Summary
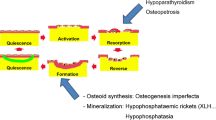
The heterogeneity of “rare bone disorders” can be explained by the number of molecules and regulatory pathways which are responsible for bone health and normal stature. In this article, the most important basic principles behind bone homeostasis from development to structure and regulation of the growing skeleton are summarized. The aim is to provide the reader with some theoretical background to understand the nature of the different main groups of disorders affecting bone stability, longitudinal growth and disturbances of calcium and phosphate homeostasis.
Zusammenfassung
Hinter der Gruppe seltener Knochenerkrankungen steht ursächlich eine Vielzahl unterschiedlicher Regulationsmechanismen, welche auch die Heterogenität der verschiedenen Erkrankungsbilder erklärt. In diesem Artikel soll ein Überblick über grundsätzliche Aspekte der Entwicklung, der Struktur und der Regulation des wachsenden Skelettsystems gegeben werden. Auf diese Weise sollen dem interessierten Leser die ganz unterschiedlichen seltenen Ursachen hinter erhöhter Frakturneigung, aber auch seltenen Wachstumsstörungen und Störungen der Mineralisation verständlich präsentiert werden.

Similar content being viewed by others
References
Robling AG, Bonewald LF. The Osteocyte: new insights. Annu Rev Physiol. 2020;82(1):485–506.
Kim J‑M, Lin C, Stavre Z, Greenblatt MB, Shim J‑H. Osteoblast-osteoclast communication and bone homeostasis. Cells. 2020;9(9):2073. https://doi.org/10.3390/cells9092073.
Udagawa N, Koide M, Nakamura M, Nakamichi Y, Yamashita T, Uehara S, et al. Osteoclast differentiation by RANKL and OPG signaling pathways. J Bone Miner Metab. 2020. https://doi.org/10.1007/s00774-020-01162-6.
Hunziker EB. Mechanism of longitudinal bone growth and its regulation by growth plate chondrocytes. Microsc Res Tech. 1994;28(6):505–19.
McKee M, Cole W. Bone matrix and mineralization. In: Glorieux F, Pettifor J, Juppner H, editors. Pediatric Bone. Biology and Diseases. Amsterdam: Elsevier; 2012. pp. 9–37.
Kronenberg HM. Developmental regulation of the growth plate. Nature. 2003;423(6937):332–6.
Zaidi M, Yuen T, Sun L, Rosen CJ. Regulation of skeletal homeostasis. Endocr Rev. 2018;39(5):701–18.
Hallett SA, Ono W, Ono N. Growth plate chondrocytes: skeletal development, growth and beyond. Int J Mol Sci. 2019;20(23):6009. https://doi.org/10.3390/ijms20236009.
Chung U, Lanske B, Lee K, Li E, Kronenberg H. The parathyroid hormone/parathyroid hormone-related peptide receptor coordinates endochondral bone development by directly controlling chondrocyte differentiation. Proc Natl Acad Sci U S A. 1998;95(22):13030–5.
Haeusler G, Raimann A, Egerbacher M. Growth plate research. In: Pietschmann P, editor. Principles of bone and joint research. Berlin Heidelberg: Springer; 2017. pp. 153–71. Learning Materials in Biosciences.
Golub EE. Role of matrix vesicles in biomineralization. Biochim Biophys Acta. 2009;1790(12):1592–8.
Orimo H. The mechanism of mineralization and the role of alkaline phosphatase in health and disease. J Nippon Med Sch. 2010;77(1):4–12.
Rowe PSN. Regulation of bone–renal mineral and energy metabolism: the PHEX, FGF23, DMP1, MEPE ASARM pathway. Crit Rev Eukaryot Gene Expr. 2012;22(1):61–86.
Florencio-Silva R, Sasso GRS, Sasso-Cerri E, Simões MJ, Cerri PS. Biology of Bone tissue: structure, function, and factors that influence bone cells. Biomed Res Int. 2015;2015:421746. https://doi.org/10.1155/2015/421746.
Siddiqui JA, Partridge NC. Physiological bone remodeling: systemic regulation and growth factor involvement. Physiology. 2016;31(3):233–45.
van der Eerden BCJ. Systemic and local regulation of the growth plate. Endocr Rev. 2003;24(6):782–801.
