Abstract
Purpose
To clarify recent trends in the use of intravitreal injections of anti-vascular endothelial growth factor (VEGF) in Japan.
Study design
Retrospective cohort study.
Methods
We used the DeSC database, a large-scale claims database for Japan, for entries between April 2014 and March 2021. We counted the number of anti-VEGF drug injections (aflibercept, ranibizumab, brolucizumab, and pegaptanib) administered every year, calculated the sex- and age-adjusted injection rates, and stratified these rates according to sex, age categories, anti-VEGF drugs, and diagnoses. We also calculated the number of injections administered within one year after the first injection according to the diagnoses.
Results
In total, 164,451 cases of anti-VEGF injections were identified. The sex- and age-adjusted rates of anti-VEGF injections per 1000 person-years increased from 7.9 in 2014 to 16.1 in 2020. Men were approximately twice as likely to receive anti-VEGF injections than women. The 70–79, 80–89, and ≥90 age categories had the highest rates, accounting for approximately 80%. Neovascular age-related macular degeneration had the highest rate, accounting for 60–70% over the study period. Aflibercept was the most commonly used drug, accounting for approximately 80% over the study period. The average number of injections within one year after the first injection was 4.4 for neovascular age-related macular degeneration, 2.7 for branch retinal vein occlusion, 3.1 for central retinal vein occlusion, and 3.5 for diabetic macular edema in 2020.
Conclusion
These findings can be used as a benchmark for the clinical practice of anti-VEGF therapy.
Similar content being viewed by others
Introduction
Many randomized controlled studies show that intravitreal injections of anti-vascular endothelial growth factors (VEGF) provide notable benefits for patients with neovascular age-related macular degeneration (nAMD) [1], branch retinal vein occlusion (BRVO) [2, 3], central retinal vein occlusion (CRVO) [2, 4], diabetic macular edema (DME) [5,6,7,8], myopic choroidal neovascularization (mCNV) [9, 10], neovascular glaucoma (NVG) [11], and retinopathy of prematurity (ROP) [12, 13].
Trends in the use of anti-VEGF are reported in various countries, the US [14, 15], the UK [16], and Italy [17]. A large claims’ database study was conducted in Japan [18], in which the age of the participants ranged from 21–75 years. Considering the aging population in Japan and the high prevalence of diseases such as nAMD and RVO in the elderly [19, 20], it is necessary to include all ages to understand the details of the trends.
We aimed to investigate more recent trends (2014–2021) in the use of anti-VEGF medication in Japan by using a large claims database containing information regarding all ages.
Subjects and methods
Data source
We used the DeSC database (DeSC Healthcare Inc.) for entries between April 2014 and March 2021. This database was developed in 2021 and comprises health insurance claims’ data from multiple types of health insurers: (1) health insurance for employees of large companies (Kempo), (2) the National Health Insurance for unemployed (Kokuho), and (3) the Advanced Elderly Medical Service System for elderly individuals aged ≥75 years (Koki Koreisha Iryo Seido). Thus, the DeSC database covers young, middle-aged, and elderly individuals. The individual-level data on outpatients and inpatients are anonymously stored. The information stored is as follows: (1) unique identifier; (2) age and sex; (3) diagnoses based on the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision codes; (4) procedures; (5) drugs dispensed based on the Anatomical Therapeutic Chemical Classification System; and (6) period from start to end of insurance.
The DeSC database reportedly contains the information of 2,220,702 individuals, including 824,516 individuals from Kempo, 1,095,713 individuals from Kokuho, and 300,473 individuals from Koki Koreisha Iryo Seido, between December 2019 and November 2020 [21]. Contrastingly, the Ministry of Health, Labour and Welfare, Japan, report that 78 million, 27 million, and 18 million individuals were enrolled in Kempo, Kokuho, and Koki Koreisha Iryo Seido, respectively, as of March 2020 [22]. Therefore, the DeSC database has a higher proportion of individuals from Kokuho than from the entire population.
This study was conducted in accordance with the tenets of the Declaration of Helsinki. This study was approved by the Institutional Review Board of the University of Tokyo. The requirement for informed consent was waived due to the anonymous nature of the database.
