Abstract
Objective
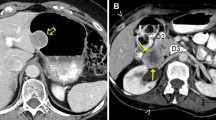
In this pictorial essay, we described the clinical, pathologic, and computed tomographic (CT) findings of malignant gastrointestinal stromal tumors (MGISTs) and attempt to establish the correlation between radiologic appearance and malignant potential.
Methods
This retrospective analysis included 20 patients receiving treatment for MGIST between 2008 and 2010. The diagnosis was established by pathology and immunohistochemistry. All these patients underwent preoperative CT. Clinical presentation, pathology and CT images were analyzed. Helical CT images were reviewed for morphologic features such as tumor size, number and location, tumor margins, necrosis, degree of enhancement and metastasis.
Results
Gastrointestinal bleeding, abdominal pain and discomfort, and without clinical symptom were common findings and were observed in 9 (45%), 6 (30%), and 5 (25%) of the 20 patients. 8 (40%) tumors were located in stomach, and 10 (50%), 1 (5%) and 1 (5%) were located in small intestine, mesentery and peritoneum, respectively. Male to female ratio was about 1:2. The size of MGIST ranged from 2.6 cm to 17.5 cm with a mean of 8.7 cm. All tumors density was inhomogeneous and heterogeneous enhancement. MGISTs with highly malignant located in small intestine were about 30% higher than stomach. The “satellite” tumours were found in 6 cases with high malignant risk. 7 cases were suffered from liver metastasis, and 4 cases went with seeding into the abdominal cavity, 1 cases went with lymph node metastasis. Histologically, 19 cases (95%) were of spindle cell type. Immunohistochemical stains demonstrated a strong positivity for both c-kit (CD117) and CD34s enhancement in 19 (95%).
Conclusion
Clinical expression is varied in MGIST patients. Female might be predominance in MGIST. The GISTs located in small intestine would tend to be more aggressive. The satellite tumours, necrosis and cystic degeneration were strongly benefit for MGIST diagnosis. Furthermore, intestinal obstruction doesn’t support the diagnosis. Lymph node metastasis and calcification is rare.
Similar content being viewed by others
References
Miettinen M, Lasota J. Gastrointestinal stromal tumors — definition, clinical, histological, immunohistochemical, and molecular genetic features and differential diagnosis. Virchows Arch, 2001, 438: 1–12.
He ZH, Lv FJ, Cao ZF, et al. Value of Multi-slice spiral CT in diagnosis of malignant gastrointestinal stromal tumors. Chinese-German J Clin Oncol, 2009, 8: 443–446.
Sandrasegaran K, Rajesh A, Rushing DA, et al. Gastrointestinal stromal tumors: CT and MRI findings. Eur Radiol, 2005, 15: 1407–1414.
Blanke C, Eisenberg BL, Heinrich M. Epidemiology of GIST. Am J Gastroenterol, 2005, 100: 2366.
Miettien M, Monihan JM, Sarlomo-Rikala M, et al. Gastrointestinal stromal tumors/smooth muscle tumors (GISTs) primary in the omentum and mesentery: clinicopathologic and immunohistochemical study of 26 cases. Am J Surg Pathol, 1999, 23: 1109–1118.
Behranwala KA, Spalding D, Wotherspoon A, et al. Small bowel gastrointestinal stromal tumours and ampullary cancer in Type I neurofibromatosis. World J Surg Oncol, 2004, 2: 1–4.
Towu E, Stanton M. Gastrointestinal stromal tumour presenting with severe bleeding: a review of the molecular biology. Pediatr Surg Int, 2006, 22: 462–464.
Du CY, Shi YQ, Zhou Y, et al. The analysis of status and clinical implication of KIT and PDGFRA mutations in gastrointestinal stromal tumor (GIST). J Surg Oncol, 2008, 98: 175–178.
Lasota J, Miettinen M. Clinical significance of oncogenic KIT and PDGFRA mutations in gastrointestinal stromal tumours. Histopathology, 2008, 53: 245–266.
Ludwig DJ, Traverso LW. Gut stromal tumors and their clinical behavior. Am J Surg, 1997, 173: 390–394.
Lee CM, Chen HC, Leung TK, et al. Gastrointestinal stromal tumor: Computed tomographic features. World J Gastroenterol, 2004, 10: 2417–2418.
Miettinen M, El-Rifai W, HL Sobin L, et al. Evaluation of malignancy and prognosis of gastrointestinal stromal tumors: a review. Hum Pathol, 2002, 33: 478–483.
Miettinen M, Lasota J. Gastrointestinal strumal tumors: review on morphology, molecular pathology, prognosis, and differential diagnosis. Arch Pathol Lab Med, 2006, 130: 1466–1478.
