Abstract
Osteoarthritis (OA) is a disabling chronic disease involving the gradual degradation of joint structures causing pain and dysfunction. Magnetic resonance imaging (MRI) has been widely used as a non-invasive tool for assessing OA-related changes. While anatomical MRI is limited to the morphological assessment of the joint structures, quantitative MRI (qMRI) allows for the measurement of biophysical properties of the tissues at the molecular level. Quantitative MRI techniques have been employed to characterize tissues’ structural integrity, biochemical content, and mechanical properties. Their applications extend to studying degenerative alterations, early OA detection, and evaluating therapeutic intervention. This article is a review of qMRI techniques for musculoskeletal tissue evaluation, with a particular emphasis on articular cartilage. The goal is to describe the underlying mechanism and primary limitations of the qMRI parameters, their association with the tissue physiological properties and their potential in detecting tissue degeneration leading to the development of OA with a primary focus on basic and preclinical research studies. Additionally, the review highlights some clinical applications of qMRI, discussing the role of texture-based radiomics and machine learning in advancing OA research.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis (OA) is a multifaceted disorder affecting diarthrodial joints, characterized by the gradual degradation of cartilage, bones, menisci, ligaments, and tendons, accompanied by synovial inflammation arising from diverse biochemical and biomechanical mechanisms [1]. OA stands as one of the most prevalent chronic degenerative diseases, exerting a substantial global burden of disability [2], with its prevalence rising significantly with age and obesity. Projections further suggest an exponential increase in the upcoming decades, placing additional strain on healthcare systems [3]. Presently, disease-modifying drugs remain unavailable, leaving the management of OA confined to symptomatic treatments and joint replacement surgeries in severe cases.
Over the last two decades, various imaging-based methodologies have emerged for early OA detection and monitoring the efficacy of potential therapeutic interventions. Among these, magnetic resonance imaging (MRI) has become a fundamental and widely used tool in preclinical and clinical OA research [4]. While anatomical MRI is frequently employed for the morphological assessment of joint tissues [5], it lacks the capability to detect biochemical and microstructural changes preceding gross morphological alterations. A plethora of quantitative MRI (qMRI) techniques has been proposed, enabling the direct measurement of biophysical tissue properties at the molecular level. Techniques like T2 and T1ρ relaxation time mapping quantify tissues’ magnetic properties to characterize biochemical content, architecture, and functional condition [6, 7]. Other techniques allow for the indirect assessment of specific biochemical components. For instance, delayed gadolinium-enhanced MRI of cartilage (dGEMRIC) [8], sodium (23Na) MRI [9], and glycosaminoglycan (GAG) chemical exchange saturation transfer [10] provide insights into GAG content. Quantitative MRI has been extensively employed in collagenous tissues, particularly articular cartilage, to explore composition, structural integrity, and mechanical properties in normal, artificially degenerated cartilage samples, and animal models of OA [11, 12]. Moreover, it has been proven valuable in evaluating cartilage quality in both preclinical and clinical studies [13], as well as after reparative and regenerative surgical treatment of osteochondral lesions [14].
This paper provides an overview of qMRI techniques for musculoskeletal tissue evaluation (Table 1), including their underlying mechanisms, correlations with physiological properties, potential for detecting degeneration, and primary limitations. Notably, several reviews in the literature mostly present qMRI applications in clinical OA research. The primary focus of this review centers on qMRI applications in basic research and preclinical studies, with a particular emphasis on articular cartilage research. As such, a detailed review of clinical research on OA involving qMRI is beyond the scope of this paper, and interested readers can refer to comprehensive review articles available in the literature for further insights [4, 13, 15, 16].
Native relaxometry of articular cartilage
T2 relaxation time mapping is the most established qMRI technique, extensively investigated in validation studies with chondral samples and animal models of OA. T2 relaxation time mapping quantifies the attenuation of transverse magnetization within the tissue, which is associated with the dipolar interaction of proton spins, and in cartilage is primarily influenced by the restricted motion of water molecules within the extracellular matrix [6]. As a result, T2 is susceptible to molecular and organizational changes in cartilage. Specifically, T2 measurements reflect tissue hydration and provide information on collagen orientation and content. Biochemical assays of ex vivo cartilage have shown that T2 relaxation time correlates positively with water content and negatively with collagen content [17,18,19]. Furthermore, the spatial variation of T2 is closely associated with the three-dimensional arrangement of the collagen fibrils as observed through polarized light microscopy [20,21,22]. This enables the visualization of the typical laminar appearance of cartilage in T2 maps, which reveals the orientation of collagen fibers in different histological zones (Fig. 1) [19, 21]. As an increase in the water content and disruption in the organization of the collagen matrix are among the earliest physiologic changes in cartilage degeneration, T2 mapping serves as a valuable tool for detecting subtle OA-related alterations even before conventional morphological images reveal macroscopic lesions. T2 relaxation time has been reported to increase with cartilage degeneration (Figs. 1, 2) particularly with loss of collagen matrix integrity [23, 24]; therefore, T2 mapping enables assessment of OA progression. Additionally, T2 relaxation times have been found to correlate with cartilage mechanical properties, showing a negative correlation with Young’s modulus and dynamic modulus [22, 24,25,26]. Thus, T2 provides insight into the functional status of the tissue. Several methods have been proposed for T2 mapping [28,29,30,31]. The most common approach involves acquiring multiple images with varying echo times using single-echo or multi-echo spin-echo sequences, followed by fitting an exponential function to the signal intensity of these images. Despite its main strength in sensitivity to collagen fiber orientation, the technique also faces significant challenges, as T2 values are dependent on the tissue's orientation with respect to the direction of the main magnetic field [32, 33]. This phenomenon, known as the magic angle effect, makes the interpretation of T2 maps challenging. Additional drawbacks include long scan times and T2 quantitation dependency on the acquisition method, imaging parameters, MRI scanner, and analysis method used, which are common challenges across quantitative MRI techniques.
Representative T2 and T1ρ maps and histological images showing collagen fibril anisotropy (parallelism index, PI) and PG content (Safranin-O) of osteochondral specimens obtained from tibial plateaus of patients with early OA (OARSI grade 0.9) and advanced OA (OARSI grade 3.7). Prolonged T2 and T1ρ values are depicted on the maps particularly in the superficial cartilage of the patient with advanced OA, which are consistent with collagen disorganization and PG loss, as depicted by the histology. Tri-laminar appearance of cartilage is demonstrated by the T2 and T1ρ at low spin-locking frequencies (≤ 500 kHz). Adapted from [41] and reproduced with permission of John Wiley & Sons, copyright 2023
Histological images including optical density (absorbance) of Safranin-O (a–d) and polarized light microscopy (PLM) (e–h) of articular cartilage reveal decreasing proteoglycan (PG) content and disrupted collagen fibril orientation, respectively, with increasing OARSI grades. The corresponding regions (indicated as rectangles) on the T1ρ (i–l) and T2 maps (m–p) depict elevated relaxation time values, which are consistent with increasing OARSI grades and degenerative changes measured with histology. Reproduced from [23] with permission of John Wiley & Sons, copyright 2023
Another commonly used qMRI technique in OA research is T2* relaxation time mapping, which also serves as an assessment tool for cartilage quality. T2* relaxation is influenced by processes similar to those contributing to T2 relaxation, with an additional impact from the magnetic field inhomogeneity [34]. As local field inhomogeneities reflect tissue structure, T2* mapping has the potential to reveal changes in the cartilage extracellular matrix. Specifically, magnetic susceptibility variations related to collagen fiber alignment within the tissue are captured by T2*, which makes it particularly relevant when imaging highly ordered tissues such as articular cartilage, tendons, or ligaments. Similar to T2, T2* has been reported to be strongly sensitive to collagen orientation and positively correlated with histological grading of cartilage degeneration [33, 35, 36]. Nykänen et al. have reported moderate negative correlations of T2* with GAG content, Young’s modulus, and dynamic modulus [36]. T2* relaxation time can be measured from the exponential decay of the signal using a gradient echo sequence with multiple echo times. Due to the absence of a refocusing pulse, acquisition of T2* mapping is faster than T2 mapping, which facilitates 3D acquisitions. However, it is affected by field inhomogeneity artifacts and, like T2 relaxation, it is prone to the magic angle effect that can potentially lead to misinterpretation of the tissue characteristics or pathology if not properly accounted for [34].