Outcomes
The number of anti-VEGF injections and patients receiving anti-VEGF injections
We defined intravitreal anti-VEGF injections as the prescription of anti-VEGF drugs, such as aflibercept, ranibizumab, brolucizumab, and pegaptanib. The codes used to identify these drugs are shown in Online Resource 1.
We counted the number of anti-VEGF injections stratified according to the fiscal year. The fiscal year is defined as the period from April to March (hereafter, the year refers to the fiscal year). If an individual received two or more injections in the same month, they were counted separately. We subsequently stratified the number of injections according to the sex, age category (≤39, 40–49, 50–59, 60–69, 70–79, 80–89, and ≥90 years), anti-VEGF drugs (aflibercept, ranibizumab, brolucizumab, and pegaptanib), and diagnoses (nAMD, BRVO, CRVO, DME, mCNV, NVG, ROP, multiple diagnoses, and unspecified). The diagnoses were identified based on the recorded diagnoses in the same year and month as the prescription of drugs. The codes used to identify these drugs are shown in Online Resource 2. The multiple diagnoses group included cases that had two or more diagnoses amongst nAMD, BRVO, CRVO, DME, mCNV, NVG, and ROP in the same year and month as the use of anti-VEGF drugs. The unspecified group was defined as cases that did not have any of the abovementioned diagnoses. The use of anti-VEGF drugs before or without approval was included. For example, we included cases in which only NVG was registered, and aflibercept was simultaneously administered before 2019. The approval timings for the anti-VEGF drugs are shown in Online resource 3.
We also counted the number of unique patients receiving anti-VEGF injections in each fiscal year and stratified this number according to sex and age category.
The rate of anti-VEGF injections
The total number of injections depends on the number of beneficiaries enrolled in the DeSC database. Thus, we calculated the injection rates by year, using the number of injections as the numerator and the total person-years at risk for all the beneficiaries in the same year as the denominator. These rates were expressed as the number of injections per 1000 person-years, as in previous studies [15]. Furthermore, we stratified the injection rates according to sex, age category, anti-VEGF drugs, diagnoses, and drugs and diagnoses. We adjusted the rates by sex and age using the direct standardization method [20, 23], with reference to the population in the DeSC database in 2020. We also calculated the distribution of the age category stratified by diagnosis in 2020.
The annual number of anti-VEGF injections after the first injections
We investigated the number of anti-VEGF injections per person within one year after the first injection. First, we identified the date of the first injection for each patient. We only included patients with more than one year of observation period after the first injections. We then included patients who received anti-VEGF injections for a single diagnosis among the abovementioned diagnoses within one year after the first injections (Online Resource 4). We subsequently counted the number of anti-VEGF injections within one year after the first injection. We used the years and diagnoses of the first injection dates to stratify the number of injections. Finally, we standardized the number of injections per person within one year after the first injection with reference to the population who underwent anti-VEGF injections at least once in 2020.
Comparison between the DeSC database and the whole population in Japan
Lastly, we investigated the representativeness of the DeSC database. We compared the number of anti-VEGF injections in the current study with that in the NDB open data for 2019 [24].
We used the statistical programming language R (version 3.5.0) for data cleaning, making graphs, and calculating the standardized rates.
Results
In total, 164,451 anti-VEGF injections were administered between 2014 and 2020. The total number of injections increased from 2221 in 2014 to 60,229 in 2020, with an increase in the total person-years (the denominator of the injection rate) from 516,350 to 3,753,480 (Table 1). The number of patients receiving anti-VEGF injections increased from 947 in 2014 to 20,145 in 2020.
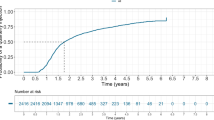
The crude injection rates per 1,000 person-years were 5.0 (2014), 3.1 (2015), 3.5 (2016), 4.2 (2017), 12.7 (2018), 13.9 (2019), and 16.1 (2020) in fiscal years (Fig. 1). The sex- and age-adjusted rates of the injections per 1,000 person-years increased from 7.9 in 2014 to 16.1 in 2020 (Fig. 2), increasing by 104 % (2.04-fold) over 7 years.
