Abstract
Introduction
Ineffective esophageal motility (IEM) is the most commonly diagnosed abnormality on high-resolution manometry (HRM). However, the clinical significance of IEM and associated reflux burden remains unclear.
Aim
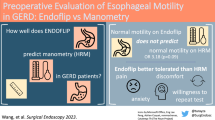
Our primary aim was to compare reflux patterns between IEM versus normal motility on HRM.
Methods
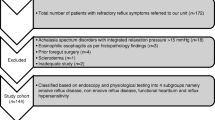
HRM and reflux studies in patients with IEM and normal motility were retrospectively reviewed. Esophageal pressure topography parameters, reflux variables, and patient-reported outcome questionnaires were explored.
Results
A total of 239 patients with IEM were explored. Of these, 146 underwent reflux monitoring. Additionally, 100 patients with normal HRM all of whom had undergone reflux monitoring were included. IEM patients were more likely to have an abnormal number of reflux events compared to normal (22.7% vs. 9.0%, p < 0.01). Including only off-proton pump inhibitor (PPI) testing, IEM patients had higher mean total acid exposure time (AET) and total reflux events compared to normal motility (p = 0.02). Within IEM patients, higher AET modestly correlated with increased percentage of impaired swallows. Increased reflux events modestly correlated with higher impaired swallows and decreased lower esophageal sphincter (LES) resting pressure. Reflux burden increased with higher esophagogastric junction (EGJ) subtype, driven mostly by subtype III, although there was no difference in the distribution of EGJ subtypes between the IEM and normal HRM cohorts.
Conclusions
Patients with HRM diagnosis of IEM may be more prone to acid reflux while off-PPI and non-acid reflux while on-PPI. Reflux burden appears to be worse in IEM patients who have lower resting LES pressure, higher EGJ subtype, or higher percentage of impaired swallows.


Similar content being viewed by others
Abbreviations
- AET:
-
Acid exposure time
- BMI:
-
Body Mass Index
- CLT:
-
Conventional line tracing
- CD:
-
Crural diaphragm
- DCI:
-
Distal contractile integral
- EPT:
-
Esophageal pressure topography
- EGJ-CI:
-
Esophagogastric junction contractile integral
- GERD:
-
Gastroesophageal reflux disease
- HRM:
-
High-resolution manometry
- HRIM:
-
High-resolution impedance manometry
- IRB:
-
Institutional review board
- IRP:
-
Integrated relaxation pressure
- LES:
-
Lower esophageal sphincter
- MII-pH:
-
Multichannel intraluminal impedance-pH
- PPI:
-
Proton pump inhibitor
- TLESR:
-
Transient lower esophageal sphincter relaxation
References
Kahrilas PJ, Bredenoord A, Fox M, et al. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015;27:160–174.
Abdel Jalil AA, Castell DO. Ineffective esophageal motility (IEM): the old-new frontier in esophagology. Curr Gastroenterol Rep. 2016;18:1.
Blonski W, Vela M, Safder A, Hila A, Castell DO. Revised criterion for diagnosis of ineffective esophageal motility is associated with more frequent dysphagia and greater bolus transit abnormalities. Am J Gastroenterol. 2008;103:699–704.
Vinjirayer E, Gonzalez B, Brensinger C, et al. Ineffective motility is not a marker for gastroesophageal reflux disease. Am J Gastroenterol. 2003;98:771–776.
Ho SC, Chang CS, Wu CY, Chen GH. Ineffective esophageal motility is a primary motility disorder in gastroesophageal reflux disease. Dig Dis Sci. 2002;47:652–656. https://doi.org/10.1023/A:1017992808762.
Jain A, Baker JR, Chen JW. In ineffective esophageal motility, failed swallows are more functionally relevant than weak swallows. Neurogastroenterol Motil. 2018;30:e13297.
Min YW, Shin I, Son HJ, Rhee PL. Multiple rapid swallow maneuver enhances the clinical utility of high-resolution manometry in patients showing ineffective esophageal motility. Medicine (Baltimore). 2015;94:e1669.
Mello MD, Shriver AR, Li Y, Patel A, Gyawali CP. Ineffective esophageal motility phenotypes following fundoplication in gastroesophageal reflux disease. Neurogastroenterol Motil. 2016;28:292–298.
