Abstract
Objectives
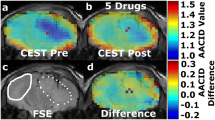
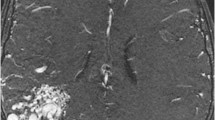
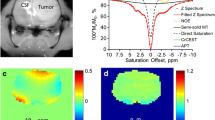
We demonstrated a novel metabolic method based on sequential administration of 5-aminolevulinic acid (ALA) and iron supplement, and ferric ammonium citrate (FAC), for glioblastoma multiforme (GBM) detection using R2’ and quantitative susceptibility mapping (QSM).
Materials and methods
Intra-cellular iron accumulation in glioblastoma cells treated with ALA and/or FAC was measured. Cell phantoms containing glioblastoma cells and Wistar rats bearing C6 glioblastoma were imaged using a 3 T MRI scanner after sequential administration of ALA and FAC. The relaxivity and QSM analysis were performed on the images.
Results
The intra-cellular iron deposition was significantly higher in the glioma cells with sequential treatment of ALA and FAC for 6 h compared to those treated with the controls. The relaxivity and magnetic susceptibility values of the glioblastoma cells and rat brain tumors treated with ALA + FAC (115 ± 5 s-1 for R2’, and 0.1 ± 0.02 ppm for magnetic susceptibility) were significantly higher than those treated with the controls (55 ± 18 (FAC), 45 ± 15 (ALA) s-1 for R2’, p < 0.05, and 0.03 ± 0.03 (FAC), 0.02 ± 0.02 (ALA) ppm for magnetic susceptibility, p < 0.05).
Discussion
Sequential administration of ALA and iron supplements increases the iron deposition in glioblastoma cells, enabling clinical 3 T MRI to detect GBM using R2’ or QSM.






Similar content being viewed by others
References
Rahmat R, Saednia K, Khani MRHH, Rahmati M, Jena R, Price SJ (2020) Multi-scale segmentation in GBM treatment using diffusion tensor imaging. Comput Biol Med 103815
Lamborn KR, Chang SM, Prados MD (2004) Prognostic factors for survival of patients with glioblastoma: recursive partitioning analysis. Neuro Oncol 6(3):227–235
Baykara M, Ozcan M, Bilgen M, Kelestimur H (2021) Interference of gadolinium dechelated from MR contrast agents by calcium signaling in neuronal cells of GnRH. J Cell Physiol 236(3):2139–2143
Xu X, Yadav NN, Knutsson L, Hua J, Kalyani R, Hall E, Laterra J, Blakeley J, Strowd R, Pomper M (2015) Dynamic glucose-enhanced (DGE) MRI: translation to human scanning and first results in glioma patients. Tomography 1(2):105
Riyahi-Alam N, Behrouzkia Z, Seifalian A, Haghgoo S (2010) SU-GG-I-149: Positive MRI Contrast Agent Based on Gd2O3 Nanoparticles for Cell Tracking. Med Phys 37(6Part5):3135–3136
Heydarnezhadi S, Riyahi-Alam N, Haghgoo S, Gorji E, Ghenaati H, Rafiei B (2015) In Vitro and In Vivo Studies Glycosylated Gadolinum Nanomagnetic Particleas (GD-DTPA-DG) as New Potential Metabolic Contrast Agent in MMRI. World Congress on Medical Physics and Biomedical Engineering, June 7–12, 2015, Toronto, Canada. Springer, New York, pp 126–131
Mortezazadeh T, Gholibegloo E, Alam NR, Dehghani S, Haghgoo S, Ghanaati H, Khoobi M (2019) Gadolinium (III) oxide nanoparticles coated with folic acid-functionalized poly (β-cyclodextrin-co-pentetic acid) as a biocompatible targeted nano-contrast agent for cancer diagnostic: in vitro and in vivo studies. Magn Reson Mater Phy 32(4):487–500
Kim J-h, Chang K-H, Na D, Song I, Kwon B, Han M, Kim K (2006) 3T 1H-MR spectroscopy in grading of cerebral gliomas: comparison of short and intermediate echo time sequences. Am J Neuroradiol 27(7):1412–1418
Kang Y, Choi SH, Kim Y-J, Kim KG, Sohn C-H, Kim J-H, Yun TJ, Chang K-H (2011) Gliomas: histogram analysis of apparent diffusion coefficient maps with standard-or high-b-value diffusion-weighted MR imaging—correlation with tumor grade. Radiology 261(3):882–890
