Abstract
Cancer patients are more vulnerable to COVID-19 compared to the general population, but it remains unclear which types of cancer have the highest risk of COVID-19-related mortality. This study examines mortality rates for those with hematological malignancies (Hem) versus solid tumors (Tumor). PubMed and Embase were systematically searched for relevant articles using Nested Knowledge software (Nested Knowledge, St Paul, MN). Articles were eligible for inclusion if they reported mortality for Hem or Tumor patients with COVID-19. Articles were excluded if they were not published in English, non-clinical studies, had insufficient population/outcomes reporting, or were irrelevant. Baseline characteristics collected included age, sex, and comorbidities. Primary outcomes were all-cause and COVID-19-related in-hospital mortality. Secondary outcomes included rates of invasive mechanical ventilation (IMV) and intensive care unit (ICU) admission. Effect sizes from each study were computed as logarithmically transformed odds ratios (ORs) with random‐effects, Mantel‐Haenszel weighting. The between‐study variance component of random‐effects models was computed using restricted effects maximum likelihood estimation, and 95% confidence intervals (CIs) around pooled effect sizes were calculated using Hartung–Knapp adjustments. In total, 12,057 patients were included in the analysis, with 2,714 (22.5%) patients in the Hem group and 9,343 (77.5%) patients in the Tumor group. The overall unadjusted odds of all-cause mortality were 1.64 times higher in the Hem group compared to the Tumor group (95% CI: 1.30–2.09). This finding was consistent with multivariable models presented in moderate- and high-quality cohort studies, suggestive of a causal effect of cancer type on in-hospital mortality. Additionally, the Hem group had increased odds of COVID-19-related mortality compared to the Tumor group (OR = 1.86 [95% CI: 1.38–2.49]). There was no significant difference in odds of IMV or ICU admission between cancer groups (OR = 1.13 [95% CI: 0.64–2.00] and OR = 1.59 [95% CI: 0.95–2.66], respectively). Cancer is a serious comorbidity associated with severe outcomes in COVID-19 patients, with especially alarming mortality rates in patients with hematological malignancies, which are typically higher compared to patients with solid tumors. A meta-analysis of individual patient data is needed to better assess the impact of specific cancer types on patient outcomes and to identify optimal treatment strategies.
Similar content being viewed by others
Introduction
As of May 2022, the COVID-19 pandemic has been the cause of 6.3 million deaths worldwide and over one million deaths in the USA [1]. Research efforts have established that patients with comorbidities and chronic diseases are at higher risk of contracting the virus and experiencing severe COVID-19 illness [2, 3]. Cancer patients are particularly at risk; various studies have found that those with cancer have 2.06 times the odds of severe COVID-19 and 3.04 times the odds of mortality compared to those without cancer [4, 5], possibly due to their immunocompromised status, immunosuppressive cancer treatments, or comorbidities [6,7,8]. However, it is not clear as to whether and to what extent their immunocompromised status and immunotherapy treatments are deleterious [9, 10]. International consortiums (e.g., European Society for Medical Oncology) and individual institutions (e.g., Johns Hopkins) have developed some treatment guidelines for cancer patients during the COVID-19 pandemic [11, 12], but care for these patients suffers from persistent knowledge gaps and an incomplete literature.
Evidence also indicates that COVID-19 may affect patients differently depending on cancer type. Several reports have shown that patients with hematologic, lung, or metastatic malignancies may be more vulnerable to severe COVID-19 or fatality [13,14,15], but pooled evidence on this topic is limited, and to our knowledge, there have been no meta-analyses that have directly compared solid tumors to hematological malignancies. This systematic review and meta-analysis examined all-cause mortality, COVID-19-related mortality, ICU admission, and invasive mechanical ventilation in patients with hematological malignancies versus solid tumors primarily to provide quantitative evidence to strengthen current and future guidelines for patients with hematological cancers and secondarily to contribute concrete evidence for current clinical trials to provide patient-level, cancer subtype breakdowns in their data collection and analyses to allow for even more robust meta-analyses in the future.
Methods
Study design and search
This study was performed in compliance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [16]. A PRISMA checklist is provided in Additional File 1. A systematic search of the PubMed and Embase databases was conducted using Nested Knowledge research software (Nested Knowledge, St Paul, MN). Search strings are shown in Additional File 2, Table S1.
Inclusion/exclusion criteria
Unique studies that resulted from these queries were initially screened by the Nested Knowledge automatic exclusion software for the following exclusion criteria: (1) not published in English; (2) published before February 1, 2020; and (3) title includes: “Case report.” Following automatic exclusion, title/abstract review was performed by several authors and was supervised by N.H. The remaining articles then underwent full-text review to determine inclusion (see Additional File 3 for details on the screening protocol).
Articles were eligible for inclusion if they included direct comparisons of the primary outcomes of interest in adult COVID-19 patients with hematological malignancies (Hem) versus solid tumors (Tumor). Exclusion criteria were studies not published in English, non-human studies, case series or case reports, meta-analyses, editorials or letters to the editor, interim reports, protocols or technical articles, did not compare hematological malignancies and solid tumor groups, did not report in-hospital mortality, or not relevant to the topic.
Data extraction
The data extraction workflow was supervised by N.H., with data extraction performed by several authors. The quality of data was validated a second time by J.M.P. prior to statistical analysis (see Additional File 3 for a detailed description of the data extraction process). Baseline characteristics collected included age, sex, comorbidities (cerebrovascular disease, chronic obstructive pulmonary disease [COPD], coronary artery disease, diabetes, hypertension, kidney disease, liver disease), type of hematological cancer (leukemia, lymphoma, multiple myeloma, myelodysplastic syndrome, other/unspecified), cancer status (active, relapsed/refractory, remission), and active chemotherapy (meaning treatment within the last 3 months). Patients were categorized into either the hematological malignancy group (Hem) or the solid tumors group (Tumor). The primary outcomes of interest were 1) all-cause, in-hospital mortality and 2) COVID-19-related, in-hospital mortality. Secondary outcomes included invasive mechanical ventilation (IMV) and intensive care unit (ICU) admission.
