Abstract
Objective
To assess the appropriateness of Computed Tomography (CT) examinations, using the ESR-iGuide.
Material and methods
A retrospective study was conducted in 2022 in a medium-sized acute care teaching hospital. A total of 278 consecutive cases of CT referral were included. For each imaging referral, the ESR-iGuide provided an appropriateness score using a scale of 1–9 and the Relative Radiation Level using a scale of 0–5. These were then compared with the appropriateness score and the radiation level of the recommended ESR-iGuide exam.
Data analysis
Pearson’s chi-square test or Fisher exact test was used to explore the correlation between ESR-iGuide appropriateness level and physician, patients, and shift characteristics. A stepwise logistic regression model was used to capture the contribution of each of these factors.
Results
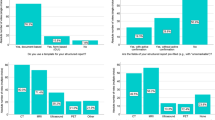
Most of exams performed were CT head (63.67%) or CT abdominal pelvis (23.74%). Seventy percent of the actual imaging referrals resulted in an ESR-iGuide score corresponding to “usually appropriate.” The mean radiation level for actual exam was 3.2 ± 0.45 compared with 2.16 ± 1.56 for the recommended exam. When using a stepwise logistic regression for modeling the probability of non-appropriate score, both physician specialty and status were significant (p = 0.0011, p = 0.0192 respectively). Non-surgical and specialist physicians were more likely to order inappropriate exams than surgical physicians.
Conclusions
ESR-iGuide software indicates a substantial rate of inappropriate exams of CT head and CT abdominal-pelvis and unnecessary radiation exposure mainly in the ED department. Inappropriate exams were found to be related to physicians' specialty and seniority.
Clinical relevance statement
These findings underscore the urgent need for improved imaging referral practices to ensure appropriate healthcare delivery and effective resource management. Additionally, they highlight the potential benefits and necessity of integrating CDSS as a standard medical practice. By implementing CDSS, healthcare providers can make more informed decisions, leading to enhanced patient care, optimized resource allocation, and improved overall healthcare outcomes.
Key Points
• The overall mean of appropriateness for the actual exam according to the ESR-iGuide was 6.62 ± 2.69 on a scale of 0–9.
• Seventy percent of the actual imaging referrals resulted in an ESR-iGuide score corresponding to “usually appropriate.”
• Inappropriate examination is related to both the specialty of the physician who requested the exam and the seniority status of the physician.


Similar content being viewed by others
Abbreviations
- ACR:
-
American College of Radiology
- CDSS:
-
Clinical decision support systems
- CT:
-
Computed tomography
- ICRP:
-
International Commission on Radiological Protection
- RCR:
-
Royal College of Radiologists
- RRL:
-
Relative radiation level
- ESR:
-
European Society of Radiology
- QSI:
-
Quality and safety in imaging
References
Hadad S, Hadad Y, health TSTTE journal of, 2013 undefined (2013) Determinants of healthcare system’s efficiency in OECD countries. Springer. 14(2):253–265. https://doi.org/10.1007/s10198-011-0366-3
Rao VM, Levin DC (2012) The overuse of diagnostic imaging and the choosing wisely initiative. Ann Intern Med 157(8):574–576. https://doi.org/10.7326/0003-4819-157-8-201210160-00535
Smith-Bindman R, Miglioretti DL, Larson EB (2008) Rising use of diagnostic medical imaging in a large integrated health system: the use of imaging has skyrocketed in the past decade, but no one patient population or medical condition is responsible. Health Aff (Millwood) 27(6):1491. https://doi.org/10.1377/HLTHAFF.27.6.1491