Roessler K, Gatterbauer B, Becherer A, Paul M, Kletter K, Prayer D, Hoeftberger R, Hainfellner J, Asenbaum S, Knosp E (2007) Surgical target selection in cerebral glioma surgery: linking methionine (MET) PET image fusion and neuronavigation. min-Minim Invasive Neurosurg 50(05):273–280
Widhalm G, Wolfsberger S, Minchev G, Woehrer A, Krssak M, Czech T, Prayer D, Asenbaum S, Hainfellner JA, Knosp E (2010) 5-Aminolevulinic acid is a promising marker for detection of anaplastic foci in diffusely infiltrating gliomas with nonsignificant contrast enhancement. Cancer Interdiscip Int J Am Cancer Soc 116(6):1545–1552
Hefti M, Siegner A, Looser H (2008) 5-aminolevulinic acid induced protoporphyrin IX fluorescence in high-grade glioma surgery. Swiss Med Wkly 138 (1112)
Weinberg SE, Chandel NS (2015) Targeting mitochondria metabolism for cancer therapy. Nat Chem Biol 11(1):9
Layer G, Reichelt J, Jahn D, Heinz DW (2010) Structure and function of enzymes in heme biosynthesis. Protein Sci 19(6):1137–1161
Ebrahimpour A, Riahialam N, Khoobi M (2020) The potential of 5-aminolevulinic acid as a contrast agent in MR imaging: challenges and opportunities. J Sci Islam Repub Iran
Cho HR, Kim DH, Kim D, Doble P, Bishop D, Hare D, Park C-K, Moon WK, Han MH, Choi SH (2014) Malignant glioma: MR imaging by using 5-aminolevulinic acid in an animal model. Radiology 272(3):720–730
Peng Q, Warloe T, Berg K, Moan J, Kongshaug M, Giercksky KE, Nesland JM (1997) 5-Aminolevulinic acid-based photodynamic therapy: clinical research and future challenges. Cancer Interdiscip Int J Am Cancer Soc 79(12):2282–2308
Ates S, Deistung A, Schneider R, Prehn C, Lukas C, Reichenbach JR, Schneider-Gold C, Bellenberg B (2019) Characterization of iron accumulation in deep grey matter in Myotonic Dystrophy type 1 and 2 using quantitative susceptibility mapping and R2* relaxometry: a magnetic resonance imaging study at 3 Tesla. Front Neurol 10:1320
Wood JC, Enriquez C, Ghugre N, Tyzka JM, Carson S, Nelson MD, Coates TD (2005) MRI R2 and R2* mapping accurately estimates hepatic iron concentration in transfusion-dependent thalassemia and sickle cell disease patients. Blood 106(4):1460–1465
Li J, Chang S, Liu T, Wang Q, Cui D, Chen X, Jin M, Wang B, Pei M, Wisnieff C (2012) Reducing the object orientation dependence of susceptibility effects in gradient echo MRI through quantitative susceptibility mapping. Magn Reson Med 68(5):1563–1569
Ulrich X, Yablonskiy DA (2016) Separation of cellular and BOLD contributions to T2* signal relaxation. Magn Reson Med 75(2):606–615
Deistung A, Schweser F, Reichenbach JR (2017) Overview of quantitative susceptibility mapping. NMR Biomed 30(4):e3569
Sharma SD, Fischer R, Schoennagel BP, Nielsen P, Kooijman H, Yamamura J, Adam G, Bannas P, Hernando D, Reeder SB (2017) MRI-based quantitative susceptibility mapping (QSM) and R2* mapping of liver iron overload: comparison with SQUID-based biomagnetic liver susceptometry. Magn Reson Med 78(1):264–270
Kim H-G, Park S, Rhee HY, Lee KM, Ryu C-W, Rhee SJ, Lee SY, Wang Y, Jahng G-H (2017) Quantitative susceptibility mapping to evaluate the early stage of Alzheimer’s disease. NeuroImage Clin 16:429–438
Chary K, Nissi MJ, Nykänen O, Manninen E, Rey RI, Shmueli K, Sierra A, Gröhn O (2021) Quantitative susceptibility mapping of the rat brain after traumatic brain injury. NMR Biomed 34(2):e4438
