Abstract
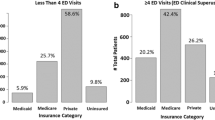
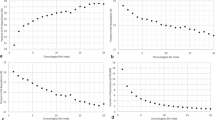
The purpose of this study was to assess if clinical indications, patient location, and imaging sites predict the viewing pattern of referring physicians for CT and MR of the head, chest, and abdomen. Our study included 166,953 CT/MR images of head/chest/abdomen in 2016–2017 in the outpatient (OP, n = 83,981 CT/MR), inpatient (IP, n = 51,052), and emergency (ED, n = 31,920) settings. There were 125,329 CT/MR performed in the hospital setting and 41,624 in one of the nine off-campus locations. We extracted information regarding body region (head/chest/abdomen), patient location, and imaging site from the electronic medical records (EPIC). We recorded clinical indications and the number of times referring physicians viewed CT/MR (defined as the number of separate views of imaging in the EPIC). Data were analyzed with the Microsoft SQL and SPSS statistical software. About 33% of IP CT and MR studies are viewed > 6 times compared to 7% for OP and 19% of ED studies (p < 0.001). Conversely, most OP studies (55%) were viewed 1–2 times only, compared to 21% for IP and 38% for ED studies (p < 0.001). In-hospital exams are viewed (≥ 6 views; 39% studies) more frequently than off-campus imaging (≥ 6 views; 17% studies) (p < 0.001). For head CT/MR, certain clinical indications (i.e., stroke) had higher viewing rates compared to other clinical indications such as malignancy, headache, and dizziness. Conversely, for chest CT, dyspnea-hypoxia had much higher viewing rates (> 6 times) in IP (55%) and ED (46%) than in OP settings (22%). Patient location and imaging site regardless of clinical indications have a profound effect on viewing patterns of referring physicians. Understanding viewing patterns of the referring physicians can help guide interpretation priorities and finding communication for imaging exams based on patient location, imaging site, and clinical indications. The information can help in the efficient delivery of patient care.


Similar content being viewed by others
References
Maros ME, Wenz R, Förster A, Froelich MF, Groden C, Sommer WH, Schönberg SO, Henzler T, Wenz H: Objective comparison using guideline-based query of conventional radiological reports and structured reports. In Vivo. 32:843–849, 2018
Pinto Dos Santos D, Hempel JM, Mildenberger P, Klöckner R, Persigehl T: Structured reporting in clinical routine. Rofo. 191:33–39, 2019
Mabotuwana T, Hombal V, Dalal S, Hall CS, Gunn M: Determining adherence to follow-up imaging recommendations. J Am Coll Radiol. 15(3 Pt A):422–428, 2018
Meng X, Ganoe CH, Sieberg RT, Cheung YY, Hassanpour S: Assisting radiologists with reporting urgent findings to referring physicians: a machine learning approach to identify cases for prompt communication. J Biomed Inform. 93:103169, 2019
Bhatti ZS, Brown RKJ, Kazerooni EA, Davenport MS: Communicating radiology test results: are our phone calls excessive, just right, or not enough? Acad Radiol. 25:365–371, 2018
Duncan KA, Drinkwater KJ, Dugar N, Howlett DC, Royal College of Radiologists’ Clinical Radiology Audit Committee: Audit of radiology communication systems for critical, urgent, and unexpected significant findings. Clin Radiol. 71:265–270, 2016
Larson PA, Berland LL, Griffith B, Kahn, Jr CE, Liebscher LA: Actionable findings and the role of IT support: report of the ACR Actionable Reporting Work Group. J Am Coll Radiol. 11:552–558, 2014
McEnery KW, Suitor CT, Thompson SK et al.: Enterprise utilization of “always on-line” diagnostic study archive. J Digit Imaging. 15(Suppl 1):81–86, 2002
Harvey HB, Krishnaraj A, Alkasab TK: A software system to collect expert relevance ratings of medical record items for specific clinical tasks. JMIR Med Inform. 2:e3, 2014
Funding
One study co-author (MKK) received research grants from Siemens Healthineers and Riverain Inc. for unrelated research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This retrospective, quality assurance study was exempted from Institutional Review Board approval and used de-identified patient information.
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Homayounieh, F., Singh, R., Chen, T. et al. Viewing Imaging Studies: How Patient Location and Imaging Site Affect Referring Physicians. J Digit Imaging 33, 334–340 (2020). https://doi.org/10.1007/s10278-019-00279-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10278-019-00279-z