The injection rates for men increased from 11.6 to 20.8, and for women from 4.9 to 12.1, from 2014 to 2020. (Fig. 2). Men accounted for approximately 60–70% of the total injections over the period. All age categories show increases in the injection rates from 2014–2020, with the rate for individuals in their 80s increasing by 111% (2.11-fold) from 13.4 to 28.3, 70s increasing by 87 % (1.87-fold) from 11.3 to 21.1, and people ≥90 years of age increasing by 133% (2.33-fold) from 7.6 to 17.7 (Fig. 3). These three age categories were most likely to receive injections, accounting for approximately 80%.
All diagnoses (excluding NVG and ROP) show increases in the injection rates from 2014 to 2020, with the rate of nAMD increasing by 83% (1.83-fold) from 5.3 to 9.7, BRVO by 122% (2.22-fold) from 0.9 to 2.0, CRVO by 73% (1.73-fold) from 0.55 to 0.95, DME by 442 % (5.42-fold) from 0.19 to 1.03, and mCNV by 80% (1.80-fold) from 0.05 to 0.09 (Fig. 4). The nAMD group shows the highest rate, accounting for 60–70% over the study period, followed by the BRVO group. Although CRVO and DME ranked third and fourth from 2014 to 2019, this order was reversed in 2020.
Over the study period, the rate of aflibercept increased by 130% (2.30-fold) from 5.4 to 12.4, and of ranibizumab increased by 28 % (1.28-fold) from 2.5 to 3.2 (Fig. 5). Pegaptanib peaked in 2015 at a rate of 0.06 but gradually decreased thereafter and finally was eliminated by 2020. The rate of brolucizumab was 0.43 in 2020. Aflibercept was the most commonly used drug, accounting for approximately 80% of the total injections over the study period.
Analysis stratified according to the drug and diagnosis shows that aflibercept gained popularity for use in nAMD, BRVO, and DME from 2014 to 2020, and the increase in the use of aflibercept and ranibizumab was similar for CRVO and mCNV (Fig. 6).
On stratifying the analysis according to the age category and diagnosis in 2020, the age category accounting for the majority was 80–89 years (51%) for nAMD, 70–79 years (43%) for BRVO, 80–89 years (47%) for CRVO, 70–79 years (48%) for DME, 70–79 years (50%) for mCNV, 70–79 years (49%) for NVG, and ≤39 years (100%) for ROP (Online Resource 5).
The average number of injections per person within one year after the first injection tended to increase for all diseases except NVG (Fig. 7). The number of injections for nAMD increased from 3.4 to 4.4, BRVO from 2.1 to 2.7, CRVO from 2.7 to 3.1, DME from 2.8 to 3.5, and mCNV from 2.4 to 2.9, over the study period.
Annual number of anti-VEGF injections after the first injections according to diagnosis. nAMD neovascular age-related macular degeneration, BRVO branch retinal vein occlusion, CRVO central retinal vein occlusion, DME diabetic macular edema, mCNV myopic choroidal neovascularization, NVG neovascular glaucoma
Comparing the number of injections in the DeSC database with that in the NDB open data, the age distribution of the DeSC database was somewhat biased toward older individuals (the furthest right column in Table 1). Injections administered to individuals aged ≥70 years accounted for 90% in the DeSC database, whereas they accounted for 72% in the whole population. The distribution of sex and drugs was similar in the DeSC database and NDB open data.
Discussion
Here we clarify the recent trends in the use of anti-VEGF drugs using a large-scale claims database. The total injection rate in 2020 was approximately 16 per 1000 person-years. The injections were most commonly administered to men to people in their 80s, and those with nAMD. Aflibercept was the most commonly used drug. These trends were observed over the period between 2014 and 2020.
The total sex- and age-adjusted injection rates increased by 104% between 2014 and 2020. The possible reasons for this increase include (1) the approval of the use of ranibizumab and aflibercept for the treatment of BRVO, CRVO, and DME between 2013 and 2015. The pivotal clinical trials after 2014 demonstrating the effectiveness of anti-VEGF drugs may have accelerated anti-VEGF use [3, 4, 8]. Previous surveys show that the proportion of ophthalmologists choosing anti-VEGF injections as the first choice therapy for DME increased from 73% in 2015 to 81% in 2016–2017 [25, 26] in Japan. Although only one survey investigated the preference regarding the treatment of RVO in Japan [27], 100% of ophthalmologists chose anti-VEGF injections as the first therapy; (2) the spread of spectral-domain optical coherence tomography (OCT) in Japan between 2014 and 2020. OCT can detect even the slightest lesions, such as subretinal fluid and intraretinal fluid; it has become the current standard in ophthalmic clinical practice [28]. This spread may have lowered the threshold for the administration of anti-VEGF drugs; and (3) the changes in the guiding criteria for the retreatment of nAMD. The criteria initially consisted of quantitative measures, such as OCT-measured central retinal thickness [29, 30]; however, qualitative measures, such as evidence of the presence of fluid on OCT, are now indicated [31]. This may have contributed to the increase in anti-VEGF injections.
