Abstract
Background
The updated Chicago Classification version 4.0 (CCv4.0) establishes a more stringent criteria to diagnose ineffective esophageal motility (IEM). This study aims to investigate the clinical significance of IEM in CCv4.0 in the context of gastroesophageal reflux disease (GERD).
Methods
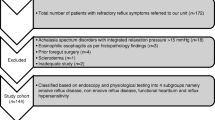
A retrospective study was conducted among suspected GERD patients who had heartburn and/or regurgitation as their chief complaints and completed esophageal function tests in our center from 2017 to 2019. Patients were further grouped as “CCv3.0 IEM” and normal motility according to Chicago Classification version 3.0 (CCv3.0), and as “CCv4.0 IEM” and normal motility according to CCv4.0. The clinical characteristics, high-resolution manometry, esophageal reflux monitoring, and proton pump inhibitor (PPI) efficacy were compared between different groups. Multivariate analyses were performed to identify esophageal motility parameters associated with reflux burden and symptom outcome.
Results
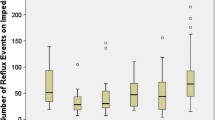
Of 172 subjects included, 93 patients were identified as CCv3.0 IEM, 69 as CCv4.0 IEM. IEM in either version was concomitant with elevated acid burden and impaired esophageal clearance as compared to normal motility in corresponding diagnostic criteria, while the only presence of IEM in CCv4.0 was predictive to abnormal acid exposure (AET > 6%: OR = 2.66, 95% CI [1.27–5.56], p < 0.01). The presence of “CCv3.0 IEM” and low EGJ-CI (EGJ-CI < 39.1 mmHg·cm) had no added value in predicting increased reflux burden. No interaction effect was found between the presence of IEM and a weakened EGJ. None of the manometric variables was capable of predicting PPI response.
Conclusions
Stringent criteria of IEM in CCv4.0 can better predict abnormal acid exposure as compared to CCv3.0.

Similar content being viewed by others
References
Tutuian R, Castell DO. Combined multichannel intraluminal impedance and manometry clarifies esophageal function abnormalities: study in 350 patients. Am J Gastroenterol. 2004;99(6):1011–9.
Boland K, Abdul-Hussein M, Tutuian R, et al. Characteristics of consecutive esophageal motility diagnoses after a decade of change. J Clin Gastroenterol. 2016;50(4):301–6.
Savarino E, Bredenoord AJ, Fox M, et al. Expert consensus document: advances in the physiological assessment and diagnosis of GERD. Nat Rev Gastroenterol Hepatol. 2017;14(11):665–76.
Liu L, Li S, Zhu K, et al. Relationship between esophageal motility and severity of gastroesophageal reflux disease according to the Los Angeles classification. Medicine (Baltimore). 2019;98(19):e15543.
Savarino E, Gemignani L, Pohl D, et al. Oesophageal motility and bolus transit abnormalities increase in parallel with the severity of gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2011;34(4):476–86.
Bazin C, Benezech A, Alessandrini M, et al. Esophageal motor disorders are a strong and independant associated factor of Barrett’s esophagus. J Neurogastroenterol Motil. 2018;24(2):216–25.
Rogers BD, Rengarajan A, Mauro A, et al. Fragmented and failed swallows on esophageal high-resolution manometry associate with abnormal reflux burden better than weak swallows. Neurogastroenterol Motil. 2019;32(2):e13736.
Rengarajan A, Bolkhir A, Gor P, et al. Esophagogastric junction and esophageal body contraction metrics on high-resolution manometry predict esophageal acid burden. Neurogastroenterol Motil. 2018;30(5):e13267.
Jain A, Baker JR, Chen JW. In ineffective esophageal motility, failed swallows are more functionally relevant than weak swallows. Neurogastroenterol Motil. 2018;30(6):e13297.
Dao HV, Matsumura T, Kaneko T, et al. Impact of ineffective esophageal motility on chemical clearance in patients with gastroesophageal reflux symptoms. Dis Esophagus. 2020;33(9):doaa026.
Reddy CA, Baker JR, Lau J, et al. High-resolution manometry diagnosis of ineffective esophageal motility is associated with higher reflux burden. Dig Dis Sci. 2019;64(8):2199–205.
Kahrilas PJ, Bredenoord AJ, Fox M, et al. The Chicago classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015;27(2):160–74.