Jones PS, Yekula A, Lansbury E, Small JL, Ayinon C, Mordecai S, Hochberg FH, Tigges J, Delcuze B, Charest A (2019) Characterization of plasma-derived protoporphyrin-IX-positive extracellular vesicles following 5-ALA use in patients with malignant glioma. EBioMedicine 48:23–35
Kim HS, Cho HR, Choi SH, Woo JS, Moon WK (2010) In vivo imaging of tumor transduced with bimodal lentiviral vector encoding human ferritin and green fluorescent protein on a 1.5 T clinical magnetic resonance scanner. Cancer Res 70(18):7315–7324
He T, Gatehouse PD, Smith GC, Mohiaddin RH, Pennell DJ, Firmin DN (2008) Myocardial T measurements in iron-overloaded thalassemia: An in vivo study to investigate optimal methods of quantification. Magn Reson Med 60(5):1082–1089
Li W, Wu B, Liu C (2011) Quantitative susceptibility mapping of human brain reflects spatial variation in tissue composition. Neuroimage 55(4):1645–1656
Haacke EM, Liu S, Buch S, Zheng W, Wu D, Ye Y (2015) Quantitative susceptibility mapping: current status and future directions. Magn Reson Imaging 33(1):1–25
Gorman AW, Deh KM, Schwiedrzik CM, White JR, Groman EV, Fisher CA, Gillen KM, Spincemaille P, Rasmussen S, Prince MR (2018) Brain iron distribution after multiple doses of ultra-small superparamagnetic iron oxide particles in rats. Comp Med 68(2):139–147
Ogura S-i, Maruyama K, Hagiya Y, Sugiyama Y, Tsuchiya K, Takahashi K, Abe F, Tabata K, Okura I, Nakajima M (2011) The effect of 5-aminolevulinic acid on cytochrome c oxidase activity in mouse liver. BMC Res Notes 4(1):1–4
Saito K, Fujiwara T, Ota U, Hatta S, Ichikawa S, Kobayashi M, Okitsu Y, Fukuhara N, Onishi Y, Ishizuka M (2017) Dynamics of absorption, metabolism, and excretion of 5-aminolevulinic acid in human intestinal Caco-2 cells. Biochem Biophys Rep 11:105–111
Fujiwara T, Okamoto K, Niikuni R, Takahashi K, Okitsu Y, Fukuhara N, Onishi Y, Ishizawa K, Ichinohasama R, Nakamura Y (2014) Effect of 5-aminolevulinic acid on erythropoiesis: a preclinical in vitro characterization for the treatment of congenital sideroblastic anemia. Biochem Biophys Res Commun 454(1):102–108
Yoshida T, Migita CT (2000) Mechanism of heme degradation by heme oxygenase. J Inorg Biochem 82(1–4):33–41
Hagiya Y, Adachi T, Ogura S-I, An R, Tamura A, Nakagawa H, Okura I, Mochizuki T, Ishikawa T (2008) Nrf2-dependent induction of human ABC transporter ABCG2 and heme oxygenase-1 in HepG2 cells by photoactivation of porphyrins: biochemical implications for cancer cell response to photodynamic therapy. J Exp Ther Oncol 7(2)
Chen Y-H, Yet S-F, Perrella MA (2003) Role of heme oxygenase-1 in the regulation of blood pressure and cardiac function. Exp Biol Med 228(5):447–453
Nishio Y, Fujino M, Zhao M, Ishii T, Ishizuka M, Ito H, Takahashi K, Abe F, Nakajima M, Tanaka T (2014) 5-Aminolevulinic acid combined with ferrous iron enhances the expression of heme oxygenase-1. Int Immunopharmacol 19(2):300–307
Eisenstein RS, Garcia-Mayol D, Pettingell W, Munro HN (1991) Regulation of ferritin and heme oxygenase synthesis in rat fibroblasts by different forms of iron. Proc Natl Acad Sci 88(3):688–692
Xue L, Deng D, Sun J (2019) Magnetoferritin: Process, prospects, and their biomedical applications. Int J Mol Sci 20(10):2426
Yablonskiy DA, Wen J, Kothapalli SV, Sukstanskii AL (2021) In vivo evaluation of heme and non-heme iron content and neuronal density in human basal ganglia. Neuroimage 235:118012
Liu M, Liu S, Ghassaban K, Zheng W, Dicicco D, Miao Y, Habib C, Jazmati T, Haacke EM (2016) Assessing global and regional iron content in deep gray matter as a function of age using susceptibility mapping. J Magn Reson Imaging 44(1):59–71