According to the current study men were more likely to receive injections than women. A possible reason is that most of the diagnoses were nAMD. Two previous population-based studies conducted in Japan showed that the prevalence of nAMD was higher among men than that among women, and this trend was the opposite of that observed in caucasians [32, 33]. This sex gap may be due to the following characteristics unique to Japan: (1) a higher proportion of smokers among men, (2) a high prevalence of polypoidal choroidal vasculopathy, a type of nAMD more likely to develop in men than in women, and (3) differences in the genetic composition of nAMD, such as the complement factor H gene [33].
The elderly were more likely to receive injections than the middle-aged and young. This may be related to the prevalence of the diseases. Older age is a significant risk factor for AMD [19] and RVO [20]. These two diseases accounted for the majority of the population in the current study; thus, the proportion of the elderly aged 70–79, 80–89, and ≥90 years were larger than other age categories.
The injection rates for nAMD, BRVO, CRVO, and DME increased during the study period. Among all the diagnoses, except for unspecified diagnoses, the highest rate was observed for nAMD, followed by BRVO, DME, and CRVO in 2020. This order was consistent with a previous study that used a claims database in Japan from 2008 to 2015 [18]. However, previous population-based cohort studies in Japan report that, among people aged ≥50 years the prevalence of nAMD was 0.7% in 1998 [32] and 0.6% in 2000–2002 [19], that of BRVO was 2.4% in 1998 [20], and of CRVO was 0.2% in 1998 [20]. Furthermore, a survey conducted in 2019 reports that the prevalence of DM was 19.7% in men and 10.8% in women (approximately 15% of the total population) [34], whereas a meta-analysis showed that the estimated prevalence of DME was 7.4% among patients with DM [35]; thus, the prevalence of DME in the general population would be approximately 1.1% (= 0.15*0.074), signifying that nAMD was not the highest.
This difference between the injection rates and prevalence may be attributed to the different levels of necessity to treat the diseases. Almost all nAMD patients should be treated with anti-VEGF injections regularly because nAMD is vision-threatening, and anti-VEGF is usually the first choice of treatment, as established by the AMD guidelines [36]. In contrast, only 5–15% of BRVO develop macular edema [37]. Furthermore, alternative therapies, such as laser photocoagulation and vitrectomy, can be used in the treatment of RVO [27]. Alternative therapies for DME, such as sub-Tenon's corticosteroid and vitrectomy, would lower the injections’ rates farther than in nAMD [38]. Our analysis reveals that the number of injections within one year after the first injection was higher for nAMD (4.4) compared with BRVO (2.7) and DME (3.5) in 2020.
The injection rates for DME continued to increase and surpassed those of CRVO in 2020. Since the number of cases of diabetes mellitus in Japan was stable between 2010 and 2019 [34], there is a possibility that the treatment pattern of DME has been gradually changing. This is supported by surveys that report a recent preference for anti-VEGF therapy over other treatments, such as sub-Tenon’s corticosteroid and laser photocoagulation, in the treatment of DME [25, 26]. Specifically, the proportion of ophthalmologists choosing anti-VEGF injections as the first therapy has increased from 73% in 2015 to 81% in 2016–2017 [25, 26].
