Abstract
The maxilla occupies a key position in dentofacial orthopaedics, since its transversal development can be directly influenced by orthodontic therapy. The maturation stages of the mid-palatal suture, which are obtained from cone-beam computed tomography images (CBCT), present an addition to clinical decision-making in transversal discrepancies of the upper jaw. In an endeavour to reduce ionizing radiation in adolescents and young adults, who are particularly susceptible to long term stochastic irradiation effects, we investigated the feasibility of 3 Tesla (3T) MRI in detecting the maturation stages of the mid-palatal suture. A collective of 30 patients aged 24–93 years with routine neck MRI at 3T, underwent an additional three-dimensional isotropic T1 weighted study sequence of the midface. Image evaluation was performed on axial, multi-planar formatted reconstructions of the dataset aligned to the midline axis of the palate, and curved reconstructions aligned to the concavity of the palate. Inverted images helped to achieve an image impression similar to the well-known CBCT appearance. All datasets were reviewed by three readers and mid-palatal maturation was scored twice according to Angelieri et al. Intra- and inter-rater agreement were evaluated to measure the robustness of the images for clinical evaluation. 3T MRI deemed reliable for the assessment of mid-palatal suture maturation and hence for the appraisal of the hard palate and its adjacent sutures. The data of this pilot study display the feasibility of non-ionizing cross-sectional MRI for the determination of sutural maturation stages. These findings underline the potential of MRI for orthodontic treatment planning, further contributing to the avoidance of unnecessary radiation doses.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The upper jaw is of the utmost importance for orthodontics and orofacial orthopaedics, since transversal and sagittal maxillary growth development can be actively influenced [1, 2]. Transversal palatal expansion is particularly intriguing, since this simultaneously widens the nasal floor [3]. As a consequence, it enhances nasal breathing and has been described to improve sleep apnoea in children and overall quality of life [4,5,6,7]. Rapid maxillary expansion is, therefore, considered to be an orthodontic procedure with a high impact on general health [8]. In children, who are treated before the peak of growth velocity, this intervention is efficient and predictable [9]. However, with increasing age, it becomes increasingly difficult to predict the success rate of transverse expansion as there is no linear correlation between patient age and suture fusion [10]. Starting in late adolescence, maxillary resistance becomes increasingly pronounced, so that a transversal deficiency can only be corrected with an additional subtotal Le Fort I osteotomy [11, 12]. Since the cut-off value for surgery is still very much empirical, sutural maturation stages have been classified histologically and radiologically to increase the predictability of rapid maxillary expansion in late adolescence [13,14,15,16]. Cross-sectional CBCT imaging has been described as a non-invasive method for the assessment of mid-palatal suture maturation in clinical routine [17]. Angelieri et al. were the first to use axial CBCT images in 2013 to describe 5 different stages of maturation, ranging from A, an open suture, radiologically depicted as a line of high density with little or no interdigitation (Fig. 1A–E) to E, a completely fused suture (Fig. 1E) [13, 17, 18]. The authors suggest that patients with stages D and E (Fig. 1D, E) as the most obliterated ones, will most likely experience inadequate success of treatment and iatrogenic side effects ranging from buccal tipping, recessions to gingival ulcers and will, therefore, benefit most from additional surgery [10, 17, 19, 20]. Although Angelieri et al. have introduced a promising approach towards individualised orthodontic treatment, a cone-beam computed tomography (CBCT) or computed tomography (CT) has to be carried out to obtain their index. According to the linear-non-threshold-model (LTN), ionizing radiation is always linked to an elevated stochastic cancer risk and children, who represent the phenotypical orthodontic patient collective, have been described to be particularly susceptible to irradiation side effects [21,22,23,24,25]. In recent years, MRI as a non-ionizing methodology to obtain cross-sectional images, has found increasing application in dental medicine and orthodontics [26,27,28,29]. This is mainly due to continuously increasing spatial resolution and image contrast as well as decreasing scan duration [30, 31]. MRI scanners are available at different B0-field strengths (magnetic flux density), ranging from 0.55 to 7 Tesla (T = kg⋅s−2⋅A−1) for clinical application. The feasibility of 1.5 T Black Bone MRI for the detection of mid-palatal suture maturation was first described by Rossi et al. in a preliminary study investigating one patient only [32]. Black bone MRI was considered to have clinical potential for assessment of the hard palate and adjacent sutures [32]. The aim of this retrospective study was to assess the feasibility of 3 T MRI in diagnosing the maturation stages of the mid-palatal suture investigating a larger sample size.