Ultrashort echo time (UTE) enhanced T2* mapping can capture fast-relaxing spins in the deeper and calcified regions of cartilage that are not well-detected by the conventional T2 mapping and may exhibit higher sensitivity to cartilage degeneration [37]. These UTE protocols have echo times about 10–20 times shorter than the shortest echo times generally available on modern clinical MR scanners [38]. The MR signal from highly ordered tissues such as deep and calcified cartilage, cortical bone, and menisci decays very fast so that the echo times used in clinical imaging are unable to produce a signal and so appear dark. The absence of signal from these tissues limits the characterization of their constituents. Williams et al. observed a higher sensitivity of UTE T2* mapping compared to standard T2 mapping in detecting fast relaxing signals within deep cartilage tissue, which implies that UTE T2* mapping potentially could be more effective at capturing specific characteristics or changes in deep cartilage that are not as easily detected by the traditional T2 mapping technique [37]. Liu et al. demonstrated the utility of UTE T2* mapping for visualizing the zone of calcified cartilage in healthy and cadaveric specimens [39]. Moreover, cartilage short T2* components, acquired with UTE acquisition, have been positively correlated with histopathologically confirmed degeneration and alterations in the extracellular matrix organization [40]. However, the advantages of UTE imaging are limited by susceptibility to chemical shift artifacts and off-resonance effects.
The T1 relaxation in a rotating frame (T1ρ relaxation time mapping) has emerged as another valuable method for assessing cartilage quality. In a typical T1ρ relaxation time experiment, following the initial radiofrequency (RF) excitation, the tissue is irradiated with a long, low-amplitude RF pulse, known as the spin-lock pulse. The technique is sensitive to low-frequency macromolecular interactions on the order of the spin-lock pulse frequency [7]. The T1ρ is negatively correlated with the loss of GAG content and variations in fixed-charged density within cartilage tissues [22, 24, 41, 42], which are important indicators of OA-related changes in cartilage. To explain this correlation, it has been suggested that the mechanism dominating T1ρ relaxation in cartilage is the exchange of protons between hydroxyl and amide groups from the GAG chains and bulk water. In early studies, T1ρ has been proposed as a potential alternative for GAG measurement. However, the strength of the correlation between T1ρ and GAG varies with the frequency of the spin-lock pulse, and in the range of frequencies used in biological tissues (< 2 kHz), T1ρ relaxation is also influenced by collagen orientation, and collagen and water content (Fig. 1) [21, 27, 43]. Although the claimed GAG specificity may not hold true, given its relationship with GAG content, tissue hydration, and collagen organization, T1ρ can be used to detect GAG loss, increment in water content and mobility, and loss of cartilage matrix integrity, which are the initial events in the onset of osteoarthritis. Similar to T2, T1ρ values have been shown to increase with cartilage degeneration (Figs. 1, 2) and correlated negatively with cartilage mechanical properties, including equilibrium and dynamic elastic moduli [24, 27, 44]. Typically, multiple images are acquired by varying the duration of the spin-lock RF pulse, and T1ρ values are then estimated by fitting an exponential function to the signal intensity of the images. Despite its potential, T1ρ suffers from similar disadvantages as T2, though the magic angle effect can be mitigated by increasing the spin-lock pulse amplitude. However, this will also lead to increased RF energy deposition within the tissue, which is a concern in T1ρ measurements, especially for in vivo studies as it may result in excessive tissue heating. The RF energy deposition and the magic angle effect can be reduced by employing adiabatic pulses [33].
GAG-specific methods
T1 relaxation time mapping has mostly been used in combination with gadolinium-based contrast agents. According to Donnan's theory, in the delayed Gadolinium Enhanced MRI of Cartilage (dGEMRIC) method the negatively charged gadolinium agent accumulates in higher concentrations in areas of lower glycosaminoglycan (GAG) content, which itself contains abundant negatively charged carboxyl and sulfate groups [8]. In these regions, the paramagnetic properties of the contrast agent induce faster T1 relaxation, enabling the use of T1 mapping for spatial assessment of GAG content. The dGEMRIC technique has been validated ex vivo against histological and biochemical measurements of GAG distribution [8, 23] and has demonstrated sensitivity to cartilage degeneration (Fig. 3) [23, 35, 45], as well as positive correlations with cartilage static and dynamic compressive moduli [26, 46, 47]. The technique, however, is not free from uncertainty. Differences in cartilage thickness and permeability can affect contrast agent diffusion, and equilibrium concentrations may not be reached simultaneously in different cartilage zones [48, 49]. Furthermore, dGEMRIC requires long measurement times [50] as T1 mapping must be repeated twice (with and without contrast agent) for accurate GAG content assessment. Pre-contrast T1 mapping is often omitted in clinical studies to reduce scan time. However, this practice may compromise the accuracy of GAG assessment due to variations in native T1 values.
Representative relaxation time maps (dGEMRIC (T1Gd) and T2) and histological image (Safranin-O) of bovine patellar cartilage sample classified according to cartilage quality index (CQI) as normal (CQI = 0–13), early degeneration (CQI = 14–26) and advanced degeneration (CQI = 27–40). The degenerative changes are reflected with decreased T1Gd, increase T2 and confirmed with decreased intensity of Safranin-O. Cartilage surface is towards the top of the figure. Adapted from [22] and reproduced with permission of John Wiley & Sons, copyright 2023
Glycosaminoglycan chemical exchange saturation transfer (gagCEST) is another MRI technique sensitive to the GAG content in cartilage [10]. During a gagCEST experiment, a relatively long and selective RF pulse is applied at specific frequencies to suppress the magnetization of labile protons bound to GAG. As those protons undergo chemical exchange with water molecules, a partial loss in MRI signal intensity is observed. This effect allows for quantification of GAG content in cartilage. The technique benefits from higher magnetic field strengths (> 3.0 Tesla) (Fig. 4) and has been used in OA research. Notably, gagCEST has been demonstrated to detect changes in artificially degraded cartilage [10]; however, validation studies against histological and biochemical GAG content assessments remain limited [51, 52].
Sodium (23Na) MRI has been used for the measurement of GAG content in articular cartilage [9]. The negatively charged GAG side chains within the extracellular matrix attract positively charged 23Na ions. Under normal physiological condition, these ions distribute proportionally to GAGs, balancing the net charge in cartilage. By assessing sodium concentrations using 23Na MRI, fixed charge density in cartilage can be indirectly measured, providing valuable information about GAG content. Absolute quantification of 23Na concentration is achieved using reference phantoms with known 23Na concentrations (Fig. 5) [53]. This technique directly correlates with GAG content, has demonstrated the ability to differentiate between normal and degenerated cartilage, and has proven to be a useful tool for investigating cartilage maturation [54,55,56]. The technique has certain limitations due to the low sensitivity of 23Na MRI compared to 1H MRI. Consequently, sodium MRI has relatively low resolutions (typically on the order of a few millimeters) and requires long measurement times and dedicated hardware, such as RF amplifiers and dedicated coils optimized for signal detection from sodium nuclei.
Quantification of sodium concentration in bovine articular cartilage using phantoms as reference. a Representative sagittal sodium 3D GRE image of bovine patella and four phantoms with different sodium concentration (from top to bottom: 200, 150, 250, and 300 mM). b Curve plot showing the mean calibration obtained from four different slices of a 3D data set. Circles represent signal intensities and error bars indicate the 95% confidence intervals measured from four phantoms. Reproduced from [55] with permission of Elsevier, copyright 2023
Diffusion imaging and quantitative susceptibility mapping of articular cartilage
Diffusion-weighted imaging (DWI) utilizes gradient pulses to create contrast based on differences in water motion. Diffusing water molecules differ from degenerated to normal cartilage, where water mobility is restricted by the cartilage components. Consequently, DWI becomes a valuable tool to identify damaged cartilage [57]. Diffusion tensor imaging (DTI) has shown sensitivity to both proteoglycan content, which influences mean diffusivity, and collagen orientation, reflected by fractional anisotropy (Fig. 6) [58]. DTI-based tractography enables visualization of collagen fiber architecture (Fig. 7) [59]. Both DWI and DTI are technically challenging and benefit from higher magnetic field strengths.
Representative DTI mean diffusivity map (apparent diffusion coefficient, ADC) and histology sections (Safranin-O and PLM) in a sample obtained from a 45-year-old donor. The maps and the histology sections are presented before (top) and 96 h after treatment with trypsin (bottom). Increased ADC values are depicted after the treatment, which are associated with a decrease in intensity of Safranin-O and reflective of progressive PG loss. The treatment did not change the collage architecture as evidenced by PLM. Adapted from [174] and reproduced with permission of Wolters Kluwer Health, Inc., copyright 2023
Diffusion MRI tractography (a–c) and corresponding PLM images (b–d) of rat joints display collagen fiber orientation in articular cartilage (a, b) and anterior cruciate ligament (c, d). Adapted from [61] and reproduced with permission of John Wiley & Sons, copyright 2023
Quantitative susceptibility mapping (QSM) is a technique that utilizes MRI magnitude and phase data to estimate the spatial distribution of magnetic susceptibility in tissues [60]. MRI phase data are used to measure field perturbations caused by inhomogeneous susceptibility, which is influenced by tissue properties. Association of QSM with collagen fiber orientation and cartilage calcification [36, 61, 62]. Furthermore, QSM correlates positively with proteoglycan content and cartilage mechanical properties [36]. Notably, QSM has been used to detect abnormalities in cartilage canals in goat model of osteochondritis dissecans [63]. Recently, a study used UTE-QSM for simultaneous quantification of susceptibility properties in articular cartilage and cortical bone [64]. However, further research is required to demonstrate the ability of QSM to detect cartilage degeneration.