Shaker A, Stoikes N, Drapekin J, Kushnir V, Brunt LM, Gyawali CP. Multiple rapid swallow responses during esophageal high-resolution manometry reflect esophageal body peristaltic reserve. Am J Gastroenterol. 2013;108:1706–1712.
Rengarajan A, Bolkhir A, Gor P, Wang D, Munigala S, Gyawali CP. Esophagogastric junction and esophageal body contraction metrics on high-resolution manometry predict esophageal acid burden. Neurogastroenterol Motil. 2018;30:e13267.
Ravi K, Friesen L, Issaka R, Kahrilas PJ, Pandolfino JE. Long-term outcomes of patients with normal or minor motor function abnormalities detected by high-resolution esophageal manometry. Clin Gastroenterol Hepatol. 2015;13:1416–1423.
Goyal O, Bansal M, Sood A. Esophageal motility disorders: symptomatic and manometric spectrum in Punjab, northern India. Indian J Gastroenterol. 2017;36:202–208.
Roman S, Pandolfino JE, Chen J, Boris L, Luger D, Kahrilas PJ. Phenotypes and clinical context of hypercontractility in high-resolution esophageal pressure topography (EPT). Am J Gastroenterol. 2012;107:37–45.
Jonasson C, Wernersson B, Hoff DA, Hatlebakk JG. Validation of the GerdQ questionnaire for the diagnosis of gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2013;37:564–572.
Park MI. Recent concept in interpreting high-resolution manometry. J Neurogastroenterol Motil. 2010;16:90–93.
Nicodeme F, Pipa-Muniz M, Khanna K, Kahrilas PJ, Pandolfino JE. Quantifying esophagogastric junction contractility with a novel HRM topographic metric, the EGJ-Contractile Integral: normative values and preliminary evaluation in PPI non-responders. Neurogastroenterol Motil. 2014;26:353–360.
Sifrim D, Castell D, Dent J, Kahrilas PJ. Gastro-oesophageal reflux monitoring: review and consensus report on detection and definitions of acid, non-acid, and gas reflux. Gut. 2004;53:1024–1031.
Gyawali CP, Kahrilas PJ, Savarino E, et al. Modern diagnosis of GERD: the Lyon Consensus. Gut. 2018;67:1351–1362.
Monrroy H, Cisternas D, Bilder C, et al. The Chicago classification 3.0 results in more normal findings and fewer hypotensive findings with no difference in other diagnoses. Am J Gastroenterol. 2017;112:606–612.
Reddy CA, Patel A, Gyawali CP. Impact of symptom burden and health-related quality of life (HRQOL) on esophageal motor diagnoses. Neurogastroenterol Motil. 2017;29:e12970.
Kasamatsu S, Matsumura T, Ohta Y, et al. The effect of ineffective esophageal motility on gastroesophageal reflux disease. Digestion. 2017;95:221–228.
Jiang L, Ye B, Wang Y, Wang M, Lin L. Esophageal body motility for clinical assessment in patients with refractory gastroesophageal reflux symptoms. J Neurogastroenterol Motil. 2017;23:64–71.
Shetler KP, Bikhtii S, Triadafilopoulos G. Ineffective esophageal motility: clinical, manometric, and outcome characteristics in patients with and without abnormal esophageal acid exposure. Dis Esophagus. 2017;30:1–8.
Tolone S, de Cassan C, de Bortoli N, et al. Esophagogastric junction morphology is associated with a positive impedance-pH monitoring in patients with GERD. Neurogastroenterol Motil. 2015;27:1175–1182.
Author information
Authors and Affiliations
Contributions
CAR was involved in study planning, collection and analysis of data, interpretation of the data, and drafting of manuscript. JRB collected the data, interpreted the data, and edited the manuscript. JL planned the study, interpreted the data, and edited the manuscript. JWC was involved in study planning, interpretation of data, editing and approval of final manuscript. All authors have approved the submitted final draft.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Reddy, C.A., Baker, J.R., Lau, J. et al. High-Resolution Manometry Diagnosis of Ineffective Esophageal Motility Is Associated with Higher Reflux Burden. Dig Dis Sci 64, 2199–2205 (2019). https://doi.org/10.1007/s10620-019-05633-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-019-05633-3