Winder M, Owczarek AJ, Chudek J, Pilch-Kowalczyk J, Baron J (2021) Are we overdoing it? Changes in diagnostic imaging workload during the years 2010–2020 including the impact of the SARS-CoV-2 pandemic. Healthcare. 9(11):1557. https://doi.org/10.3390/HEALTHCARE9111557
Smith-Bindman R, Kwan ML, Marlow EC et al (2019) Trends in use of medical imaging in US health care systems and in Ontario, Canada, 2000–2016. JAMA 322(9):843–856. https://doi.org/10.1001/JAMA.2019.11456
Allen B, Prabhakar Reddy K, Miller W et al (2017) Summary of the proceedings of the international forum 2016: “Imaging referral guidelines and clinical decision support - how can radiologists implement imaging referral guidelines in clinical routine?” Insights Imaging 8(1):1. https://doi.org/10.1007/S13244-016-0523-4
Levin DC, Rao VM (2017) Reducing inappropriate use of diagnostic imaging through the choosing wisely initiative. J Am Coll Radiol 14(9):1245–1252. https://doi.org/10.1016/j.jacr.2017.03.012
Flaherty S, Zepeda ED, Mortele K, Young GJ (2019) Magnitude and financial implications of inappropriate diagnostic imaging for three common clinical conditions. Int J Qual Health Care 31(9):691–697. https://doi.org/10.1093/INTQHC/MZY248
ACR Appropriateness Criteria (2015) Literature search process. Available via https://www.acr.org/-/media/ACR/Files/Appropriateness-Criteria/LiteratureSearchProcess.pdf. Last Accessed 14 June 2023
Subramaniam RM, Kurth DA, Waldrip CA, Rybicki FJ (2019) American College of Radiology Appropriateness Criteria: advancing evidence-based imaging practice. Semin Nucl Med 49(2):161–165. https://doi.org/10.1053/J.SEMNUCLMED.2018.11.011
Sheng AY, Castro A, Lewiss RE (2016) Awareness, utilization, and education of the ACR Appropriateness Criteria: a review and future directions. J Am Coll Radiol 13(2):131–136. https://doi.org/10.1016/J.JACR.2015.08.026
Kawamoto K, Houlihan CA, Balas EA, Lobach DF (2005) Improving clinical practice using clinical decision support systems: a systematic review of trials to identify features critical to success. BMJ 330(7494):765–768. https://doi.org/10.1136/BMJ.38398.500764.8F
Heekin AM, Kontor J, Sax HC, Keller MS, Wellington A, Weingarten S (2018) Choosing wisely clinical decision support adherence and associated inpatient outcomes. Am J Manag Care. 24(8):361 (Accessed September 5, 2022. /pmc/articles/PMC6813785/)
Bautista AB, Burgos A, Nickel BJ, Yoon JJ, Tilara AA, Amorosa JK (2012) Do clinicians use the American College of Radiology Appropriateness Criteria in the management of their patients? AJR Am J Roentgenol 192(6):1581–1585. https://doi.org/10.2214/AJR.08.1622
Boland GW, Weilburg J, Duszak R (2015) Imaging appropriateness and implementation of clinical decision support. J Am Coll Radiol 12(6):601–603. https://doi.org/10.1016/j.jacr.2015.03.014
European Society of Radiology (ESR) (2019) Methodology for ESR iGuide content. Insights Imaging 10(1):32. https://doi.org/10.1186/S13244-019-0720-Z
Gabelloni M, Di NM, Morganti R et al (2020) Application of the ESR iGuide clinical decision support system to the imaging pathway of patients with hepatocellular carcinoma and cholangiocarcinoma: preliminary findings. Radiol Med 125:531–537. https://doi.org/10.1007/s11547-020-01142-w
Markus T, Saban M, Sosna J et al (2023) Does clinical decision support system promote expert consensus for appropriate imaging referrals? Chest–abdominal–pelvis CT as a case study. Insights Imaging 14(1):45. https://doi.org/10.1186/S13244-023-01371-3
Francisco MZ, Altmayer S, Verma N et al (2021) Appropriateness of computed tomography and ultrasound for abdominal complaints in the emergency department. Curr Probl Diagn Radiol 50(6):799–802. https://doi.org/10.1067/J.CPRADIOL.2020.11.004
American College of Radiology. ACR Appropriateness Criteria evidence table development. – (2015). https://www.acr.org/-/media/ACR/Files/Appropriateness-Criteria/EvidenceTableDevelopment.pdf. Accessed June 14, 2023