I displays a schematic drawing, (adapted from Angeleri et al. [17]) and II displays the corresponding cross-sectional images of the five maturation stages in CT. In I, the maxillary is colored in yellow while the palatine bones are depicted in orange and the suture is colored in blue, the sphenoid bone is colored in dark yellow. In the first 3 stages (A–C), the suture is visible in both the maxillary and palatal bones, while in stage (D), the suture in the palatal bone has already fused and in stage E complete fusion has taken place in both bones
Materials and methods
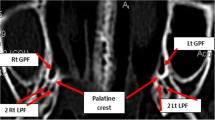
After approval of the institutional review board (IRB Number: 22–338-Br), we retrospectively selected patients from our archives, who had received a diagnostic neck MRI and an additional study sequence of the midface, in a time period from March 2021 to July 2022. Patients were only enclosed if they had a full dentition, with a maximum of one singular tooth missing per jaw. Subjects with facial skull asymmetries, previous trauma or surgery of the midface, craniofacial malformations, displaced teeth in the palatal region and metabolic bone disorders were excluded. After screening the records of 50 applicable cases, a total of 30 patients met the inclusion criteria for further analysis. This sample size is in line with the rules of Koo et al. who consider a heterogeneous sample size of 30 people with 3 readers involved to be valid for a reliability study [33]. All of the patients had received a three-dimensional isotropic T1 weighted sequence, allowing for 3D reconstruction: T1w single slab 3D TSE sequence with slab selective, variable excitation pulse ((SPACE, Siemens Healthcare GmbH, Erlangen, Germany), TE 27 ms, TR 700 ms, flip angle mode: T1Var (Tissue T1 940/Tissue T2 100/Organ Exam Standard), field of view 250 × 250 mm, matrix 320 × 320)). The reconstructed voxel size was 0.4 × 0.4 × 0.8 mm. This sequence enables both, a good visualisation of the bony marrow structures and an individual 3D angulation to the hard palate, suitable for the detection of the five mid-palatal maturation stages according to Angelieri et al. [13, 17, 18]. In addition to the underlying MRI, a total of 5 patients had additionally received a high resolution CT (Siemens SOMATOM X.ceed; slice thickness 0.5 mm; tube voltage 100 kV) on account of a medical justifying indication. The images of these patients were employed to validate MR image quality of the sutural region as opposed to the CT images as the gold standard (Figs. 2, 3, 4). All of the MR images were subsequently inverted to yield a closer resemblance to the image impression on CBCT (Figs. 3, 4). The Angelieri maturation stages are scored on a five-point scale (stages A–E) (Figs. 1, 2) [17]. In stages A–C, the suture is visible in both the maxillary and palatine bones. Stage A is described as straight high-density line with no or little interdigitation (Fig. 1A) [17]. Stage B is defined as a scalloped high-density line with a phenotypically irregular shape (Fig. 1B) while in stage C, there are two parallel, scalloped, high-density lines close to each other (Fig. 1C) [17]. In stage D, sutural fusion has commenced in the palatine bone (Fig. 1D) and in stage E, the suture is totally fused (Fig. 1E) [17]. For the assessment of the above-mentioned indices, we reconstructed dedicated axial MR images, strictly abiding by the respective sagittal and coronal head orientation as proposed by Angelieri [17]. In addition, the 3D data sets could be adapted to the midline axis of the palate, using a standard multiplanar reconstruction (MPR) viewer. Furthermore, in patients with a particularly high or thick plate, a curved reconstruction was performed, aligning the plane with the concave shape of the palate in coronal view. This allows the comprehensive assessment of the suture in one single plane, even in cases of complex anatomy (Fig. 5). In a blinded investigation setting, 3 raters with more than 5 years expertise in maxillofacial radiology assessed the maturation stages of 30 MRI data sets twice. Consensus reading was performed in 10 trial cases prior to the study evaluation inter- and intraexaminer reliability was estimated for all raters using Cohen’s (unweighted) kappa with a 2 week period between the different readings [34].