Quantitative methods for menisci, ligaments, and tendons
Several qMRI techniques used for cartilage have also been applied to assess other cartilaginous tissues. In cases of histologically confirmed meniscal degeneration, elevated T2, T1ρ, and T2* relaxation times have been observed (Fig. 8) [65,66,67,68,69]. Meniscal T2 and T1ρ relaxation times have been associated with water and GAG content, collagen content and organization, and tissue mechanical properties [65, 70]. However, the relationship between these relaxation times and the biochemical content of the meniscus is still not fully understood [65, 68, 70].
Representative normal and diseased menisci images depicting histology sections (hematoxylin and Eosin (a, b) and Safranin-O Fast Green (c, d)), and MRI UTE (e, f), T2* map (g, h), T2 map (i, j) and T1 map (k, l). Decreased intensity of Safranin-O, reflective of PG content, in the diseased meniscus is associated with increased T1, T2, T2* and UTE. Reproduced from [70] under the terms of the CC-BY Creative Commons Attribution 4.0 International License
For ligament assessment, both T2* and T1ρ have shown negative correlations with ligament elastic modulus [71]. In the case of the Achilles tendon, T2 mapping has been linked to histological evaluation and mechanical properties and has been used to assess tendon healing post-treatment [72, 73]. Additionally, 23Na MRI has been shown to positively correlate with GAG content in the Achilles tendon [74].
DTI-based tractography provides visualization of collagen fiber architecture in menisci, tendons and ligaments (Fig. 7) [59, 75, 76]. Furthermore, DTI fractional anisotropy (FA) has been observed to positively correlate with collagen content in the Achilles tendon [73]. DTI has also been used to evaluate the anterior cruciate ligament after reconstruction [77,78,79] and Achilles tendon after surgical repair [80]. While these findings are promising, more extensive validation of these techniques is warranted.
Quantitative methods for bones and muscles
For bone tissue characterization, magnetic field inhomogeneities resulting from susceptibility differences between trabecular and bone marrow are exploited. T2* relaxation time has demonstrated correlations with trabecular bone microstructure, bone mineral density and biomechanical properties [81,82,83,84], as well as cortical bone porosity and mechanical properties [85]. Additionally, QSM has been explored for bone characterization [64, 86] and has shown positive correlations with bone porosity and a negative correlation with mineral density (Fig. 9) [87,88,89].
Representative cortical bone sample obtained from tibial midshaft depicts (a) QSM, (b) uCT slice with the ROIs, (c) uCT-based porosity, and (d) bone mineral density (BMD) maps. Local maxima as shown in the QSM correspond to the regions of high BMD and low porosity. Reproduced from [91] with permission of Elsevier, copyright 2023
Fat fraction (FF) MRI techniques can be employed to quantify fat content within bone marrow and skeletal muscles [90,91,92,93] and have found significant applications primarily in clinical research related to osteoarthritis, osteoporosis, myopathies, and other metabolic disorders. In addition to FF, various qMRI techniques have been used for the noninvasive assessment of muscular tissues. T2 mapping and 23Na MRI have been employed for the characterization of muscle damage [93, 94]. A recent study has shown that FF and T2 mapping are positively correlated with histopathological features in patients with inflammatory myopathies [92]. DTI has been also used to estimate muscle fiber architecture and to visualize microstructural changes due to disease or injury [95, 96]. While these studies have demonstrated the potential of qMRI techniques to identify characteristic features in muscular disorders, their primary application has been in clinical settings. However, research in basic and preclinical domains remains limited, and validation studies are lacking.
Applications, limitations, and future directions
The primary advantage of utilizing qMRI measurements in studies aimed at advancing our understanding of the underlying biology and pathophysiology of cartilage lies in their noninvasive and nondestructive nature. This characteristic makes qMRI ideal for tracking disease progression over time, unlike histological methods. Another notable advantage of qMRI is the possibility to assess large specimens and whole joints. This can be used for the detection of patterns of regional variability in cartilage degeneration within joints, for instance to identify areas more susceptible to deterioration. Additionally, since it is nondestructive and does not require any special tissue preparation, qMRI is compatible with other techniques. Coupling qMRI with mechanical testing and histology, for example, can aid in understanding the impact of mechanical loading on cartilage integrity, and elucidate how cartilage composition influences its response to mechanical loading in both healthy and degenerated tissue. Quantitative MRI techniques, especially T2, T1ρ, T2*, dGEMRIC, and sodium MRI have been successfully applied to assess cartilage degeneration in both in vivo and ex vivo settings, employing different animal models of OA [27, 55, 97,98,99,100,101]. Moreover, qMRI parameters have been widely used in numerous ex vivo studies to assess the quality and function of human osteochondral samples with varying degrees of degeneration [43, 45, 102,103,104,105,106,107]. While the strength of the reported correlations varies, T2, T1ρ and T2* were in general sensitive to alterations in collagen fiber network and hydration of the tissue, whereas dGEMRIC and sodium MRI were specific to cartilage compositional changes, and GAG content. These degenerative changes are key indicators of cartilage tissue integrity and reflective of early OA. By understanding the different sensitivities and specificities of these qMRI techniques, researchers can tailor their imaging protocols to comprehensively assess various aspects of cartilage structure, composition, and health.
As for the heterogeneity in the specificity of qMRI parameters reported in the literature, it can be attributed to several factors. First, qMRI measurements are influenced by magnetic field strengths and acquisition protocols, leading to variations in parameter values across different studies. Second, correlations may vary when using cartilage from different animal species or joints due to inherent differences in tissue properties and composition. Furthermore, discrepancies in correlations may arise depending on the reference methods used to assess cartilage constituents. For instance, correlations between T1ρ values and GAG content may differ when using biochemical assays like dimethylmethylene blue compared to optical densitometry with Safranin O staining for GAG quantification [12, 27]. Finally, comparing qMRI data with histology poses challenges due to differences in spatial resolution and tissue processing. MRI slices are typically larger, ranging from hundreds of microns to millimeters, leading to partial volume effects. In contrast, histological sections are typically a few microns thick, with large gaps between slices, and tissue may undergo distortions during processing, resulting in mismatches between the two modalities.
Quantitative MRI techniques have also been instrumental in assessing cartilage restoration after different repair treatments in preclinical animal studies [108,109,110,111,112]. T2 and dGEMRIC have been shown to effectively differentiate repair tissue from native cartilage after microfracture in a goat model and evaluate the regenerative process following allograft chondrocyte implantation in rabbits [108, 110]. Moreover, a significant positive correlation was found between dGEMRIC and GAG concentration in repair tissue [108, 110]. Chu et al. found differences in UTE T2* texture features between chondral defects treated with bone marrow concentrate with and without concomitant microfracture in an equine model [111]. These findings underscore the ability of qMRI to assess structural and biochemical compositional differences following different cartilage repair procedures, providing a noninvasive means for assessing the efficacy of interventions aimed at enhancing cartilage regeneration. Furthermore, qMRI has proven valuable in characterizing engineered cartilage-like tissue [113,114,115,116,117,118]. For example, in a recent study T2 was used to track the temporal development of fibrocartilage constructs, and it was shown that T2 significantly correlated with their compressive stiffness and coefficient of viscosity [118]. In another study, T2 was demonstrated to correlate with pulsed low-intensity ultrasound-induced changes in cartilage matrix development, indicating its potential for the evaluation of anabolic interventions for engineered tissue [114]. These studies showcase the potential of qMRI in facilitating noninvasive evaluation of engineered cartilage quality in comparison to native tissue, addressing a crucial need in regenerative medicine. In human studies, T2, T1ρ, dGEMRIC and sodium MRI have been applied to evaluate cartilage repair outcomes following bone marrow-stimulating procedures, cartilage grafting techniques, and advanced cell therapy combined with diverse types of biomaterial scaffolds as well as evaluating the quality of regenerated tissue in patients after cartilage repair surgery [14, 109, 119,120,121,122,123,124]. Another study has also shown the potential of T2 mapping for the assessment and monitoring of meniscal healing status after meniscal repair [125].
Notably, preclinical studies have often used ultra-high magnetic field strengths (≥ 7.0 Tesla) to take advantage of the greater signal-to-noise ratio (SNR) and higher spatial resolution (up to tens of microns) compared to the lower field strengths with submillimeter resolution in clinical studies. Higher spatial resolution and SNR enable visualization of fine anatomical details and enhance the sensitivity of qMRI techniques which are particularly valuable for characterizing small structures or subtle changes in tissue composition and structure. Achieving higher spatial resolution often requires long acquisition times which are more feasible in preclinical or ex vivo studies where logistic constraints are less stringent compared to clinical studies involving human participants. Additionally, ex vivo studies involving tissue specimens can be conducted under controlled conditions coupled with histological analyses. Combining high spatial resolution MRI with histological validation allows for direct correlation between imaging findings and tissue microstructure, which can provide a more thorough understanding of tissue biology, disease processes, and treatment effects.
