Abstract
Purpose
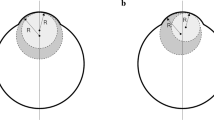
Orthokeratology for correction of myopia reduces corneal power by flattening corneal curvature and thinning central corneal thickness (CCT). Measurement of intraocular pressure (IOP) with a noncontact tonometer is known to be affected by CCT and corneal curvature. We investigated the influence of orthokeratology on such measurements of IOP.
Methods
This was a prospective, interventional case series derived from a clinical trial of orthokeratology lenses in two hospitals. Both eyes of 45 subjects were fitted with reverse-geometry lenses, worn for more than 4 h overnight for 52 weeks. Uncorrected visual acuity, refraction, IOP (with a noncontact tonometer), CCT, and corneal curvature were measured.
Results
Uncorrected visual acuity, spherical equivalent value, IOP, CCT, and the radius of corneal curvature were 0.93 ± 0.27, −2.87 ± 1.05 D, 13.5 ± 2.5 mmHg, 536.2 ± 39.6 μm, and 7.88 ± 0.25 mm, respectively, before orthokeratology, and 0.17 ± 0.34, −1.05 ± 1.18 D, 12.4 ± 2.7 mmHg, 528.6 ± 40.8 μm, and 8.10 ± 0.31 mm at 52 weeks after treatment. The changes in all parameters were significant, and the change in IOP was significantly correlated with that in CCT at 24 weeks and thereafter.
Conclusions
Orthokeratology for myopia leads to a decrease in IOP measured with a noncontact tonometer, likely as a result of the associated decrease in CCT.







Similar content being viewed by others
References
Damji KF, Munger R. Influence of central corneal thickness on applanation intraocular pressure. J Glaucoma. 2000;9:205–7.
Matsumoto T, Makino H, Uozato H, Saishin M, Miyamoto S. The influence of corneal thickness and curvature on the difference between intraocular pressure measurements obtained with a non-contact tonometer and those with a Goldmann applanation tonometer. Jpn J Ophthalmol. 2000;44:691.
Goldmann H, Schmidt T. Applanation tonometry. Ophthalmologica. 1957;134:221–42.
Purslow PP, Karwatowski WS. Ocular elasticity. Is engineering stiffness a more useful characterization parameter than ocular rigidity? Ophthalmology. 1996;103:1686–92.
Chihara E. Assessment of true intraocular pressure: the gap between theory and practical data. Surv Ophthalmol. 2008;53:203–18.
Swarbrick HA. Orthokeratology review and update. Clin Exp Optom. 2006;89:124–43.
Hiraoka T, Matsumoto Y, Okamoto F, Yamaguchi T, Hirohara Y, Mihashi T, et al. Corneal higher-order aberrations induced by overnight orthokeratology. Am J Ophthalmol. 2005;139:429–36.
Chen D, Lam AK, Cho P. A pilot study on the corneal biomechanical changes in short-term orthokeratology. Ophthalmic Physiol Opt. 2009;29:464–71.
Cheung SW, Cho P, Chan B. Astigmatic changes in orthokeratology. Optom Vis Sci. 2009;86:1352–8.
Choo JD, Caroline PJ, Harlin DD, Papas EB, Holden BA. Morphologic changes in cat epithelium following continuous wear of orthokeratology lenses: a pilot study. Contact Lens Anterior Eye. 2008;31:29–37.
Stillitano IG, Chalita MR, Schor P, Maidana E, Lui MM, Lipener C, et al. Corneal changes and wavefront analysis after orthokeratology fitting test. Am J Ophthalmol. 2007;144:378–86.
Tsukiyama J, Miyamoto Y, Higaki S, Fukuda M, Shimomura Y. Changes in the anterior and posterior radii of the corneal curvature and anterior chamber depth by orthokeratology. Eye Contact Lens. 2008;34:17–20.
Alharbi A, Swarbrick HA. The effects of overnight orthokeratology lens wear on corneal thickness. Invest Ophthalmol Vis Sci. 2003;44:2518–23.
Reinstein DZ, Gobbe M, Archer TJ, Couch D, Bloom B. Epithelial, stromal, and corneal pachymetry changes during orthokeratology. Optom Vis Sci. 2009;86:E1006–14.
Cheah PS, Norhani M, Bariah MA, Myint M, Lye MS, Azian AL. Histomorphometric profile of the corneal response to short-term reverse-geometry orthokeratology lens wear in primate corneas: a pilot study. Cornea. 2008;27:461–70.
Alharbi A, La Hood D, Swarbrick HA. Overnight orthokeratology lens wear can inhibit the central stromal edema response. Invest Ophthalmol Vis Sci. 2005;46:2334–40.
Barr JT, Rah MJ, Jackson JM, Jones LA. Orthokeratology and corneal refractive therapy: a review and recent findings. Eye Contact Lens. 2003;29:S49–53; discussion S7–9, S192–4.
Saw SM, Gazzard G, Shih-Yen EC, Chua WH. Myopia and associated pathological complications. Ophthalmic Physiol Opt. 2005;25:381–91.
Fournier AV, Podtetenev M, Lemire J, Thompson P, Duchesne R, Perreault C, et al. Intraocular pressure change measured by Goldmann tonometry after laser in situ keratomileusis. J Cataract Refract Surg. 1998;24:905–10.
Cronemberger S, Guimaraes CS, Calixto N, Calixto JMF. Intraocular pressure and ocular rigidity after LASIK. Arq Bras Oftalmol. 2009;72:439–43.
Siganos DS, Papastergiou GI, Moedas C. Assessment of the Pascal dynamic contour tonometer in monitoring intraocular pressure in unoperated eyes and eyes after LASIK. J Cataract Refract Surg. 2004;30:746–51.
Hsu SY, Chang MS, Lee CJ. Intraocular pressure assessment in both eyes of the same patient after laser in situ keratomileusis. J Cataract Refract Surg. 2009;35:76–82.
Yang CC, Wang IJ, Chang YC, Lin LL, Chen TH. A predictive model for postoperative intraocular pressure among patients undergoing laser in situ keratomileusis (LASIK). Am J Ophthalmol. 2006;141:530–6.
Climenhaga H, Plucinska H. Comparison of the Pulsair noncontact tonometer and the Goldmann applanation tonometer. Can J Ophthalmol. 1989;24:7–9.
Sorensen PN. The noncontact tonometer. Clinical evaluation on normal and diseased eyes. Acta Ophthalmol (Copenh). 1975;53:513–21.
Ko YC, Liu CJ, Hsu WM. Varying effects of corneal thickness on intraocular pressure measurements with different tonometers. Eye (Lond). 2005;19:327–32.
Acknowledgments
This study was supported in part by a grant (22791663) from the Ministry of Education, Culture, Sports, Science, and Technology of Japan.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Ishida, Y., Yanai, R., Sagara, T. et al. Decrease in intraocular pressure following orthokeratology measured with a noncontact tonometer. Jpn J Ophthalmol 55, 190–195 (2011). https://doi.org/10.1007/s10384-011-0018-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-011-0018-2