, Sifrim D, Bredenoord AJ. Jackhammer esophagus: observations on a european cohort. Neurogastroenterol Motil. 2017. https://doi.org/10.1111/nmo.12975.
Clement M, Zhu WJ, Neshkova E, Bouin M. Jackhammer esophagus: from manometric diagnosis to clinical presentation. Can J Gastroenterol Hepatol. 2019;2019:5036160.
Wahba G, Bouin M. Jackhammer esophagus: A meta-analysis of patient demographics, disease presentation, high-resolution manometry data, and treatment outcomes. Neurogastroenterol Motil. 2020;32(11): e13870.
Roman S, Hirano I, Kwiatek MA, Gonsalves N, Chen J, Kahrilas PJ, et al. Manometric features of eosinophilic esophagitis in esophageal pressure topography. Neurogastroenterol Motil. 2011;23(3):208–14, e111.
Martin Martin L, Santander C, Lopez Martin MC, Espinoza-Rios J, Chavarria-Herbozo C, Gisbert JP, et al. Esophageal motor abnormalities in eosinophilic esophagitis identified by high-resolution manometry. J Gastroenterol Hepatol. 2011;26(9):1447–50.
Melchior C, Chiavelli H, Leroi AM, Ducrotté P, Gourcerol G. Recovery of a “Jackhammer esophagus” after the treatment of an eosinophilic esophagitis. Am J Gastroenterol. 2012;107(6):952–4.
Nakajima N, Sato H, Takahashi K, Hasegawa G, Mizuno K, Hashimoto S, et al. Muscle layer histopathology and manometry pattern of primary esophageal motility disorders including achalasia. Neurogastroenterol Motil. 2017. https://doi.org/10.1111/nmo.12968.
Funaki Y, Ogasawara N, Kawamura Y, Yoshimine T, Tamura Y, Izawa S, et al. Markedly effective steroid treatment of three patients with allergy-related jackhammer esophagus. Intern Med. 2020;59(5):633–9.
Sato H, Honma T, Nozawa Y, Owaki T, Imai M, Sano T, et al. Eosinophilic esophagitis in Japanese patients: A mild and slow-progressing disorder. PLoS One. 2018;13(11): e0206621.
Fujishiro H, Amano Y, Kushiyama Y, Ishihara S, Kinoshita Y. Eosinophilic esophagitis investigated by upper gastrointestinal endoscopy in Japanese patients. J Gastroenterol. 2011;46(9):1142–4.
Kawami N, Hoshino S, Hoshikawa Y, Takenouchi N, Hanada Y, Tanabe T, et al. Differences in clinical characteristics between conservative-treatment-response group and refractory (surgical-treatment) group in patients with jackhammer esophagus. Esophagus. 2021;18(1):138–43.
Tolone S, Savarino E, Docimo L. Radiofrequency catheter ablation for atrial fibrillation elicited “Jackhammer Esophagus”: a new complication due to vagal nerve stimulation? J Neurogastroenterol Motil. 2015;21(4):612–5.
Khan MQ, Nizami IY, Khan BJ, Al-Ashgar HI. Lung transplantation triggered “jackhammer esophagus”: a case report and review of literature. J Neurogastroenterol Motil. 2013;19(3):390–4.
Babaei A, Shad S, Massey BT. Esophageal hypercontractility is abolished by cholinergic blockade. Neurogastroenterol Motil. 2020;33(8): e14017.
Nakato R, Manabe N, Mitsuoka N, Shiwaku H, Matsumoto H, Yamashita K, et al. Clinical experience with four cases of jackhammer esophagus. Esophagus. 2015;13(2):208–14.
Maeda T, Shinozuka K, Baba K, Hayashi M, Hayashi E. Effect of shakuyaku-kanzoh-toh, a prescription composed of shakuyaku (Paeoniae Radix) and kanzoh (Glycyrrhizae Radix) on guinea pig ileum. J Pharmacobiodyn. 1983;6(3):153–60.
Sakai Y, Tsuyuguchi T, Ishihara T, Kato K, Tsuboi M, Ooka Y, et al. Confirmation of the antispasmodic effect of shakuyaku-kanzo-to (TJ-68), a Chinese herbal medicine, on the duodenal wall by direct spraying during endoscopic retrograde cholangiopancreatography. J Nat Med. 2009;63(2):200–3.
Acknowledgements
We thank all the investigators from the participating hospitals for their cooperation: our study group; Hirofumi Abe and Shinwa Tanaka, Department of Gastroenterology, Kobe University Hospital; Tatsuya Kaneko, Department of Gastroenterology, Graduate School of Medicine, Chiba University; Fumio Tanaka, Department of Gastroenterology, Osaka City University Graduate School of Medicine; Eikichi Ihara and Yoshitaka Hata, Department of Medicine and Bioregulatory Science, Graduate School of Medical Sciences, Kyushu University; Rie Kure, Department of Gastroenterological Endoscopy, Tokyo Women’s Medical University; Takahiro Masuda, Department of Surgery, The Jikei University School of Medicine; Kazumi Inokuchi, Division of Gastroenterology and Hepatology, Department of Internal Medicine, Keio University School of Medicine; Mariko Hamada, Department of gastroenterology, National Center for Global Health and Medicine, Eiko Okimoto, Second Department of Internal Medicine, Shimane University Faculty of Medicine; Hironobu Mikami, Mikami Clinic; and Toshiro Iizuka and Daisuke Kikuchi, Toranomon Hospital.
Funding
This study was supported by the Diversity Promotion Center Joint Research Promotion Project.
Author information
Authors and Affiliations
Contributions
HH was responsible for the conception and design of the study, data acquisition and interpretation, drafting of the manuscript, and statistical analysis. NK, NM, and SK were responsible for study design, data acquisition, analysis, and interpretation, and revision of the manuscript. HS, YF, MA, KH, ST, TM, YF, MW, MK, FY, TM, NI, JA, and YO were responsible for data acquisition from each hospital. TU was responsible for the drafting and revision of the manuscript, and supervision of the study. KI was responsible for organizing the study team, conception and design of the study, and revision of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no financial conflicts of interest to disclose concerning this study.
Ethical statement
All procedures were performed in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national), as well as the tenets of the 1964 Declaration of Helsinki and its later versions. This retrospective study used the opt-out consent method concerning patient participation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hosaka, H., Kawami, N., Manabe, N. et al. Clinical presentation and therapeutic outcome of patients with jackhammer esophagus—a multicenter cohort study in Japan. Esophagus 19, 393–400 (2022). https://doi.org/10.1007/s10388-022-00916-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10388-022-00916-7