Results
3T MRI of the midface was successfully performed in 30 patients (24–93 years; 15 females, 15 males; mean age 54 ± 17). Mean acquisition time was 07:26 min. Minor motion artefacts were only observed in a minor proportion of all patients. In patients with a very high or thick palate, we employed curved MPR reconstructions to visualise the entire palate in one axial slice as opposed to evaluating two different slices as described in the original protocol (Fig. 5). Two senior radiologists validated and critically evaluated the five patients who had received both, a high-resolution CT as the current gold standard and a 3 T MRI. Although the MR image quality does not yet match the thin-slice CT and is inferior in terms of resolution, it was deemed feasible for further analysis and interpretation (Figs. 3, 4). All 30 MRIs were rated twice by all three raters, who had been calibrated beforehand, with both, the native MRI as well as the inverted versions being presented to the raters. For the 30 MRI data sets inter-rater reliability for palatal maturation demonstrated substantial agreement, with an overall Cohens Kappa Coefficient of 0.72 [0.64; 0.80] for the first and second measurement (Table 1). Intra-rater reliability for palatal maturation equally proved substantial agreement, with weighted Kappa Coefficients being 0.69 [0.67; 0.95] (Rater 1), 0.68 [0.68; 0.95] (Rater 2) and 0.77 [0.75; 0.98] (Rater 3) (Table 1) [35]. Differential ratings were more frequent in patients with stages B, C and D while the rates were able to discriminate between stages A, and E with relative ease. By means of inversion, the MR image resembles to the suture as displayed on CBCT or conventional CT (Figs. 2, 3). The results of the inverted axial MRI slides are shown in Fig. 6.
Displays the 5 different maturation stages A–E as obtained on 3 T MRI (T1 = original T1w 3 T MRI; B: inverted 3T MR image). In stages A–C, the suture is visible in both the maxillary (white arrow in A–E) and palatine bones [17](yellow arrow in A–E). A Stage A: the suture is straight high-density line with no or little interdigitation [17]. B Stage B: the suture is depicted as a scalloped high-density line with an irregular shape [17]. C Stage C: the suture comprised two parallel, scalloped, high-density lines close to each other [17]. D Stage D: sutural fusion has commenced in the palatine bone [17] (yellow arrow). E Stage E: the suture is totally fused and is neither visible in the maxillary (white arrow) nor palatine bones (yellow arrow) [17]
Discussion
In dental radiology, different indications, such as impacted- and supplementary teeth, orofacial clefts, pre-surgical planning among others, warrant 3D imaging [36,37,38]. With regard to sutural maturation status, there is no linear correlation between chronological or skeletal age and mid-palatal suture fusion [39]. Cross-sectional imaging can be beneficial to the assessment of the precise maturation stage, facilitating clinical decision making and outcome [13]. Up-to-date, axial CBCT images present the gold standard for the assessment of sutural maturation status [13, 17, 18]. As opposed to 2D panoramic images, which are routinely performed in dental medicine, CBCT creates 3D images without superimposition with other anatomic landmarks, allowing for a standardized description of mid-palatal sutures maturation [40, 41]. However, since children and young adults present a large proportion of the orthodontic patient collective, the medical indication for employing ionizing radiation has to be well-considered [38]. Children are significantly more vulnerable to long term, stochastic irradiation effects than adults, with radiation risk being inversely proportional with age [42]. With regard to radiation exposure, pronounced differences have been observed between CBCT units, with dose assessment being particularly challenging in children [43, 44]. CBCT doses in pediatric dento-maxillofacial imaging range from 103 µSv for upper and lower jaw imaging (FOV 10 × 10, small FOV) to 175 µSv for skull protocols (medium 17 × 11 and large 24 × 19 FOV) [44]. The lifetime attributable risk is particularly high in skull protocols, which have equally been reported to dramatically increase the likelihood of brain cancer in children [23, 44]. A further disadvantage seems to be that many dental CBCT units are tailored to usage in adults and many do not have imaging protocols specific for a paediatric population, resulting in elevated radiation doses for the thyroid gland, the eye lenses, the brain, and the salivary glands [42, 45]. Due to the above-mentioned disadvantages of ionising radiation in pediatric dentistry, there