Ex vivo studies have several limitations. Enzymatic degradation procedures used in those studies are frequently nonspecific to particular components and may also not accurately replicate natural degeneration processes. Moreover, human cartilage samples obtained from joint replacement surgery and cadaveric donors are often scarce, and healthy tissue specimens can be particularly limited. Additionally, certain protocols used in ex vivo studies may not be adaptable for in vivo studies involving human subjects. Therefore, the question remains regarding the generalizability of ex vivo findings to the in vivo setting.
In clinical OA research, qMRI techniques have been widely used in both cross-sectional and longitudinal research studies [4]. Among these techniques, T2 and T1ρ mapping of articular cartilage are the most widely used in clinical studies, as their reliability and discriminative power in identifying OA patients and individuals at risk for OA have been demonstrated [126, 127]. Furthermore, incorporating cartilage T2 mapping in clinical MRI protocols has been shown to enhance sensitivity in detecting cartilage lesions [128]. T2 has been applied to large datasets [129] and used to develop OA diagnostic and prognostic prediction models [130,131,132]. T2, T2*, T1ρ, and dGEMRIC have also been employed to study cartilage response to mechanical loading in vivo [133,134,135,136,137]. Despite the vast body of evidence supporting their translational potential as biomarkers for OA, qMRI techniques have not yet become routine in clinical practice, primarily due to the lack of standardization in patient preparation protocols, MRI hardware, image acquisition, and processing methods, all of which can impact measurement outcomes [138,139,140,141,142,143]. To enhance the accuracy of qMRI parameters as biomarkers for monitoring treatment response, further basic research is warranted to gain an in-depth mechanistic understanding of the relationship between biological processes and qMRI. Additionally, it is essential to verify how well the findings obtained at higher magnetic field translate to clinical settings. Therefore, rigorous validation studies are needed to assess the reproducibility and reliability of qMRI measurements across different MRI platforms, acquisition parameters, and patient populations. This will ensure that qMRI biomarkers retain their diagnostic and prognostic value in clinical practice and enable clinicians to make informed treatment decisions based on qMRI-derived information.
The integration of artificial intelligence (AI) tools, particularly deep learning algorithms, may help reduce variability in image acquisition and analysis in MRI studies, including those focused on assessing cartilage health [144, 145]. AI-driven automated segmentation algorithms can accurately delineate cartilage boundaries and automated segmentations of cartilage structures have been reported to closely agree with those performed by expert radiologists and clinicians [144]. These algorithms can learn complex patterns and features from large datasets, enabling them to adapt to variations in imaging protocols and scanner characteristics. By automating the segmentation process, AI tools help ensure standardized and reproducible measurements across different MR scanners, acquisition parameters and subject population; thereby reducing variability and enhancing the reliability and comparability of MRI data obtained from different sources. In the future, deep learning may play a crucial role in image reconstruction to mitigate image acquisition variability. However, this aspect has yet to be explored, as to date deep learning-based image reconstruction algorithms have been applied to shorten scan times in clinical settings [146, 147].
Texture-based radiomics analysis of qMRI has emerged as a valuable approach for detecting changes in the distribution of the cartilage matrix associated with degeneration. The gray-level co-occurrence matrix (GLCM) allows for the extraction of statistical measures of the spatial distribution of pixel values [148], aiding in the identification of textural differences between healthy and pathological tissue, which exhibit significant spatial variation in cartilage relaxation time values compared with normal cartilage [149]. Notably, GLCM texture features derived from cartilage T2 and T1ρ maps have shown enhanced discriminative power in detecting early structural changes [149,150,151,152,153,154,155,156]. Recently, GLCM texture analysis of T2 maps has been used to assess repair tissue and tissue adjacent to the repair site after matrix-associated chondrocyte transplantation [124, 157]. While GLCM-based texture features are commonly used in the context of OA research, local binary pattern-based texture analysis [158] of T2 maps was explored in one study and demonstrated significant differences between OA vs asymptomatic knees [159]. Texture analysis holds the potential to boost qMRI sensitivity to pathological changes in cartilage; however, further validation in basic studies is necessary, and it remains unknown which specific biochemical changes are reflected in different textural features. Furthermore, the reproducibility of texture analysis of qMRI has not been systematically studied and is reliant on factors such as image resolution, acquisition sequence, imaging parameters, and selection of input parameters (e.g., orientation, inter-pixel distance, number of gray levels), as well as the data preprocessing pipeline used.
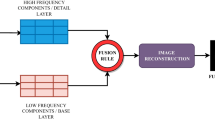
Advancing the sensitivity to degeneration and specificity to cartilage structural properties and biochemical components is achievable through the combination of multiple qMRI techniques [116, 160,161,162]. Recent studies have utilized several qMRI parameters in conjunction with machine learning techniques to estimate proteoglycan and collagen content (Fig. 10) and collagen fiber orientation in cartilage specimens [163, 164]. The findings demonstrated high prediction accuracy and moderate-to-strong correlations between predicted and measured cartilage compositional and structural parameters. These findings hold great promise for future in vivo applications. However, the clinical translation of tools based on measurements of multiple qMRI parameters is complicated by the relatively long acquisition times of conventional sequences for quantitative cartilage mapping. This limitation could potentially be overcome by novel methods enabling rapid measurements of multiple qMRI parameters, such as magnetic resonance fingerprinting [30, 165, 166].
Spatial distributions of collagen (a) and proteoglycan content (b) in a human cartilage specimen: spectroscopic measurements at original resolution (first column) and after downsampling to match MRI resolution (second column); multiparametric qMRI-based predictions with artificial neural network (third column), and multivariate linear model (fourth column). Reproduced from [170] with permission of Elsevier, copyright 2023
In conclusion, qMRI techniques have extended the capabilities of MRI beyond traditional morphological imaging, enabling indirect assessment of cartilage microstructure, biochemical content, and function. Several of these techniques have been extensively validated in cartilage and provide valuable tools in basic and translational research for a deeper understanding of disease mechanisms, cartilage degeneration and repair processes, and for characterizing engineered cartilage-like tissue. Moreover, qMRI holds significant promise in contributing to the development of innovative and novel therapeutic approaches for cartilage-related disorders. The non-destructive nature of qMRI allows for repeated measurements over time, facilitating longitudinal studies to track disease progression and monitor therapeutic interventions.
While T2 and T1ρ mapping lack specificity to biochemical components of cartilage, they have demonstrated the ability to assess the structural integrity of the extracellular matrix and showed their potential in OA diagnostics. On the other hand, promising techniques auch as DTI, sodium MRI, and gagCEST, though presenting technical challenges and requiring higher magnetic field strengths, hold significant potential for precisely assessing cartilage changes in osteoarthritis.
The current evidence supporting qMRI's value in menisci, tendons, and ligaments is relatively limited, necessitating further investigation and validation. Standardization of measurements and analysis protocols remains a challenge. Addressing these challenges, potentially through the integration of artificial intelligence, will be crucial in realizing the full potential of qMRI in clinical practice. Further basic research to better understand the underlying biological processes is an essential step toward enhancing the accuracy and applicability of qMRI parameters as biomarkers for monitoring treatment response.
Texture-based radiomics and combining multiple qMRI techniques offer promising avenues for improving the sensitivity to degeneration and specificity of cartilage structural properties and biochemical components. These approaches hold great potential for providing a more comprehensive and detailed assessment of cartilage, and they are poised to play an increasingly significant role in cartilage research and potentially transforming the diagnosis and treatment of cartilage-related disorders.
Data availability
Not applicable, this is a review paper as such and not involving any data collection/analysis.