The analysis stratified according to drugs shows the popularity of aflibercept compared with ranibizumab in the treatment of nAMD, BRVO, and DME. Ranibizumab binds to VEGF-A, whereas aflibercept traps VEGF-A, VEGF-B, and placental growth factor [39, 40]. This difference in their pharmacological function may be associated with the following clinical superiorities of aflibercept over ranibizumab. First, some studies report a higher possibility of polyp regression with the administration of aflibercept compared with ranibizumab for polypoidal choroidal vasculopathy [41, 42]. Since the prevalence of polypoidal choroidal vasculopathy is high among Asians, the effectiveness of aflibercept may have contributed to its popularity. Second, aflibercept can decrease choroidal thickness to a greater extent than ranibizumab [43]. Third, one study reports that nAMD cases with choroidal vascular hyperpermeability had better visual outcomes when treated with aflibercept than with ranibizumab [44]. The second and third results imply that aflibercept can suppress the exudative tendency of the choroid more potently than ranibizumab. Furthermore, in terms of cost, aflibercept was cheaper than ranibizumab (JPY 137, 292 vs. JPY 160,698 as of March 2021). The abovementioned reasons likely contributed to the popularity of aflibercept in the treatment of nAMD.
The Diabetic Retinopathy Clinical Research Network Protocol T study reports that visual acuity at one year was better in patients treated with aflibercept than in those treated with ranibizumab whenever their baseline visual acuity was < 20/50 [45]. The superiority of aflibercept over ranibizumab disappeared at two years, but from the perspective of the area under the curve [46], some ophthalmologists may have preferred aflibercept for the treatment of DME. There is no clear evidence of the superiority of aflibercept over ranibizumab in treating RVO. For example, a recent randomized controlled study (LEAVO study) did not show the superiority of aflibercept over ranibizumab in the treatment of macular edema secondary to CRVO [47]. Hence, why aflibercept is more likely to be chosen for the treatment of RVO in recent years remains unknown.
The current study had several limitations. First, not all diagnoses were accurately identified because some patients had multiple diagnoses in the same year and month as the injections or because they did not have any of the abovementioned diagnoses. We may have to develop algorithms to predict the true diagnoses from the data of diagnoses, drugs, and procedures of adjacent months. Second, the claims data are subject to coding errors and omissions. Third, we did not account for the influence of the COVID-19 pandemic. This may influence -patients’ behaviour whenever there is a need to consult a doctor; However, an increasing trend in injection rates was observed in 2020. Fourth, when interpreting the current results we must consider the age distribution of the DeSC database as the proportion of older individuals in the DeSC database was higher than that in the whole population in Japan.
One of the strengths of the current study is that it includes a large number of people using large-scale claims’ data. This enabled us to estimate the injection rates with small variance. Another strength is that the DeSC database includes all ages, including >75 years, in addition to information on the diagnoses (unlike the NDB open data). Since the prevalence of nAMD and RVO is strongly associated with older age [32, 33], it is essential to include the elderly to provide all the details of the anti-VEGF injections administered.
In conclusion, the current study clarifies the recent trends in anti-VEGF injections in Japan using a large claims’ database. The total injection rate increased by 104% between 2014 and 2020. Men, the elderly aged ≥70 years, nAMD, and aflibercept had a large share in the stratified analyses according to sex, age category, diagnosis, and drug use. The current findings help understand the details of the use of anti-VEGF drugs in recent Japanese clinical practice and can become a benchmark for anti-VEGF drug injections.
Data availability
We used de-identified, individual-level data obtained from the DeSC Claims Database (Tokyo, Japan). The address of their HP is https://desc-hc.co.jp. Data may be obtained from the Inc. and are not publicly available.
References
Rofagha S, Bhisitkul RB, Boyer DS, Sadda SR, Zhang K. Seven-year outcomes in ranibizumab-treated patients in ANCHOR, MARINA, and HORIZON. Ophthalmology. 2013;120:2292–9.
Varma R, Bressler NM, Suñer I, Lee P, Dolan CM, Ward J, et al. Improved vision-related function after ranibizumab for macular edema after retinal vein occlusion: results from the bravo and cruise trials. Ophthalmology. 2012;119:2108–18.
Clark WL, Boyer DS, Heier JS, Brown DM, Haller JA, Vitti R, et al. Intravitreal aflibercept for macular edema following branch retinal vein occlusion: 52-week results of the vibrant study. Ophthalmology. 2016;123:330–6.
Ogura Y, Roider J, Korobelnik J-F, Holz FG, Simader C, Schmidt-Erfurth U, et al. Intravitreal aflibercept for macular edema secondary to central retinal vein occlusion: 18-month results of the phase 3 GALILEO study. Am J Ophthalmol. 2014;158:1032-8.e2.