have been increasing efforts to implement non-ionising cross-sectional imaging into clinical routine [31]. In this pilot study we investigated the suitability of 3T MRI for the conspicuity of the hard palate and its adjacent sutures. A robust intra-, and inter-rater reliability were observed, however, our reliabilities values are not as high as those reported in other CBCT studies, evaluating sutural maturation [17, 39]. This might be attributed to the image quality of MRI, which is still inferior to CT/CBCT, particularly with regard to spatial resolution. Furthermore, dentists are not accustomed to routinely evaluate MR images, however, with respective training, the skills in evaluating dental MRI could certainly be improved. We consciously inverted the T1w MRI sequences to obtain an image impression that is comparable to CBCT, facilitating the transition from CBCT to MRI for dentists (Fig. 6). Discrepancies with regard to inter-rater reliability, were primarily found in stages B, C and D while stages A and E were scored with relative ease. This might be due to the fact that stages A (an open and wide suture, Figs. 1A, 6A) and E (a completely fused suture, Figs. 1E, 6E) are more likely a visual diagnosis with less differential diagnostic contemplations to be made. In patients with a very high or very thick palate, the respective axial slices are often not appropriate for the visualization of the entire suture in a single image. In those cases, the evaluation of at least two slices per jaw has been described by Angelieri et al. for a valid assessment of the actual anatomy [17]. We utilized curved MPR reconstructions, which are widely available on MRI scanners and in 3D post-processing tools. Those curved reconstructions and can ease the reading and increase the accuracy of the respective maturation status (Fig. 5). The fact that our approach is based on MRI data, might certainly present a limitation for many dentists, since MRI, as opposed to CBCT, is not readily available in every clinical setting. In addition, the acquisition recording time of 07:26 min is quite long, which leads to an increased risk of movement artefacts and is impractical in clinical orthodontic routine. However, with novel MRI devices and respective protocol optimization using artificial intelligence, acquisition times are likely to decrease in the near future, resulting in patient friendly examination times. Due to the retrospective design of this study the patient collective is comprised of adults only and the respective MR sequences have to be confirmed in paediatric patients to improve clinical validity. The validity of the Angelieri method in general has been questioned and alternative grading methods based on CBCT images e.g. density of the sutural area relative to soft tissues have been introduced [46]. The presented MRI protocol might, therefore, be helpful to reduce ionizing radiation in other study settings investigating the hard palate and adjacent sutures. The results of the preset pilot study display the feasibility of 3T MRI with a T1w single slab 3D TSE sequence for the depiction of the hard palate and mid-palatal suture. Inversion of the MR images yields a closer resemblance to an image impression comparable to CBCT. Further studies with larger sample sizes, including a pediatric collective, are aimed to improve and standardize non-ionizing imaging in dental radiology.
References
Coloccia G, Inchingolo AD, Inchingolo AM, et al. Effectiveness of dental and maxillary transverse changes in tooth-borne, bone-borne, and hybrid palatal expansion through cone-beam tomography: a systematic review of the literature. Medicina. 2021;57:288.
Delaire J. Maxillary development revisited: relevance to the orthopaedic treatment of Class III malocclusions. Eur J Orthod. 1997;19:289–311.
Altieri F, Cassetta M. Comparison of changes in skeletal, dentoalveolar, periodontal, and nasal structures after tooth-borne or bone-borne rapid maxillary expansion: a parallel cohort study. Am J Orthod Dentofacial Orthop. 2022;161:e336–44.
Alyessary AS, Othman SA, Yap AUJ, Radzi Z, Rahman MT. Effects of non-surgical rapid maxillary expansion on nasal structures and breathing: a systematic review. Int Orthod. 2019;17:12–9.
Hoxha S, Kaya-Sezginer E, Bakar-Ates F, Köktürk O, Toygar-Memikoğlu U. Effect of semi-rapid maxillary expansion in children with obstructive sleep apnea syndrome: 5-month follow-up study. Sleep Breath. 2018;22:1053–61.
Kiliç N, Oktay H. Effects of rapid maxillary expansion on nasal breathing and some naso-respiratory and breathing problems in growing children: a literature review. Int J Pediatr Otorhinol. 2008;72:1595–601.