References
Loeser RF, Goldring SR, Scanzello CR, Goldring MB (2012) Osteoarthritis: a disease of the joint as an organ. Arthritis Rheum 64:1697–1707
Hunter DJ, Bierma-Zeinstra S (2019) Osteoarthritis. Lancet 393:1745–1759
Long H, Liu Q, Yin H et al (2022) Prevalence trends of site-specific osteoarthritis from 1990 to 2019: findings from the global burden of disease study 2019. Arthritis Rheumatol 74:1172–1183
Juras V, Chang G, Regatte RR (2020) Current status of functional MRI of osteoarthritis for diagnosis and prognosis. Curr Opin Rheumatol 32:102–109
Oei EHG, van Zadelhoff TA, Eijgenraam SM, Klein S, Hirvasniemi J, van der Heijden RA (2021) 3D MRI in osteoarthritis. Semin Musculoskelet Radiol 25:468–479
Mosher TJ, Dardzinski BJ (2004) Cartilage MRI T2 relaxation time mapping: overview and applications. Semin Musculoskelet Radiol 08:355–368
Wang L, Regatte RR (2015) T 1ρ MRI of human musculoskeletal system: T 1ρ MRI of Human MSK System. J Magn Reson Imaging 41:586–600
Bashir A, Gray ML, Hartke J, Burstein D (1999) Nondestructive imaging of human cartilage glycosaminoglycan concentration by MRI. Magn Reson Med 41:857–865
Zbýň Š, Mlynárik V, Juras V, Szomolanyi P, Trattnig S (2014) Sodium MR imaging of articular cartilage pathologies. Curr Radiol Rep 2:41
Ling W, Regatte RR, Navon G, Jerschow A (2008) Assessment of glycosaminoglycan concentration in vivo by chemical exchange-dependent saturation transfer (gagCEST). Proc Natl Acad Sci 105:2266–2270
Kuyinu EL, Narayanan G, Nair LS, Laurencin CT (2016) Animal models of osteoarthritis: classification, update, and measurement of outcomes. J Orthop Surg Res 11:19
Emanuel KS, Kellner LJ, Peters MJM, Haartmans MJJ, Hooijmans MT, Emans PJ (2022) The relation between the biochemical composition of knee articular cartilage and quantitative MRI: a systematic review and meta-analysis. Osteoarthr Cartil 30:650–662
Guermazi A, Alizai H, Crema MD, Trattnig S, Regatte RR, Roemer FW (2015) Compositional MRI techniques for evaluation of cartilage degeneration in osteoarthritis. Osteoarthr Cartil 23:1639–1653
Liu YW, Tran MD, Skalski MR et al (2019) MR imaging of cartilage repair surgery of the knee. Clin Imaging 58:129–139
Eck BL, Yang M, Elias JJ et al (2023) Quantitative MRI for evaluation of musculoskeletal disease: cartilage and muscle composition, joint inflammation, and biomechanics in osteoarthritis. Invest Radiol 58:60–75
Zibetti MVW, Menon RG, de Moura HL, Zhang X, Kijowski R, Regatte RR (2023) Updates on compositional MRI mapping of the cartilage: emerging techniques and applications. J Magn Reson Imaging 58:44–60
Lüsse S, Claassen H, Gehrke T et al (2000) Evaluation of water content by spatially resolved transverse relaxation times of human articular cartilage. Magn Reson Imaging 18:423–430
Liess C, Lüsse S, Karger N, Heller M, Glüer C-C (2002) Detection of changes in cartilage water content using MRI T2-mapping in vivo. Osteoarthr Cartil 10:907–913
Gahunia HK, Lemaire C, Babyn PS, Cross AR, Kessler MJ, Pritzker KP (1995) Osteoarthritis in rhesus macaque knee joint: quantitative magnetic resonance imaging tissue characterization of articular cartilage. J Rheumatol 22:1747–1756
Nieminen MT, Rieppo J, Töyräs J et al (2001) T 2 relaxation reveals spatial collagen architecture in articular cartilage: a comparative quantitative MRI and polarized light microscopic study: T 2 imaging of articular cartilage. Magn Reson Med 46:487–493
Menezes NM, Gray ML, Hartke JR, Burstein D (2004) T2 and T1rho MRI in articular cartilage systems. Magn Reson Med 51:503–509
Mlynárik V, Szomolányi P, Toffanin R, Vittur F, Trattnig S (2004) Transverse relaxation mechanisms in articular cartilage. J Magn Reson 169:300–307
Nissi MJ, Töyräs J, Laasanen MS et al (2004) Proteoglycan and collagen sensitive MRI evaluation of normal and degenerated articular cartilage. J Orthop Res 22:557–564
Nishioka H, Hirose J, Nakamura E et al (2012) T1ρ and T2 mapping reveal the in vivo extracellular matrix of articular cartilage. J Magn Reson Imaging 35:147–155
Nieminen MT, Töyräs J, Laasanen MS, Silvennoinen J, Helminen HJ, Jurvelin JS (2004) Prediction of biomechanical properties of articular cartilage with quantitative magnetic resonance imaging. J Biomech 37:321–328
Lammentausta E, Kiviranta P, Nissi MJ et al (2006) T2 relaxation time and delayed gadolinium-enhanced MRI of cartilage (dGEMRIC) of human patellar cartilage at 1.5 T and 9.4 T: Relationships with tissue mechanical properties. J Orthop Res 24:366–374
Kajabi AW, Casula V, Sarin JK et al (2021) Evaluation of articular cartilage with quantitative MRI in an equine model of post-traumatic osteoarthritis. J Orthop Res 39:63–73
Welsch GH, Scheffler K, Mamisch TC et al (2009) Rapid estimation of cartilage T2 based on double echo at steady state (DESS) with 3 Tesla. Magn Reson Med 62:544–549
Chaudhari AS, Black MS, Eijgenraam S et al (2018) Five-minute knee MRI for simultaneous morphometry and T2 relaxometry of cartilage and meniscus and for semiquantitative radiological assessment using double-echo in steady-state at 3T. J Magn Reson Imaging 47:1328–1341
Cloos MA, Assländer J, Abbas B et al (2019) Rapid radial T1 and T2 mapping of the hip articular cartilage with magnetic resonance fingerprinting: rapid hip cartilage T1 and T2 mapping. J Magn Reson Imaging 50:810–815
Han M, Tibrewala R, Bahroos E, Pedoia V, Majumdar S (2022) Magnetization-prepared spoiled gradient-echo snapshot imaging for efficient measurement of R2–R1ρ in knee cartilage. Magn Reson Med 87:733
Xia Y, Moody JB, Alhadlaq H (2002) Orientational dependence of T2 relaxation in articular cartilage: a microscopic MRI (microMRI) study. Magn Reson Med 48:460–469
Hänninen N, Rautiainen J, Rieppo L, Saarakkala S, Nissi MJ (2017) Orientation anisotropy of quantitative MRI relaxation parameters in ordered tissue. Sci Rep 7:9606
Chavhan GB, Babyn PS, Thomas B, Shroff MM, Haacke EM (2009) Principles, techniques, and applications of T2*-based MR imaging and its special applications. Radiographics 29:1433–1449
Bittersohl B, Hosalkar HS, Miese FR et al (2015) Zonal T2* and T1Gd assessment of knee joint cartilage in various histological grades of cartilage degeneration: an observational in vitro study. BMJ Open 5:e006895
Nykänen O, Sarin JK, Ketola JH et al (2019) T2* and quantitative susceptibility mapping in an equine model of post-traumatic osteoarthritis: assessment of mechanical and structural properties of articular cartilage. Osteoarthr Cartil 27:1481–1490
Williams A, Qian Y, Bear D, Chu CR (2010) Assessing degeneration of human articular cartilage with ultra-short echo time (UTE) T2* mapping. Osteoarthr Cartil 18:539–546
Gold GE, Thedens DR, Pauly JM et al (1998) MR imaging of articular cartilage of the knee: new methods using ultrashort TEs. Am J Roentgenol 170:1223–1226
Liu J, Wei Y, Ma Y-J, Zhu Y-C, Zhou Q, Zhao Y-H (2019) Magnetic resonance imaging of the zone of calcified cartilage in the knee joint using 3-dimensional ultrashort echo time cones sequences. Chin Med J 132:562
Pauli C, Bae WC, Lee M et al (2012) Ultrashort-echo time MR imaging of the patella with bicomponent analysis: correlation with histopathologic and polarized light microscopic findings. Radiology 264:484–493
Regatte RR, Akella SVS, Borthakur A, Reddy R (2003) Proton spin-lock ratio imaging for quantitation of glycosaminoglycans in articular cartilage. J Magn Reson Imaging 17:114–121
Akella SVS, Regatte RR, Wheaton AJ, Borthakur A, Reddy R (2004) Reduction of residual dipolar interaction in cartilage by spin-lock technique. Magn Reson Med 52:1103–1109
Rautiainen J, Nissi MJ, Salo E-N et al (2015) Multiparametric MRI assessment of human articular cartilage degeneration: correlation with quantitative histology and mechanical properties: multiparametric assessment of cartilage degeneration. Magn Reson Med 74:249–259
Wheaton AJ, Dodge GR, Elliott DM, Nicoll SB, Reddy R (2005) Quantification of cartilage biomechanical and biochemical properties via T1rho magnetic resonance imaging. Magn Reson Med 54:1087–1093
Zilkens C, Miese F, Herten M et al (2013) Validity of gradient-echo three-dimensional delayed gadolinium-enhanced magnetic resonance imaging of hip joint cartilage: a histologically controlled study. Eur J Radiol 82:e81-86
Samosky JT, Burstein D, Eric Grimson W, Howe R, Martin S, Gray ML (2005) Spatially-localized correlation of dGEMRIC-measured GAG distribution and mechanical stiffness in the human tibial plateau. J Orthop Res 23:93–101
Juras V, Bittsansky M, Majdisova Z et al (2009) In vitro determination of biomechanical properties of human articular cartilage in osteoarthritis using multi-parametric MRI. J Magn Reson 197:40–47