Massin P, Bandello F, Garweg JG, Hansen LL, Harding SP, Larsen M, et al. Safety and efficacy of ranibizumab in diabetic macular edema (resolve study): a 12-month, randomized, controlled, double-masked, multicenter phase II study. Diabetes Care. 2010;33:2399–405.
Nguyen QD, Brown DM, Marcus DM, Boyer DS, Patel S, Feiner L, et al. Ranibizumab for diabetic macular edema: results from 2 phase III randomized trials: RISE and RIDE. Ophthalmology. 2012;119:789–801.
Elman MJ, Aiello LP, Beck RW, Bressler NM, Bressler SB, Diabetic Retinopathy Clinical Research Network, et al. Randomized trial evaluating ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmology. 2010;117:1064-77.e35.
Heier JS, Korobelnik J-F, Brown DM, Schmidt-Erfurth U, Do DV, Midena E, et al. Intravitreal aflibercept for diabetic macular edema. Ophthalmology. 2016;123:2376–85.
Ikuno Y, Ohno-Matsui K, Wong TY, Korobelnik J-F, Vitti R, Li T, et al. Intravitreal aflibercept injection in patients with myopic choroidal neovascularization. Ophthalmology. 2015;122:1220–7.
Wolf S, Balciuniene VJ, Laganovska G, Menchini U, Ohno-Matsui K, Sharma T, et al. RADIANCE: a randomized controlled study of ranibizumab in patients with choroidal neovascularization secondary to pathologic myopia. Ophthalmology. 2014;121:682-92.e2.
Inatani M, Higashide T, Matsushita K, Miki A, Ueki M, Iwamoto Y, et al. Intravitreal aflibercept in Japanese patients with neovascular glaucoma: the VEGA randomized clinical trial. Adv Ther. 2021;38:1116–29.
Stahl A, Lepore D, Fielder A, Fleck B, Reynolds JD, Chiang MF, et al. Ranibizumab versus laser therapy for the treatment of very low birthweight infants with retinopathy of prematurity (RAINBOW): an open-label randomised controlled trial. The Lancet. 2019;394:1551–9.
Stahl A, Krohne TU, Eter N, Oberacher-Velten I, Guthoff R, Meltendorf S, et al. Comparing alternative ranibizumab dosages for safety and efficacy in retinopathy of prematurity: a randomized clinical trial. JAMA Pediatr. 2018;172:278.
Berkowitz ST, Sternberg P, Feng X, Chen Q, Patel S. Analysis of anti–vascular endothelial growth factor injection claims data in US medicare part B beneficiaries from 2012 to 2015. JAMA Ophthalmol. 2019;137:921.
Parikh R, Ross JS, Sangaralingham LR, Adelman RA, Shah ND, Barkmeier AJ. Trends of anti-vascular endothelial growth factor use in ophthalmology among privately insured and medicare advantage patients. Ophthalmology. 2017;124:352–8.
Chopra R, Preston GC, Keenan TDL, Mulholland P, Patel PJ, Balaskas K, et al. Intravitreal injections: past trends and future projections within a UK tertiary hospital. Eye Lond Engl. 2022;36:1373–8.
Perrone V, Dovizio M, Veronesi C, Citraro R, De Francesco A, Dell’Orco S, et al. Retrospective analysis of the pharmaco-utilization of VEGF inhibitors and health care costs among patients with wet age-related macular degeneration and other ocular diseases in Italy. Int J Environ Res Public Health. 2022;19:2548.
Kawasaki R, Bauer M, Bezlyak V, Ogura Y. Treatment patterns for retinal diseases in patients newly-treated with anti-VEGF agents: a retrospective analysis of claims data from the Japan medical data center database. Jpn J Ophthalmol. 2021;65:215–26.
Kawasaki R, Wang JJ, Ji G, Taylor B, Oizumi T, Daimon M, et al. Prevalence and risk factors for age-related macular degeneration in an adult Japanese population: the Funagata study. Ophthalmology. 2008;115:1376-81.e2.