Barbosa JHO, Santos AC, Tumas V, Liu M, Zheng W, Haacke EM, Salmon CEG (2015) Quantifying brain iron deposition in patients with Parkinson’s disease using quantitative susceptibility mapping, R2 and R2. Magn Reson Imaging 33(5):559–565
Langkammer C, Liu T, Khalil M, Enzinger C, Jehna M, Fuchs S, Fazekas F, Wang Y, Ropele S (2013) Quantitative susceptibility mapping in multiple sclerosis. Radiology 267(2):551–559
Du G, Liu T, Lewis MM, Kong L, Wang Y, Connor J, Mailman RB, Huang X (2016) Quantitative susceptibility mapping of the midbrain in Parkinson’s disease. Mov Disord 31(3):317–324
de Oliveira GK, da Silva MN, Sicchieri LB, de Oliveira Silva FR, de Matos RA, Courrol LC (2015) Aminolevulinic acid with gold nanoparticles: a novel theranostic agent for atherosclerosis. Analyst 140(6):1974–1980
Ma X, Qu Q, Zhao Y (2015) Targeted delivery of 5-aminolevulinic acid by multifunctional hollow mesoporous silica nanoparticles for photodynamic skin cancer therapy. ACS Appl Mater Interfaces 7(20):10671–10676
Karaca H, Güven K, Önal M, Gürsoy Ş, Başkol M, Özkul Y (2013) The prevalence of primary hereditary hemochromatosis in central Anatolia. Turk J Gastroenterol 24(1):43–50
Spínola C, Brehm A, Spínola H (2011) Prevalence of H63D, S65C, and C282Y hereditary hemochromatosis gene variants in Madeira Island (Portugal). Ann Hematol 90(1):29–32
Guo BJ, Yang ZL, Zhang LJ (2018) Gadolinium deposition in brain: current scientific evidence and future perspectives. Front Mol Neurosci 11:335
Acknowledgements
The authors thank with grateful appreciation for the assistance and financial support provided by Tehran University of Medical Sciences (TUMS) Tehran, Iran and the support of the National Institute for Medical Research Development (NIMAD). The authors as well thank the staffs in the National Brain Mapping Lab (NBML), Tehran, Iran, for providing MRI services for us. This study was part of the Ph.D. Thesis of Anita Ebrahimpour.
Funding
The research leading to these results received funding from Tehran University of Medical Sciences (TUMS) Tehran, Iran (Grant Number: 36881) and National Institute for Medical Research Development (NIMAD, Grant Number: 977114).
Author information
Authors and Affiliations
Contributions
AE performed the acquisition and quantitative analysis of MRI images, interpretation of data, and drafting the work as the principal author. FT created the rat GBM model. BH-V performed MTT assays. AA conducted Prussian blue staining. MH revised the manuscript critically for in vivo section. PA revised the manuscript critically for in vitro section. SH performed fluorescence imaging. SAHJ and HH revised the manuscript critically for important intellectual content. ARF analyzed the results statistically. NRA contributed to the design of the work for QSM and R2* analysis and approved the final version to be published. MK designed the main conception of this work and approved the final version to be published.
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
All procedures involving animals were ethically approved by the local ethics committee of the National Institute for Medical Research Development (NIMAD, ethical code: IR.NIMAD.REC.1397.424).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ebrahimpour, A., Tirgar, F., Hajipour-Verdom, B. et al. Detection of glioblastoma multiforme using quantitative molecular magnetic resonance imaging based on 5-aminolevulinic acid: in vitro and in vivo studies. Magn Reson Mater Phy 35, 3–15 (2022). https://doi.org/10.1007/s10334-021-00978-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10334-021-00978-1