Pithon MM, Marañón-Vásquez GA, da Silva LP, et al. Effect of treatment of transverse maxillary deficiency using rapid palatal expansion on oral health-related quality of life in children: a randomized controlled trial. Am J Orthod Dentofacial Orthop. 2022;161:172–81.
McNamara JA Jr, Lione R, Franchi L, et al. The role of rapid maxillary expansion in the promotion of oral and general health. Prog Orthod. 2015;16:33.
Baccetti T, Franchi L, Cameron CG, McNamara JA Jr. Treatment timing for rapid maxillary expansion. Angle Orthod. 2001;71:343–50.
Isfeld D, Lagravere M, Leon-Salazar V, Flores-Mir C. Novel methodologies and technologies to assess mid-palatal suture maturation: a systematic review. Head Face Med. 2017;13:13.
Gorback NR, Infante CM. A combined orthodontic and surgical procedure for rapid palatal expansion in skeletally mature patients. JCO. 1975;9:56–8.
Kraut RA. Surgically assisted rapid maxillary expansion by opening the midpalatal suture. J Oral Maxillofac Surg. 1984;42:651–5.
Angelieri F, Franchi L, Cevidanes LHS, Bueno-Silva B, McNamara JA Jr. Prediction of rapid maxillary expansion by assessing the maturation of the midpalatal suture on cone beam CT. Dental Press J Orthod. 2016;21:115–25.
Tonello DL, Ladewig VM, Guedes FP, Ferreira Conti ACC, Almeida-Pedrin RR, Capelozza-Filho L. Midpalatal suture maturation in 11 to 15 year olds: a cone-beam computed tomographic study. Am J Orthod Dentofacial Orthop. 2017;152:42–8.
Wehrbein H, Yildizhan F. The mid-palatal suture in young adults a radiological-histological investigation. Euro J Orthod. 2001;23(105):14.
Willershausen I, Erbe C, Al-Maawi S, Orlowska A, Wehrbein H, Ghanaati S. Development of a novel histological and histomorphometric evaluation protocol for a standardized description of the mid-palatal suture-an ex vivo study. J Anat. 2019;235:180–8.
Angelieri F, Cevidanes LH, Franchi L, Gonçalves JR, Benavides E, McNamara JA Jr. Midpalatal suture maturation: classification method for individual assessment before rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 2013;144:759–69.
Angelieri F, Franchi L, Cevidanes LHS, et al. Cone beam computed tomography evaluation of midpalatal suture maturation in adults. Int J Oral Maxillofac Surg. 2017;46:1557–61.
Bastos R, Blagitz MN, Aragón M, Maia LC, Normando D. Periodontal side effects of rapid and slow maxillary expansion: a systematic review. Angle Orthod. 2019;89:651–60.
Chang JY, McNamara JA Jr, Herberger TA. A longitudinal study of skeletal side effects induced by rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 1997;112:330–7.
Bernier MO, Baysson H, Pearce MS, et al. Cohort profile: the EPI-CT study: a European pooled epidemiological study to quantify the risk of radiation-induced cancer from paediatric CT. Int J Epidemiol. 2019;48:379–81.
Breckow J. Linear-no-threshold is a radiation-protection standard rather than a mechanistic effect model. Radiat Environ Biophys. 2006;44:257–60.
Hauptmann M, Byrnes G, Cardis E, et al. Brain cancer after radiation exposure from CT examinations of children and young adults: results from the EPI-CT cohort study. Lancet Oncol. 2023;24:45–53.
Meulepas JM, Ronckers CM, Smets A, et al. Radiation exposure from pediatric CT scans and subsequent cancer risk in the Netherlands. J Natl Cancer Inst. 2019;111:256–63.
Pearce MS, Salotti JA, Little MP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet (London, England). 2012;380:499–505.
Hilgenfeld T, Juerchott A, Jende JME, et al. Use of dental MRI for radiation-free guided dental implant planning: a prospective, in vivo study of accuracy and reliability. Eur Radiol. 2020;30:6392–401.
Hövener JB, Zwick S, Leupold J, et al. Dental MRI: imaging of soft and solid components without ionizing radiation. JMRI. 2012;36:841–6.