Yasuda M, Kiyohara Y, Arakawa S, Hata Y, Yonemoto K, Doi Y, et al. Prevalence and systemic risk factors for retinal vein occlusion in a general Japanese population: the hisayama study. Investig Opthalmology Vis Sci. 2010;51:3205.
Okada A, Yasunaga H. Prevalence of noncommunicable diseases in Japan using a newly developed administrative claims database covering young, middle-aged, and elderly people. JMA J. 2022;5:190–8.
Ministry of Health, Labour and Welfare, Japan. Universal health insurance system. https://www.mhlw.go.jp/bunya/iryouhoken/iryouhoken01/dl/01a.pdf. Accessed 7 Sep 2022 (in Japanese)
Fay MP, Feuer EJ. Confidence intervals for directly standardized rates: a method based on the gamma distribution. Stat Med. 1997;16:791–801.
Ministry of Health, Labour and Welfare, Japan. NDB open data. https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000177182.html. Accessed 7 Sep 2022 (in Japanese)
Sugimoto M, Tsukitome H, Okamoto F, Oshika T, Ueda T, Niki M, et al. Clinical preferences and trends of anti-vascular endothelial growth factor treatments for diabetic macular edema in Japan. J Diabetes Investig. 2019;10:475–83.
Ogura Y, Shiraga F, Terasaki H, Ohji M, Ishida S, Sakamoto T, et al. Clinical practice pattern in management of diabetic macular edema in Japan: survey results of Japanese retinal specialists. Jpn J Ophthalmol. 2017;61:43–50.
Ogura Y, Kondo M, Kadonosono K, Shimura M, Kamei M, Tsujikawa A. Current practice in the management of branch retinal vein occlusion in Japan: survey results of retina specialists in Japan. Jpn J Ophthalmol. 2019;63:365–73.
Fujimoto J, Swanson E. The development, commercialization, and impact of optical coherence tomography. Investig Opthalmol Vis Sci. 2016;57:1–13.
Holz FG, Amoaku W, Donate J, Guymer RH, Kellner U, Schlingemann RO, et al. Safety and efficacy of a flexible dosing regimen of ranibizumab in neovascular age-related macular degeneration: the SUSTAIN study. Ophthalmology. 2011;118:663–71.
Lalwani GA, Rosenfeld PJ, Fung AE, Dubovy SR, Michels S, Feuer W, et al. A variable-dosing regimen with intravitreal ranibizumab for neovascular age-related macular degeneration: year 2 of the PrONTO study. Am J Ophthalmol. 2009;148:43-58.e1.
Martin DF, Maguire MG, Ying G, Grunwald JE, Fine SL, CATT Research Group, et al. Ranibizumab and bevacizumab for neovascular age-related macular degeneration. N Engl J Med. 2011;364:1897–908.
Oshima Y, Ishibashi T, Murata T, Tahara Y, Kiyohara Y, Kubota T. Prevalence of age related maculopathy in a representative Japanese population: the Hisayama study. Br J Ophthalmol. 2001;85:1153–7.
Kawasaki R, Wang JJ, Rochtchina E, Taylor B, Wong TY, Tominaga M, et al. Cardiovascular risk factors and retinal microvascular signs in an adult japanese population: the funagata study. Ophthalmology. 2006;113:1378–84.
Ministry of Health, Labour and Welfare, Japan. National health and nutrition survey (2019). https://www.mhlw.go.jp/content/10900000/000687163.pdf. Accessed 9 Apr 2022 (in Japanese).
Yau JWY, Rogers SL, Kawasaki R, Lamoureux EL, Kowalski JW, Bek T, et al. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care. 2012;35:556–64.
Takahashi K, Ogura Y, Ishibashi T, Shiraga F, Yuzawa M. Treatment guidelines for age-related macular degeneration. Nippon Ganka Gakkai Zasshi. 2012;116:1150–5 (in Japanese).
Rogers SL, McIntosh RL, Lim L, Mitchell P, Cheung N, Kowalski JW, et al. Natural history of branch retinal vein occlusion: An evidence-based systematic review. Ophthalmology. 2010;117:1094-101.e5.
Moulin TA, Adjei Boakye E, Wirth LS, Chen J, Burroughs TE, Vollman DE. Yearly treatment patterns for patients with recently diagnosed diabetic macular edema. Ophthalmol Retina. 2019;3:362–70.