Li W, Scheidegger R, Wu Y et al (2010) Delayed contrast-enhanced MRI of cartilage: comparison of nonionic and ionic contrast agents. Magn Reson Med 64:1267–1273
Hawezi ZK, Lammentausta E, Svensson J, Dahlberg LE, Tiderius CJ (2011) In vivo transport of Gd-DTPA2− in human knee cartilage assessed by depth-wise dGEMRIC analysis. J Magn Reson Imaging 34:1352–1358
Sur S, Mamisch TC, Hughes T, Kim Y-J (2009) High resolution fast T1 mapping technique for dGEMRIC. J Magn Reson Imaging 30:896–900
Watkins L, Kogan F, Rubin E, Black M, Levenston M, Gold G (2019) Evaluating the relationship between gagCEST MRI and cartilage biochemical composition in juvenile bovine articular cartilage. Osteoarthr Cartil 27:S369
Brinkhof S, Nizak R, Sim S et al (2021) In vivo biochemical assessment of cartilage with gagCEST MRI: correlation with cartilage properties. NMR Biomed 34:e4463
Shapiro EM, Borthakur A, Dandora R, Kriss A, Leigh JS, Reddy R (2000) Sodium visibility and quantitation in intact bovine articular cartilage using high field 23Na MRI and MRS. J Magn Reson 142:24–31
Borthakur A, Shapiro EM, Beers J, Kudchodkar S, Kneeland JB, Reddy R (2000) Sensitivity of MRI to proteoglycan depletion in cartilage: comparison of sodium and proton MRI. Osteoarthr Cartil 8:288–293
Wheaton AJ, Borthakur A, Dodge GR, Kneeland JB, Schumacher HR, Reddy R (2004) Sodium magnetic resonance imaging of proteoglycan depletion in an in vivo model of osteoarthritis. Acad Radiol 11:21–28
Zbýň Š, Ludwig KD, Watkins LE et al (2024) Changes in tissue sodium concentration and sodium relaxation times during the maturation of human knee cartilage: ex vivo 23Na MRI study at 10.5 T. Magn Reson Med 91:1099–1114
Raya JG (2015) Techniques and applications of in vivo diffusion imaging of articular cartilage: techniques of DTI of Articular Cartilage. J Magn Reson Imaging 41:1487–1504
de Visser SK, Bowden JC, Wentrup-Byrne E et al (2008) Anisotropy of collagen fibre alignment in bovine cartilage: comparison of polarised light microscopy and spatially resolved diffusion-tensor measurements. Osteoarthr Cartil 16:689–697
Wang N, Mirando AJ, Cofer G, Qi Y, Hilton MJ, Johnson GA (2020) Characterization complex collagen fiber architecture in knee joint using high-resolution diffusion imaging. Magn Reson Med 84:908–919
Wang Y, Liu T (2015) Quantitative susceptibility mapping (QSM): decoding MRI data for a tissue magnetic biomarker. Magn Reson Med 73:82–101
Wei H, Dibb R, Decker K et al (2017) Investigating magnetic susceptibility of human knee joint at 7 tesla. Magn Reson Med 78:1933–1943
Nykänen O, Rieppo L, Töyräs J et al (2018) Quantitative susceptibility mapping of articular cartilage: ex vivo findings at multiple orientations and following different degradation treatments. Magn Reson Med 80:2702–2716
Wang L, Nissi MJ, Toth F et al (2017) Quantitative susceptibility mapping (QSM) detects abnormalities in cartilage canals in a goat model of preclinical osteochondritis dissecans (OCD). Magn Reson Med 77:1276–1283
Zhang M, Li Z, Wang H et al (2022) Simultaneous quantitative susceptibility mapping of articular cartilage and cortical bone of human knee joint using ultrashort echo time sequences. Front Endocrinol (Lausanne) 13:844351
Nakagawa Y, Sekiya I, Kondo S et al (2016) Relationship between MRI T1rho value and histological findings of intact and radially incised menisci in microminipigs. J Magn Reson Imaging 43:434–445
Nebelung S, Tingart M, Pufe T, Kuhl C, Jahr H, Truhn D (2016) Ex vivo quantitative multiparametric MRI mapping of human meniscus degeneration. Skeletal Radiol 45:1649–1660
Eijgenraam SM, Bovendeert FAT, Verschueren J et al (2019) T2 mapping of the meniscus is a biomarker for early osteoarthritis. Eur Radiol 29:5664–5672
Einarsson E, Svensson J, Folkesson E et al (2020) Relating MR relaxation times of ex vivo meniscus to tissue degeneration through comparison with histopathology. Osteoarthr Cartil Open 2:100061
Bae WC, Tadros AS, Finkenstaedt T, Du J, Statum S, Chung CB (2021) Quantitative magnetic resonance imaging of meniscal pathology ex vivo. Skelet Radiol 50:2405–2414
Son M, Goodman SB, Chen W, Hargreaves BA, Gold GE, Levenston ME (2013) Regional variation in T1ρ and T2 times in osteoarthritic human menisci: correlation with mechanical properties and matrix composition. Osteoarthr Cartil 21:796–805
Jerban S, Hananouchi T, Ma Y et al (2022) Correlation between the elastic modulus of anterior cruciate ligament (ACL) and quantitative ultrashort echo time (UTE) magnetic resonance imaging. J Orthop Res 40:2330–2339
Fukawa T, Yamaguchi S, Watanabe A et al (2015) Quantitative assessment of tendon healing by using MR T2 mapping in a rabbit achilles tendon transection model treated with platelet-rich plasma. Radiology 276:748–755
Zellers JA, Edalati M, Eekhoff JD et al (2022) Quantative MRI predicts tendon mechanical behavior, collagen composition, and organization. J Orthop Res 2:2
Juras V, Apprich S, Pressl C et al (2013) Histological correlation of 7 T multi-parametric MRI performed in ex-vivo Achilles tendon. Eur J Radiol 82:740–744
Wengler K, Tank D, Fukuda T et al (2018) Diffusion tensor imaging of human Achilles tendon by stimulated echo readout-segmented EPI (ste-RS-EPI). Magn Reson Med 80:2464–2474
Shen J, Zhao Q, Qi Y, Cofer G, Johnson GA, Wang N (2022) Tractography of porcine meniscus microstructure using high-resolution diffusion magnetic resonance imaging. Front Endocrinol (Lausanne) 13:876784
Van Dyck P, Froeling M, De Smet E et al (2017) Diffusion tensor imaging of the anterior cruciate ligament graft. J Magn Reson Imaging 46:1423–1432
Van Dyck P, Billiet T, Desbuquoit D et al (2020) Diffusion tensor imaging of the anterior cruciate ligament graft following reconstruction: a longitudinal study. Eur Radiol 30:6673–6684
Liu S, Liu J, Chen W et al (2020) Diffusion tensor imaging for quantitative assessment of anterior cruciate ligament injury grades and graft. J Magn Reson Imaging 52:1475–1484
Sarman H, Atmaca H, Cakir O et al (2015) Assessment of postoperative tendon quality in patients with achilles tendon rupture using diffusion tensor imaging and tendon fiber tracking. J Foot Ankle Surg 54:782–786
Link TM, Majumdar S, Augat P et al (1998) Proximal femur: assessment for osteoporosis with T2* decay characteristics at MR imaging. Radiology 209:531–536
Lammentausta E, Kiviranta P, Töyräs J et al (2007) Quantitative MRI of parallel changes of articular cartilage and underlying trabecular bone in degeneration. Osteoarthr Cartil 15:1149–1157
Wurnig MC, Calcagni M, Kenkel D et al (2014) Characterization of trabecular bone density with ultra-short echo-time MRI at 1.5, 3.0 and 7.0 T—comparison with micro-computed tomography. NMR Biomed 27:1159–1166
Wu H-Z, Zhang X-F, Han S-M et al (2020) Correlation of bone mineral density with MRI T2* values in quantitative analysis of lumbar osteoporosis. Arch Osteoporos 15:18
Bae WC, Chen PC, Chung CB, Masuda K, D’Lima D, Du J (2012) Quantitative ultrashort echo time (UTE) MRI of human cortical bone: correlation with porosity and biomechanical properties. J Bone Miner Res 27:848–857
Dimov AV, Liu Z, Spincemaille P, Prince MR, Du J, Wang Y (2018) Bone quantitative susceptibility mapping using a chemical species–specific signal model with ultrashort and conventional echo data. Magn Reson Med 79:121–128
Chen Y, Guo Y, Zhang X, Mei Y, Feng Y, Zhang X (2018) Bone susceptibility mapping with MRI is an alternative and reliable biomarker of osteoporosis in postmenopausal women. Eur Radiol 28:5027–5034
Diefenbach MN, Meineke J, Ruschke S, Baum T, Gersing A, Karampinos DC (2019) On the sensitivity of quantitative susceptibility mapping for measuring trabecular bone density. Magn Reson Med 81:1739–1754
Jerban S, Lu X, Jang H et al (2019) Significant correlations between human cortical bone mineral density and quantitative susceptibility mapping (QSM) obtained with 3D Cones ultrashort echo time magnetic resonance imaging (UTE-MRI). Magn Reson Imaging 62:104–110
Gee CS, Nguyen JTK, Marquez CJ et al (2015) Validation of bone marrow fat quantification in the presence of trabecular bone using MRI. J Magn Reson Imaging 42:539–544
Bray TJP, Bainbridge A, Punwani S, Ioannou Y, Hall-Craggs MA (2018) Simultaneous quantification of bone edema/adiposity and structure in inflamed bone using chemical shift-encoded MRI in spondyloarthritis. Magn Reson Med 79:1031
Wang F, Fang S, Li J et al (2023) Correlation analysis of quantitative MRI measurements of thigh muscles with histopathology in patients with idiopathic inflammatory myopathy. Eur Radiol Exp 7:51
Engelke K, Chaudry O, Gast L et al (2023) Magnetic resonance imaging techniques for the quantitative analysis of skeletal muscle: state of the art. J Orthopaed Transl 42:57–72