Lui JC, Nilsson O, Baron J. Growth plate senescence and catch-up growth. Endocr Dev. 2011;21:23–9.
Kaplan SA, Cohen P. REVIEW: the Somatomedin hypothesis 2007: 50 years later. J Clin Endocrinol Metab. 2007;92(12):4529–35.
Mortier GR, Cohn DH, Cormier-Daire V, Hall C, Krakow D, Mundlos S, et al. Nosology and classification of genetic skeletal disorders: 2019 revision. Am J Med Genet A. 2019;179(12):2393–419.
Etich J, Rehberg M, Eckes B, Sengle G, Semler O, Zaucke F. Signaling pathways affected by mutations causing osteogenesis imperfecta. Cell Signal. 2020;76:109789.
Saraff V, Högler W. Osteoporosis in children: diagnosis and management. Eur J Endocrinol. 2015;173(6):R185–97.
Van Dijk F, Sillence D. Osteogenesis imperfecta: clinical diagnosis, nomenclature and severity assessment. Am J Med Genet A. 2014;164(6):1470–81.
Boulet C, Madani H, Lenchik L, Vanhoenacker F, Amalnath DS, de Mey J, et al. Sclerosing bone dysplasias: genetic, clinical and radiology update of hereditary and non-hereditary disorders. Br J Radiol. 2016;89(1062):20150349. https://doi.org/10.1259/bjr.20150349.
Haffner D, Emma F, Eastwood DM, Duplan MB, Bacchetta J, Schnabel D, et al. Clinical practice recommendations for the diagnosis and management of X‑linked hypophosphataemia. Nat Rev Nephrol. 2019;15(7):435–55.
Stokes VJ, Nielsen MF, Hannan FM, Thakker RV. Hypercalcemic disorders in children. J Bone Miner Res. 2017;32(11):2157–70.
Allgrove J, Shaw NJ, editors. Calcium and Bone disorders in children and adolescents. Book: Karger; 2015.
Bringhurst FR, Demay MB, Kronenberg HM. Hormones and disorders of mineral metabolism. In: Williams textbook of endocrinology. Amsterdam: Elsevier; 2011. pp. 1277–94.
Thiele S, Mantovani G, Barlier A, Boldrin V, Bordogna P, De Sanctis L, et al. From pseudohypoparathyroidism to inactivating PTH/PTHrP signalling disorder (iPPSD), a novel classification proposed by the EuroPHP network. Eur J Endocrinol. 2016;175(6):P1–17.
Jee YH, Baron J, Nilsson O. New developments in the genetic diagnosis of short stature. Curr Opin Pediatr. 2018;30(4):541–7.
Pediatric Positions. ISCD.. https://iscd.org/learn/official-positions/pediatric-positions/. Accessed 14 Nov 2020.
Ward LM, Weber DR, Munns CF, Högler W, Zemel BS. A contemporary view of the definition and diagnosis of osteoporosis in children and adolescents. J Clin Endocrinol Metab. 2020;105(5):e2088–97.
Collett-Solberg PF, Ambler G, Backeljauw PF, Bidlingmaier M, Biller BMK, Boguszewski MCS, et al. Diagnosis, Genetics, and Therapy of Short Stature in Children: A Growth Hormone Research Society International Perspective. Horm Res Paediatr. 2019;92(1):1–14.
Simm PJ, Biggin A, Zacharin MR, Rodda CP, Tham E, Siafarikas A, et al. Consensus guidelines on the use of bisphosphonate therapy in children and adolescents. J Paediatr Child Health. 2018;54(3):223–33.
Davies JH. A practical approach to problems of Hypercalcaemia. Calcium Bone Disord Child Adolesc. 2009;16:93–114.
Author information
Authors and Affiliations
Contributions
GH initiated the review, AR, DAE and GH contributed equally in literature research, drafting and writing of the manuscript. After critical final review, all authors gave their consent to submit the paper.
Corresponding author
Ethics declarations
Conflict of interest
A. Raimann, D.-A. Ertl and G. Haeusler declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
A. Raimann and D.-A. Ertl are co-first authors.
Rights and permissions
About this article
Cite this article
Raimann, A., Ertl, DA. & Haeusler, G. Bone and growth: basic principles behind rare disorders. Wien Med Wochenschr 171, 86–93 (2021). https://doi.org/10.1007/s10354-020-00809-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10354-020-00809-3