Sullivan KM, Dean A, Minn MS (2009) OpenEpi: a web-based epidemiologic and statistical calculator for public health. Public Health Rep 124(3):471–474. https://doi.org/10.1177/003335490912400320
Salerno S, Terranova MC, Anzelmo MT et al (2022) Are we overusing abdominal computed tomography scans in young patients referred in an emergency for acute abdominal pain? Pol J Radiol 87(1):187–193. https://doi.org/10.5114/PJR.2022.115126
Rühm W, Laurier D, Wakeford R (2022) Cancer risk following low doses of ionising radiation – current epidemiological evidence and implications for radiological protection. Mutat Res Genet Toxicol Environ Mutagen 873:503436. https://doi.org/10.1016/J.MRGENTOX.2021.503436
Rühm W, Harrison RM (2019) High CT doses return to the agenda. Radiat Environ Biophys 59(1):3–7. https://doi.org/10.1007/S00411-019-00827-9
Rehani MM, Berris T (2012) International Atomic Energy Agency study with referring physicians on patient radiation exposure and its tracking: a prospective survey using a web-based questionnaire. BMJ Open 2(5):1425. https://doi.org/10.1136/bmjopen-2012-001425
Kosicka B, Ksykiewicz-Dorota A, Kulczycka K, Stychno E, Piasecka K, Drop B (2019) Decision making models in various fields of nursing. Polish J Public Health. 129(3):87–94. https://doi.org/10.2478/pjph-2019-0021
Kindie Abate H, Birhanu Y, Hailu Gebrie M (2022) Clinical decision making approaches and associated factors among nurses working in a tertiary teaching hospital. Int J Afr Nurs Sci. 17:100432. https://doi.org/10.1016/J.IJANS.2022.100432
Smith S, Parker T, Parker P (2022) The justification of non-obstetric ultrasound referrals: a safe and effective practice. Ultrasound 30(1):52–61. https://doi.org/10.1177/1742271X211005510
Saban M, Sosna J, Singer C et al (2022) Clinical decision support system recommendations: how often do radiologists and clinicians accept them? Eur Radiol 32(6):4218–4224. https://doi.org/10.1007/S00330-021-08479-4
Gabelloni M, Di Nasso M, Morganti R et al (2020) Application of the ESR iGuide clinical decision support system to the imaging pathway of patients with hepatocellular carcinoma and cholangiocarcinoma: preliminary findings. Radiol Med 125(6):531–537. https://doi.org/10.1007/S11547-020-01142-W
Young GJ, Flaherty S, Zepeda ED, Mortele KJ, Griffith JL (2020) Effects of physician experience, specialty training, and self-referral on inappropriate diagnostic imaging. J Gen Intern Med 35(6):1661–1667. https://doi.org/10.1007/S11606-019-05621-3/TABLES/3
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Contributions
SR, CS, and MS interpreted the data and edited and approved the final article. AK, AM, NG, MR, and SG conceptualized and designed the study, drafted the initial manuscript, and reviewed and revised the manuscript. MS, SV, and OL designed the methods section, analyzed the data, and reviewed and revised the manuscript. SR, CS, and MS critically reviewed the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Mor Saban.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise (Clara Singer).
Informed consent
Written informed consent was not required for this study because the data is archival data.
Ethical approval
Institutional Review Board approval was obtained.
The study protocol was approved by the Institutional Human Subjects Ethics Committee (CM-0058–21).
Study subjects or cohorts overlap
None.
Methodology
• Retrospective
• Observational
• performed at one institution
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rosen, S., Singer, C., Vaknin, S. et al. Inappropriate CT examinations: how much, who and where? Insights from a clinical decision support system (CDSS) analysis. Eur Radiol 33, 7796–7804 (2023). https://doi.org/10.1007/s00330-023-10136-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-10136-x