Papadopoulos N, Martin J, Ruan Q, Rafique A, Rosconi MP, Shi E, et al. Binding and neutralization of vascular endothelial growth factor (VEGF) and related ligands by VEGF Trap, ranibizumab and bevacizumab. Angiogenesis. 2012;15:171–85.
Fogli S, Del Re M, Rofi E, Posarelli C, Figus M, Danesi R. Clinical pharmacology of intravitreal anti-VEGF drugs. Eye (Lond). 2018;32:1010–20.
Cho HJ, Kim KM, Kim HS, Han JI, Kim CG, Lee TG, et al. Intravitreal aflibercept and ranibizumab injections for polypoidal choroidal vasculopathy. Am J Ophthalmol. 2016;165:1–6.
Hosokawa M, Shiraga F, Yamashita A, Shiragami C, Ono A, Shirakata Y, et al. Six-month results of intravitreal aflibercept injections for patients with polypoidal choroidal vasculopathy. Br J Ophthalmol. 2015;99:1087–91.
Gharbiya M, Cruciani F, Mariotti C, Grandinetti F, Marenco M, Cacace V. Choroidal thickness changes after intravitreal antivascular endothelial growth factor therapy for age-related macular degeneration: ranibizumab versus aflibercept. J Ocul Pharmacol Ther. 2015;31:357–62.
Hata M, Oishi A, Tsujikawa A, Yamashiro K, Miyake M, Ooto S, et al. Efficacy of intravitreal injection of aflibercept in neovascular age-related macular degeneration with or without choroidal vascular hyperpermeability. Invest Ophthalmol Vis Sci. 2014;55:7874–80.
Wells JA, Glassman AR, Ayala AR, Jampol LM, Bressler NM, Bressler SB, et al. Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema: two-year results from a comparative effectiveness randomized clinical trial. Ophthalmology. 2016;123:1351–9.
Gross JG, Glassman AR, Jampol LM, Inusah S, Aiello LP, Writing Committee for the Diabetic Retinopathy Clinical Research Network, et al. Panretinal photocoagulation vs intravitreous ranibizumab for proliferative diabetic retinopathy: a randomized clinical trial. JAMA. 2015;314:2137.
Hykin P, Prevost AT, Sivaprasad S, Vasconcelos JC, Murphy C, Kelly J, et al. Intravitreal ranibizumab versus aflibercept versus bevacizumab for macular oedema due to central retinal vein occlusion: the LEAVO non-inferiority three-arm RCT. Health Technol Assess. 2021;25:1–196.
Acknowledgments
This work was supported by grants from the Ministry of Health, Labour and Welfare, Japan (H30-Policy-Designated-004 and H29-ICT-General-004) and the Ministry of Education, Culture, Sports, Science and Technology, Japan (17H04141). The sponsor or funding organization had no role in the design or conduct of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Y. Hashimoto, None; A. Okada, None; H. Matsui, None; H. Yasunaga, None; M. Aihara, Grants or contracts (Santen, Senju, Alcon, Novartis, Pfizer, Kowa, Otsuka, Wakamoto, Johnson & Johnson, Glaukos, TOMEY, Ono, CREWT Medical Systems, Sato), Consulting fees (Santen, Senju, Alcon, Pfizer, Kowa, Otsuka, Wakamoto, HOYA, Glaukos, IRIDEX, Astellas), Payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events (Santen, Senju, Alcon, Novartis, Pfizer, Kowa, Otsuka, Johnson & Johnson, HOYA, Glaukos, TOMEY, IRIDEX, CREWT Medical Systems, Canon, ZEISS, Sato), Participation on a Data Safety Monitoring Board or Advisory Board (Santen, Senju, HOYA, Kowa), Receipt of equipment, materials, drugs, medical writing, gifts or other services (Kowa, Santen); R. Obata, Payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events (Novartis, Bayer, Santen, Senju, Alcon).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Corresponding Author: Yohei Hashimoto
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Hashimoto, Y., Okada, A., Matsui, H. et al. Recent trends in anti-vascular endothelial growth factor intravitreal injections: a large claims database study in Japan. Jpn J Ophthalmol 67, 109–118 (2023). https://doi.org/10.1007/s10384-022-00969-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-022-00969-2