Weber M-A, Nagel AM, Jurkat-Rott K, Lehmann-Horn F (2011) Sodium (23Na) MRI detects elevated muscular sodium concentration in Duchenne muscular dystrophy. Neurology 77:2017–2024
Damon BM, Ding Z, Anderson AW, Freyer AS, Gore JC (2002) Validation of diffusion tensor MRI-based muscle fiber tracking. Magn Reson Med 48:97–104
Oudeman J, Nederveen AJ, Strijkers GJ, Maas M, Luijten PR, Froeling M (2016) Techniques and applications of skeletal muscle diffusion tensor imaging: a review. J Magn Reson Imaging 43:773–788
Rautiainen J, Nissi MJ, Liimatainen T, Herzog W, Korhonen RK, Nieminen MT (2014) Adiabatic rotating frame relaxation of MRI reveals early cartilage degeneration in a rabbit model of anterior cruciate ligament transection. Osteoarthr Cartil 22:1444–1452
Wei B, Zong M, Yan C et al (2015) Use of quantitative MRI for the detection of progressive cartilage degeneration in a mini-pig model of osteoarthritis caused by anterior cruciate ligament transection. J Magn Reson Imaging 42:1032–1038
Tóth F, David FH, LaFond E, Wang L, Ellermann JM, Carlson CS (2017) In vivo visualization using MRI T2 mapping of induced osteochondrosis and osteochondritis dissecans lesions in goats undergoing controlled exercise. J Orthop Res 35:868–875
Mittelstaedt D, Kahn D, Xia Y (2018) Detection of early osteoarthritis in canine knee joints 3 weeks post ACL transection by microscopic MRI and biomechanical measurement. J Orthop Surg (Hong Kong) 26:2309499018778357
Armstrong AR, Bhave S, Buko EO et al (2022) Quantitative T2 and T1ρ mapping are sensitive to ischemic injury to the epiphyseal cartilage in an in vivo piglet model of Legg-Calvé-Perthes disease. Osteoarthr Cartil 30:1244–1253
Li X, Cheng J, Lin K et al (2011) Quantitative MRI using T1ρ and T2 in human osteoarthritic cartilage specimens: correlation with biochemical measurements and histology. Magn Reson Imaging 29:324–334
Nebelung S, Brill N, Tingart M et al (2016) Quantitative OCT and MRI biomarkers for the differentiation of cartilage degeneration. Skeletal Radiol 45:505–516
Linka K, Itskov M, Truhn D, Nebelung S, Thüring J (2017) T2 MR imaging vs computational modeling of human articular cartilage tissue functionality. J Mech Behav Biomed Mater 74:477–487
Truhn D, Sondern B, Oehrl S et al (2019) Differentiation of human cartilage degeneration by functional MRI mapping—an ex vivo study. Eur Radiol 29:6671–6681
Hafner T, Post M, Said O et al (2020) Identifying the imaging correlates of cartilage functionality based on quantitative MRI mapping—the collagenase exposure model. Acta Biomater 117:310–321
Grondin MM, Liu F, Vignos MF et al (2021) Bi-component T2 mapping correlates with articular cartilage material properties. J Biomech 116:110215
Watanabe A, Boesch C, Anderson SE, Brehm W, Mainil Varlet P (2009) Ability of dGEMRIC and T2 mapping to evaluate cartilage repair after microfracture: a goat study. Osteoarthr Cartil 17:1341–1349
Nieminen MT, Nissi MJ, Mattila L, Kiviranta I (2012) Evaluation of chondral repair using quantitative MRI. J Magn Reson Imaging 36:1287–1299
Endo J, Watanabe A, Sasho T et al (2015) Utility of T2 mapping and dGEMRIC for evaluation of cartilage repair after allograft chondrocyte implantation in a rabbit model. Osteoarthr Cartil 23:280–288
Chu CR, Fortier LA, Williams A et al (2018) Minimally manipulated bone marrow concentrate compared with microfracture treatment of full-thickness chondral defects: a one-year study in an equine model. J Bone Joint Surg Am 100:138–146
SantAnna JPC, Faria RR, Assad IP et al (2022) Tissue engineering and cell therapy for cartilage repair: preclinical evaluation methods. Tissue Eng Part C Methods 28:73–82
Novotny JE, Turka CM, Jeong C et al (2006) Biomechanical and magnetic resonance characteristics of a cartilage-like equivalent generated in a suspension culture. Tissue Eng 12:2755–2764
Irrechukwu ON, Lin P-C, Fritton K, Doty S, Pleshko N, Spencer RG (2011) Magnetic resonance studies of macromolecular content in engineered cartilage treated with pulsed low-intensity ultrasound. Tissue Eng Part A 17:407–415
Irrechukwu ON, Reiter DA, Lin P-C, Roque RA, Fishbein KW, Spencer RG (2012) Characterization of engineered cartilage constructs using multiexponential T2 relaxation analysis and support vector regression. Tissue Eng Part C Methods 18:433–443
Reiter DA, Irrechukwu O, Lin P-C et al (2012) Improved MR-based characterization of engineered cartilage using multiexponential T2 relaxation and multivariate analysis. NMR Biomed 25:476–488
Kotecha M, Klatt D, Magin RL (2013) Monitoring cartilage tissue engineering using magnetic resonance spectroscopy, imaging, and elastography. Tissue Eng Part B Rev 19:470
Hadidi P, Cissell DD, Hu JC, Athanasiou KA (2017) Temporal development of near-native functional properties and correlations with qMRI in self-assembling fibrocartilage treated with exogenous lysyl oxidase homolog 2. Acta Biomater 64:29–40
Theologis AA, Schairer WW, Carballido-Gamio J, Majumdar S, Li X, Ma CB (2012) Longitudinal analysis of T1ρ and T2 quantitative MRI of knee cartilage laminar organization following microfracture surgery. Knee 19:652–657
Guermazi A, Roemer FW, Alizai H et al (2015) State of the art: MR imaging after knee cartilage repair surgery. Radiology 277:23–43
Trattnig S, Ohel K, Mlynarik V, Juras V, Zbyn S, Korner A (2015) Morphological and compositional monitoring of a new cell-free cartilage repair hydrogel technology—GelrinC by MR using semi-quantitative MOCART scoring and quantitative T2 index and new zonal T2 index calculation. Osteoarthr Cartil 23:2224–2232
Zbýň Š, Mlynárik V, Juras V, Szomolanyi P, Trattnig S (2016) Evaluation of cartilage repair and osteoarthritis with sodium MRI: evaluation of cartilage repair and osteoarthritis with sodium MRI. NMR Biomed 29:206–215
Xu X, Gao J, Liu S et al (2021) Magnetic resonance imaging for non-invasive clinical evaluation of normal and regenerated cartilage. Regen Biomater 8:38
Janacova V, Szomolanyi P, Kirner A, Trattnig S, Juras V (2022) Adjacent cartilage tissue structure after successful transplantation: a quantitative MRI study using T2 mapping and texture analysis. Eur Radiol 32:8364–8375
Yamasaki S, Hashimoto Y, Nishida Y et al (2020) Assessment of meniscal healing status by magnetic resonance imaging T2 mapping after meniscal repair. Am J Sports Med 48:853–860
MacKay JW, Low SBL, Smith TO, Toms AP, McCaskie AW, Gilbert FJ (2018) Systematic review and meta-analysis of the reliability and discriminative validity of cartilage compositional MRI in knee osteoarthritis. Osteoarthritis Cartilage 26:1140–1152
Atkinson HF, Birmingham TB, Moyer RF et al (2019) MRI T2 and T1ρ relaxation in patients at risk for knee osteoarthritis: a systematic review and meta-analysis. BMC Musculoskelet Disord 20:182
Kijowski R, Blankenbaker DG, Munoz Del Rio A, Baer GS, Graf BK (2013) Evaluation of the articular cartilage of the knee joint: value of adding a T2 mapping sequence to a routine MR imaging protocol. Radiology 267:503–513
Razmjoo A, Caliva F, Lee J et al (2021) T2 analysis of the entire osteoarthritis initiative dataset. J Orthop Res 39:74–85
Joseph GB, McCulloch CE, Nevitt MC et al (2018) Tool for osteoarthritis risk prediction (TOARP) over 8 years using baseline clinical data, X-ray, and MRI: data from the osteoarthritis initiative. J Magn Reson Imaging 47:1517–1526
Joseph GB, McCulloch CE, Nevitt MC, Link TM, Sohn JH (2022) Machine learning to predict incident radiographic knee osteoarthritis over 8 Years using combined MR imaging features, demographics, and clinical factors: data from the Osteoarthritis Initiative. Osteoarthr Cartil 30:270–279
Pedoia V, Lee J, Norman B, Link TM, Majumdar S (2019) Diagnosing osteoarthritis from T2 maps using deep learning: an analysis of the entire Osteoarthritis Initiative baseline cohort. Osteoarthr Cartil 27:1002–1010
Nishii T, Kuroda K, Matsuoka Y, Sahara T, Yoshikawa H (2008) Change in knee cartilage T2 in response to mechanical loading. J Magn Reson Imaging 28:175–180
Mayerhoefer ME, Welsch GH, Mamisch TC et al (2010) The in vivo effects of unloading and compression on T1-Gd (dGEMRIC) relaxation times in healthy articular knee cartilage at 3.0 Tesla. Eur Radiol 20:443–449
Subburaj K, Souza RB, Stehling C et al (2012) Association of MR relaxation and cartilage deformation in knee osteoarthritis. J Orthop Res 30:919–926
Souza RB, Kumar D, Calixto N et al (2014) Response of knee cartilage T1rho and T2 relaxation times to in vivo mechanical loading in individuals with and without knee osteoarthritis. Osteoarthr Cartil 22:1367–1376
Szomolányi P, Röhrich S, Frollo I et al (2017) Evaluation of compression properties of human knee cartilage—in-vivo study at 7T MRI. In: 2017 11th International Conference on Measurement 2:185–188.