Egloff A, Lee EY, Dillon JE. Gastrointestinal stromal tumor (GIST) of stomach in a pediatric patient. Pediatr Radiol, 2005, 35: 728–729.
DÍaz-Delgado M, Hernández-Amate A, Sánchez-León M, et al. Multiple non-metastatic gastrointestinal stromal tumors. Differential features. Rev Esp Enferm Dig, 2010, 102: 489–497.
Miettinen M, Sobin LH, Lasota J. Gastrointestinal stromal tumors of the stomach: a clinicopathologic, immunohistochemical and molecular study of 1765 cases with long-term follow-up. Am J Surg Pathol, 2005, 29: 52–68.
Stamatakos M, Douzinas E, Stefanaki C, et al. Gastrointestinal stromal tumor. World J Surg Oncol, 2009, 7: 61.
Terada T. Gastrointestinal stromal tumor of the digestive organs: a histopathologic study of 31 cases in a single Japanese institute. Int J Clin Exp Pathol, 2009, 3: 162–168.
Heinrich MC, Corless CL, Duensing A, et al. PDGFRA activating mutations in gastrointestinal stromal tumors. Science, 2003, 299: 708–710.
Kim KM, Kang DW, Moon WS, et al. Gastrointestinal stromal tumors in Koreans: it’s incidence and the clinical, pathologic and immunohistochemical findings. J Korean Med Sci, 2005, 20: 977–984.
Nilsson B, Bumming P, Meis-Kindblom JM, et al. Gastrointestinal stromal tumors: the incidence, prevalence, clinical course, and prognostication in the preimatinib mesylate era—a population-based study in western Sweden. Cancer, 2005, 103: 821–829.
Hirota S, Isozaki K. Pathology of gastrointestinal stromal tumor. Pathol Int, 2006, 56: 1–9.
Singer S, Rubin BP, Lux ML, et al. Prognostic value of KIT mutation type, mitotic activity and histological subtype in gastrointestinal stromal tumor. J Clin Oncol, 2002, 20: 3898–3905.
Lasota J, Miettinen M. KIT and PDGFRA mutations in gastrointestinal stromal tumors (GISTs). Semin Diag Pathol, 2006, 23: 91–102.
Chourmouzi D, Sinakos E, Papalavrentios L, et al. Gastrointestinal stromal tumors: a pictorial Review. J Gastrointestin Liver Dis, 2009, 3: 379–383.
Hornick JL, Fletcher CD. Immunohistochemical staining for KIT (CD117) in soft tissue sarcomas is very limited in distribution. Am J Clin Pathol, 2002, 117: 188–193.
Fletcher CD, Berman JJ, Corless CL, et al. Diagnosis of grastrointestinal stromal tumors: A consensus approach. Hum Pathol, 2002, 33: 459–465.
Kochhar R, Manoharan P, Leahy M, et al. Imaging in gastrointestinal stromal tumours: current status and future directions. Clin Radiol, 2010, 65: 584–592.
Lau S, Tam KF, Kam CK, et al. Imaging of gastrointestinal stromal tumour (GIST). Clin Radiol, 2004, 59: 487–498.
Gupta P, Tewari M, Shulkla HS. Gastrointestinal stromal tumor. Surg Oncol, 2008, 17: 129–138.
Safdar A, Sher A. Role of c-kit/SCF in cause and treatment of gastrointestinal stromal tumors (GIST). GENE, 2007, 401: 38–45.
Conlon KC, Casper ES, Brennan MF. Primary gastrointestinal sarcomas: analysis of prognostic variables. Ann Surg Oncol, 1995, 2: 26–31.
Ulusan S, Koc Z, Kayaselcuk F, et al. Gastrointestinal stromal tumours: CT findings. Br J Radiol, 2008, 81: 618–623.
Suster S. Gastrointestinal stromal tumors. Semin Diagn Pathol, 1996, 13: 297–313.
Tashiro T, Hasegawa T, Omatsu M, et al. Gastrointestinal stromal tumour of the stomach showing lymph node metastases. Histopathology, 2005, 47: 438–439.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by grants from the National Natural Science Foundation of China (Key program, No. 30930027) and Natural Science Foundation of Guangdong Province (No. 8151503102000032).
Rights and permissions
About this article
Cite this article
Xu, Z., Pan, A., Yong, F. et al. Helical CT findings and clinicopathologic features in malignant gastrointestinal stromal tumors: the correlation between radiologic appearance and malignant potential. Chin. -Ger. J. Clin. Oncol. 10, 643–649 (2011). https://doi.org/10.1007/s10330-011-0857-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10330-011-0857-9