Abstract
Objective
The purpose of this study was to evaluate the impact of the negative lymph node (LN) count on the survival of the breast cancer patients in early stage after the axillary dissection.
Methods
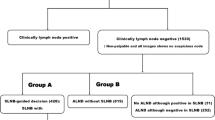
The breast cancer patients with T1–2N0–1M0 stage between January 2001 and December 2005 in Jiangsu Cancer Hospital, who underwent the axillary LNs dissection, were enrolled in this study. We analyzed the data of these patients including information of follow-up and postoperative pathological results. All patients were divided into two groups according to the axillary LN status and each group was divided into four subgroups according to the negative LN count. Cox regression analysis was performed to screen the pathological factor including the negative LN count on the survival and to compare the different negative LN count on the survival.
Results
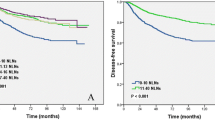
COX proportional hazard regression model showed that the survival of the breast cancer was significantly associated with the negative LN count. In T1–2N0 group, when the negative LN count was 3 or less, 4 to 5, 6 to 9 and 10 or more, the median survival time was (82.6 ± 4.1) months, (101.5 ± 1.3) months, (104.7 ± 1.0) months, and (110.5 ± 0.9) months respectively (P < 0.05). In T1–2N1 group, when the negative LN count was 6 or less, 7 to 8, 9 to 10 and 11 or more, the median survival time was (95.4 ± 1.9) months, (101.8 ± 1.1) months, (104.9 ± 1.0) months, and (106.5 ± 0.9) months respectively (P< 0.05).
Conclusion
The negative LN count can reflect the adequacy of the axillary dissection. Increasing negative LN count is independently associated with improved survival in pT1–2N0M0 or pT1–2N1M0 staging breast cancer patients. The negative LN count should be considered for incorporation into staging for breast cancer with the axillary LN dissection.
Similar content being viewed by others
References
Jatoi I, Hilsenbeck SG, Clark GM, et al. Significance of axillary lymph node metastasis in primary breast cancer. J Clin Oncol, 1999, 17: 2334–2340.
Fisher B, Bauer M, Wickerham DL, et al. Relation of number of positive axillary nodes to the prognosis of patients with primary breast cancer. An NSABP update. Cancer, 1983, 52: 1551–1557.
Singletary SE, Allred C, Ashley P, et al. Revision of the American Joint Committee on Cancer Staging system for breast cancer. J Clin Oncol, 2002, 20: 3628–3636.
Kim JY, Ryu MR, Choi BO, et al. The prognostic significance of the lymph node ratio in axillary lymph node positive breast cancer. J Breast Cancer, 2002, 14: 204–212.
Chagpar AB, Camp RL, Rimm DL. Lymph node ratio should be considered for incorporation into staging for breast cancer. Ann Surg Oncol, 18: 3143–3148.
Tausch C, Taucher S, Dubsky P, et al. Prognostic value of number of removed lymph nodes, number of involved lymph nodes, and lymph node ratio in 7502 breast cancer patients enrolled onto trials of the Austrian Breast and Colorectal Cancer Study Group (ABCSG). Ann Surg Oncol, 2012, 19: 1808–1817.
Ahn SH, Kim HJ, Lee JW, et al. Lymph node ratio and pN staging in patients with node-positive breast cancer: a report from the Korean breast cancer society. Breast Cancer Res Treat, 130: 507–515.
Schaapveld M, Otter R, de Vries EG, et al. Variability in axillary lymph node dissection for breast cancer. J Surg Oncol, 2004, 87: 4–12.
Saha S, Farrar WB, Young DC, et al. Variation in axillary node dissection influences the degree of nodal involvement in breast cancer patients. J Surg Oncol, 2000, 73: 134–137.
Chagpar AB, Scoggins CR, Martin RC 2nd, et al. Factors determining adequacy of axillary node dissection in breast cancer patients. Breast J, 2007, 13: 233–237.
Axelsson CK, Mouridsen HT, Zedeler K. Axillary dissection of level I and II lymph nodes is important in breast cancer classification. The Danish Breast Cancer Cooperative Group (DBCG). Eur J Cancer, 1992, 28: 1415–1418.
Kiricuta CI, Tausch J. A mathematical model of axillary lymph node involvement based on 1446 complete axillary dissections in patients with breast carcinoma. Cancer, 1992, 69: 2496–2501.
Giuliano AE, McCall L, Beitsch P, et al. Locoregional recurrence after sentinel lymph node dissection with or without axillary dissection in patients with sentinel lymph node metastases: the American College of Surgeons Oncology Group Z0011 randomized trial. Ann Surg, 252: 426–432; discussion 432–423.
Canessa CE, Badía F, Fierro S, et al. Anatomic study of the lymph nodes of the mesorectum. Dis Colon Rectum, 2001, 44: 1333–1336.
Topor B, Acland R, Kolodko V, et al. Mesorectal lymph nodes: their location and distribution within the mesorectum. Dis Colon Rectum, 2003, 46: 779–785.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yao, Y., Tang, J., Qin, J. et al. Clinical significance of the negative lymph node count after the axillary dissection of breast cancer patients. Chin. -Ger. J. Clin. Oncol. 11, 407–410 (2012). https://doi.org/10.1007/s10330-012-0993-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10330-012-0993-x