Koff MF, Amrami KK, Felmlee JP, Kaufman KR (2008) Bias of cartilage T2 values related to method of calculation. Magn Reson Imaging 26:1236–1243
Chang G, Wiggins GC, Xia D et al (2012) Comparison of a 28-channel receive array coil and quadrature volume coil for morphologic imaging and T2 mapping of knee cartilage at 7T. J Magn Reson Imaging 35:441–448
Li X, Wyatt C, Rivoire J et al (2014) Simultaneous acquisition of T1ρ and T2 quantification in knee cartilage: repeatability and diurnal variation. J Magn Reson Imaging 39:1287–1293
Li X, Pedoia V, Kumar D et al (2015) Cartilage T 1ρ and T 2 relaxation times: longitudinal reproducibility and variations using different coils, MR systems and sites. Osteoarthr Cartil 23:2214–2223
Mars M, Chelli M, Tbini Z, Ladeb F, Gharbi S (2018) MRI T2 mapping of knee articular cartilage using different acquisition sequences and calculation methods at 1.5 tesla. Med Princ Pract 27:443–450
Verschueren J, Eijgenraam SM, Klein S et al (2021) T2 mapping of healthy knee cartilage: multicenter multivendor reproducibility. Quant Imaging Med Surg 11:1247–1255
Thomas KA, Krzemiński D, Kidziński Ł et al (2021) Open source software for automatic subregional assessment of knee cartilage degradation using quantitative T2 relaxometry and deep learning. Cartilage 13(1):747S-756S
Schmidt AM, Desai AD, Watkins LE et al (2022) Generalizability of deep learning segmentation algorithms for automated assessment of cartilage morphology and MRI relaxometry. J Magn Reson Imaging 2:2
Johnson PM, Lin DJ, Zbontar J et al (2023) Deep learning reconstruction enables prospectively accelerated clinical knee MRI. Radiology 307:e220425
Bian W, Jang A, Liu F (2024) Improving quantitative MRI using self-supervised deep learning with model reinforcement: demonstration for rapid T1 mapping. Magn Reson Med 92:98–111
Haralick RM, Shanmugam K, Dinstein I (1973) Textural features for image classification. IEEE Trans Syst Man Cybern 3:610–621
Li X, Pai A, Blumenkrantz G et al (2009) Spatial distribution and relationship of T 1ρ and T 2 relaxation times in knee cartilage with osteoarthritis. Magn Reson Med 61:1310–1318
Blumenkrantz G, Stahl R, Carballido-Gamio J et al (2008) The feasibility of characterizing the spatial distribution of cartilage T2 using texture analysis. Osteoarthr Cartil 16:584–590
Carballido-Gamio J, Stahl R, Blumenkrantz G, Romero A, Majumdar S, Link TM (2009) Spatial analysis of magnetic resonance T1- and T2 relaxation times improves classification between subjects with and without osteoarthritis. Med Phys 36:9
Carballido-Gamio J, Joseph GB, Lynch JA, Link TM, Majumdar S (2011) Longitudinal analysis of MRI T 2 knee cartilage laminar organization in a subset of patients from the osteoarthritis initiative: a texture approach: OAI texture laminar analysis of T 2 cartilage. Magn Reson Med 65:1184–1194
Joseph GB, Baum T, Carballido-Gamio J et al (2011) Texture analysis of cartilage T2 maps: individuals with risk factors for OA have higher and more heterogeneous knee cartilage MR T2 compared to normal controls—data from the osteoarthritis initiative. Arthritis Res Ther 13:R153
Baum T, Joseph GB, Nardo L et al (2013) Correlation of magnetic resonance imaging-based knee cartilage T2 measurements and focal knee lesions with body mass index: thirty-six-month followup data from a longitudinal, observational multicenter study. Arthritis Care Res 65:23–33
Schooler J, Kumar D, Nardo L et al (2014) Longitudinal evaluation of T1ρ and T2 spatial distribution in osteoarthritic and healthy medial knee cartilage. Osteoarthritis Cartilage 22:51–62
Peuna A, Hekkala J, Haapea M et al (2018) Variable angle gray level co-occurrence matrix analysis of T2 relaxation time maps reveals degenerative changes of cartilage in knee osteoarthritis: Oulu knee osteoarthritis study. J Magn Reson Imaging 47:1316–1327
Juras V, Szomolanyi P, Janáčová V, Kirner A, Angele P, Trattnig S (2021) Differentiation of cartilage repair techniques using texture analysis from T2 maps. Cartilage 13(1):718–728
Ojala T, Pietikäinen M, Harwood D (1996) A comparative study of texture measures with classification based on featured distributions. Pattern Recogn 29:51–59
Peuna A, Thevenot J, Saarakkala S, Nieminen MT, Lammentausta E (2021) Machine learning classification on texture analyzed T2 maps of osteoarthritic cartilage: oulu knee osteoarthritis study. Osteoarthr Cartil 29:859–869
Pc L, Da R, Rg S (2009) Classification of degraded cartilage through multiparametric MRI analysis. J Magn Resonan 201:2
Lin P-C, Irrechukwu O, Roque R, Hancock B, Fishbein KW, Spencer RG (2012) Multivariate analysis of cartilage degradation using the support vector machine algorithm. Magn Reson Med 67:1815–1826
Griebel AJ, Trippel SB, Emery NC, Neu CP (2014) Noninvasive assessment of osteoarthritis severity in human explants by multicontrast MRI. Magn Reson Med 71:807–814
Linka K, Thüring J, Rieppo L et al (2021) Machine learning-augmented and microspectroscopy-informed multiparametric MRI for the non-invasive prediction of articular cartilage composition. Osteoarthr Cartil 29:592–602
Mirmojarabian SA, Kajabi AW, Ketola JHJ et al (2022) Machine learning prediction of collagen fiber orientation and proteoglycan content from multiparametric quantitative MRI in articular cartilage. J Magn Reson Imaging 2:2
Sharafi A, Zibetti MVW, Chang G, Cloos M, Regatte RR (2022) 3D magnetic resonance fingerprinting for rapid simultaneous T1, T2, and T1ρ volumetric mapping of human articular cartilage at 3 T. NMR Biomed 35:e4800
Ma D, Gulani V, Seiberlich N et al (2013) Magnetic resonance fingerprinting. Nature 495:187–192
Acknowledgements
The authors would like to thank the support from the Finnish Cultural Foundation, the National Institutes of Health, including the National Institute of Biomedical Imaging and Bioengineering (P41 EB027061) and R01EB034575, and the Research Council of Finland (Flagship of Advanced Mathematics for Sensing Imaging and Modelling grant 359186).
Funding
Open Access funding provided by University of Oulu (including Oulu University Hospital).
Author information
Authors and Affiliations
Contributions
CV and KAW contributed to the study conception, literature search, interpretation of the data, drafting and critical revision of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest relevant to this article to disclose.
Ethical standards
This article does not involve any new studies with human participants or animals performed by any of the authors. All data and materials referenced in this review comply with the ethical guidelines and policies of their respective sources.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Casula, V., Kajabi, A.W. Quantitative MRI methods for the assessment of structure, composition, and function of musculoskeletal tissues in basic research and preclinical applications. Magn Reson Mater Phy (2024). https://doi.org/10.1007/s10334-024-01174-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10334-024-01174-7