Juerchott A, Freudlsperger C, Weber D, et al. In vivo comparison of MRI- and CBCT-based 3D cephalometric analysis: beginning of a non-ionizing diagnostic era in craniomaxillofacial imaging? Eur Radiol. 2020;30:1488–97.
März K, Chepura T, Plewig B, et al. Cephalometry without complex dedicated postprocessing in an oriented magnetic resonance imaging dataset: a pilot study. Euro J Orthod. 2021;43:614–21.
Abkai C, Hourfar J, Glockengießer J, et al. Ultra short time to echo (UTE) MRI for cephalometric analysis-potential of an x-ray free fast cephalometric projection technique. PLoS ONE. 2021;16: e0257224.
Flügge T, Gross C, Ludwig U, et al. Dental MRI-only a future vision or standard of care? A literature review on current indications and applications of MRI in dentistry. Dentomaxillofac Radiol. 2023;52:20220333.
Rossi NJ, Rossi RC, Rossi NJC, Rossi BC (2018) Assessment of palatine suture maturation by “Black Bone” Rmi-a preliminary feasibility study
Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15:155–63.
Cohen J. A coefficient of agreement for nominal scales. Edu Psychol Meas. 1960;20:37–46.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74.
Apostolakis D, Michelinakis G, Kamposiora P, Papavasiliou G. The current state of computer assisted orthognathic surgery: a narrative review. J Dent. 2022;119: 104052.
Kapetanović A, Oosterkamp BCM, Lamberts AA, Schols J. Orthodontic radiology: development of a clinical practice guideline. Radiol Med. 2021;126:72–82.
Oenning AC, Jacobs R, Pauwels R, Stratis A, Hedesiu M, Salmon B. Cone-beam CT in paediatric dentistry: DIMITRA project position statement. Pediatr Radiol. 2018;48:308–16.
Gonzálvez Moreno AM, Garcovich D, Zhou WuA, et al. Cone beam computed tomography evaluation of midpalatal suture maturation according to age and sex: a systematic review. Eur J Paediatr Dent. 2022;23:44–50.
Murray D, Whyte A. Dental panoramic tomography: what the general radiologist needs to know. Clin Radiol. 2002;57:1–7.
Sams CM, Dietsche EW, Swenson DW, DuPont GJ, Ayyala RS. Pediatric panoramic radiography: techniques, artifacts, and interpretation. Radiographics. 2021;41:595–608.
Vogiatzi T, Menz R, Verna C, Bornstein MM, Dagassan-Berndt D. Effect of field of view (FOV) positioning and shielding on radiation dose in paediatric CBCT. Dentomaxillofac Radiol. 2022. https://doi.org/10.1259/dmfr.20210316.
Ludlow JB, Timothy R, Walker C, et al. Effective dose of dental CBCT-a meta analysis of published data and additional data for nine CBCT units. Dentomaxillofac Radiol. 2015;44:20140197.
Stratis A, Zhang G, Jacobs R, Bogaerts R, Bosmans H. The growing concern of radiation dose in paediatric dental and maxillofacial CBCT: an easy guide for daily practice. Eur Radiol. 2019;29:7009–18.
Haba T, Nishihara Y, Saito Y, et al. Estimating organ dose with optimized peak dose index in cone-beam CT scans. Phys Med. 2024;118: 103215.
Savoldi F, Wong KK, Yeung AWK, Tsoi JKH, Gu M, Bornstein MM. Midpalatal suture maturation staging using cone beam computed tomography in patients aged between 9 to 21 years. Sci Rep. 2022;12:4318.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors disclose no conflict of interest related to the present article. With regard to activities not related to this article, M.K., M.U. and M.S.M are members of the speaker’s bureau of Siemens Healthcare GmbH.
Ethical approval
The institutional review board of the Friedrich-Alexander-University Erlangen-Nuremberg approved of this study (IRB Number: 22–338-Br).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Willershausen, I., Kopp, M., Scholz, M. et al. Feasibility of 3 Tesla MRI for the assessment of mid-palatal suture maturation: a retrospective pilot study. Odontology (2024). https://doi.org/10.1007/s10266-024-00950-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10266-024-00950-0