Yadlapati R, Kahrilas PJ, Fox MR, et al. Esophageal motility disorders on high-resolution manometry: Chicago classification version 40((c)). Neurogastroenterol Motil. 2021;33(1):e14058.
Rogers BD, Rengarajan A, Abrahao L, et al. Esophagogastric junction morphology and contractile integral on high-resolution manometry in asymptomatic healthy volunteers: an international multicenter study. Neurogastroenterol Motil. 2020;33:e14009.
Gor P, Li Y, Munigala S, et al. Interrogation of esophagogastric junction barrier function using the esophagogastric junction contractile integral: an observational cohort study. Dis Esophagus. 2016;29(7):820–8.
Gyawali C, Kahrilas P, Savarino E, et al. Modern diagnosis of GERD: the Lyon Consensus. Gut. 2018;67(7):1351–62.
Andersson T, Alfredsson L, Kallberg H, et al. Calculating measures of biological interaction. Eur J Epidemiol. 2005;20(7):575–9.
Rogers BD, Rengarajan A, Ribolsi M, et al. Postreflux swallow-induced peristaltic wave index from pH-impedance monitoring associates with esophageal body motility and esophageal acid burden. Neurogastroenterol Motil. 2021;33(2):13973.
Wang D, Wang X, Yu Y, et al. Assessment of esophageal motor disorders using high-resolution manometry in esophageal dysphagia with normal endoscopy. J Neurogastroenterol Motil. 2019;25(1):61–7.
Liu Z, Liao J, Tian D, et al. Assessment of esophageal high-resolution impedance manometry in patients with nonobstructive dysphagia. Gastroenterol Res Pract. 2018;2018:6272515.
Simren M, Silny J, Holloway R, et al. Relevance of ineffective oesophageal motility during oesophageal acid clearance. Gut. 2003;52(6):784–90.
Rengarajan A, Gyawali CP. High-resolution manometry can characterize esophagogastric junction morphology and predict esophageal reflux burden. J Clin Gastroenterol. 2020;54(1):22–7.
van Hoeij FB, Smout AJ, Bredenoord AJ. Predictive value of routine esophageal high-resolution manometry for gastro-esophageal reflux disease. Neurogastroenterol Motil. 2015;27(7):963–70.
Tolone S, De Bortoli N, Marabotto E, et al. Esophagogastric junction contractility for clinical assessment in patients with GERD: a real added value? Neurogastroenterol Motil. 2015;27(10):1423–31.
Masuda T, Mittal SK, Kovacs B, et al. Simple manometric index for comprehensive esophagogastric junction barrier competency against gastroesophageal reflux. J Am Coll Surg. 2020;230(5):744–55.
Chen CL, Yi CH, Liu TT, et al. Effects of mosapride on secondary peristalsis in patients with ineffective esophageal motility. Scand J Gastroenterol. 2013;48(12):1363–70.
Lei WY, Hung JS, Liu TT, et al. Influence of prucalopride on esophageal secondary peristalsis in reflux patients with ineffective motility. J Gastroenterol Hepatol. 2018;33(3):650–5.
Sifrim D, Roman S, Savarino E, et al. Normal values and regional differences in oesophageal impedance-pH metrics: a consensus analysis of impedance-pH studies from around the world. Gut. 2020;70:1441.
Acknowledgements
The study was supported by grants from the National Natural Science Foundation of China (81970479) and Medical Scientific Research Foundation of Guangdong Province of China (A2019510). Specific thanks to Bin Li, medical statistician from Clinical Trials Unit, First Affiliated Hospital of Sun Yat-sen University, for providing professional statistical suggestions to this work.
Author information
Authors and Affiliations
Contributions
QJZ and NDT: study concept and design; acquisition of data; analysis and interpretation of data; drafting and finalizing the manuscript. MYZ, SFC, and YL: acquisition of data; analysis and interpretation of data, reviewing and editing the manuscript. YLX: study concept and design; finalizing the manuscript and guarantee of the study.
Corresponding author
Ethics declarations
Ethical Statement
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions.
Conflict of interest
All authors declared no conflict of interest.
Informed consent
Informed consent or substitute for it was obtained from all patients for being included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhuang, Qj., Tan, Nd., Zhang, My. et al. Ineffective esophageal motility in Chicago Classification version 4.0 better predicts abnormal acid exposure. Esophagus 19, 197–203 (2022). https://doi.org/10.1007/s10388-021-00867-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10388-021-00867-5