Risk of bias
The Newcastle–Ottawa scale (NOS) for cohort studies was used to assess the risk of bias of the included studies [17]. Two independent reviewers (J.T. and P.O.) completed the risk of bias assessments for each study, and a third reviewer (J.M.P.) resolved any disagreements that occurred. The risk of bias was classified as low, moderate, or high based on the NOS scores, as follows: low risk of bias requires 3 or 4 stars in selection, 1 or 2 stars in comparability, and 2 or 3 stars in outcomes; moderate risk of bias requires 2 stars in selection, 1 or 2 stars in comparability, and 2 or 3 stars in outcomes, high risk of bias has 0 or 1 star(s) in selection, or 0 stars in comparability, or 0 or 1 star(s) in outcomes.
Statistical analysis
All data were extracted using the Nested Knowledge interface. Extracted data were downloaded as a.csv file and imported as a Microsoft Excel sheet to RStudio (Version 1.4.1717, RStudio, PBC) running on R‐4.0.2 for analysis using the “meta” [18] and “metafor” [19] packages. J.M.P. established the statistical analysis plan and R script used for analysis.
Effect sizes from each study were computed as logarithmically transformed odds ratios (ORs) with random‐effects, Mantel‐Haenszel weighting. The between‐study variance component of random‐effects models was estimated using restricted effects maximum likelihood with 95% confidence intervals (CIs) computed using the Q‐profile method [20]. 95% CIs around pooled effect sizes were calculated using Knapp-–Hartung adjustments [21] to provide a more conservative estimate of the true effect of cancer type on outcomes and to reduce the risk of false positives. 95% prediction intervals (PIs) were also computed in order show where effect sizes would be expected to lie within 95% of similar (i.e., exchangeable) studies [22]. For each aggregated result, I2 statistics were used to measure the percentage of the total variability in effect estimates that can be attributed to heterogeneity rather than sampling error [23]. Qualitatively, I2 values of < 25%, 25% to 75%, and > 75% were considered low, moderate, and high levels of between‐study variability in effect estimates, respectively. Although planned in the original protocol (Additional File 3), this review does not include comparative subgroup analyses of the specific cancer type (for example chronic lymphocytic leukemia [CLL] vs. chronic myeloid leukemia [CML]) due to insufficient data.
Importantly, this systematic review included non-randomized and retrospective studies. As such, analyses may be impacted by residual and unobserved confounding, implying that pooled results may not reflect causal effects. Qualitative synthesis was performed with moderate- and high-quality studies providing robust multivariable and matched cohort analyses in order to evaluate the robustness of the pooled results and to investigate potential sources of heterogeneity.
Results
Search results
A total of 649 records were identified by the search, with an additional 41 added via expert recommendation; after removing duplicates, 623 articles remained. Based on title/abstract review, 418 articles were excluded, leaving 205 articles for full-text review. Ultimately, 23 cohort studies were included in this study [14, 24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45]. A PRISMA diagram of study attrition with reasons for exclusion is shown in Fig. 1.
Risk of bias assessment
After performing the risk of bias assessment, 17.4% (4/23) of studies were deemed to have low risk of bias [26, 33, 43, 44], 17.4% (4/23) had a moderate risk of bias [25, 30, 32, 42], and 65.2% (15/23) had a high risk of bias [14, 24, 27,28,29, 31, 34,35,36,37,38,39,40,41, 45]. All studies were ultimately recommended for inclusion. Study-level details on the risk of bias assessment can be found in Additional File 2, Table S2.
Baseline characteristics
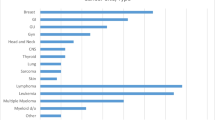
Overall, 12,057 patients were included in this systematic review; 22.5% (2,714/12,057) of patients were in the Hem group, and 77.5% (9,343/12,057) of patients were in the Tumor group. At the individual study level, mean age was generally comparable between Hem and Tumor groups, though Hem patients predictably skewed younger. Sex ratios were also generally balanced, with obvious sex-dependent exceptions in the Tumor groups (i.e., breast and prostate cancer). Study-level demographic information and baseline characteristics by cancer type are shown in Table 1. A detailed record of cancer subtypes (e.g., Hodgkin’s and non-Hodgkin’s lymphoma) and number of affected patients per study is provided in Additional File 2, Table S3. Study-level patient comorbidities, cancer status, and chemotherapy treatment are shown in Additional File 2, Table S4.
Primary outcomes
All-cause mortality
Twenty-one studies reported data on all-cause mortality [14, 24,25,26,27,28,29,30,31,32,33,34,35,36, 39,40,41,42,43,44,45]. Of these, 4 studies were associated with a low risk of bias, 4 were associated with a moderate risk of bias, and 13 were associated with a high risk of bias. The overall unadjusted mortality rate for the Hem group was 41.4% (95% CI: 36.4–46.7%), and for the Tumor group, it was 29.7% (95% CI: 23.3–37.1%). Overall, the odds of all-cause mortality for the Hem group were 1.64 times as likely as the Tumor group (95% CI: 1.30–2.09; Fig. 2). The studies were largely consistent. Of 21 studies, 16 reported the Hem group as having a higher mortality rate, while 5/21 studies reported the Tumor group as having a higher mortality rate. However, differences in mortality rates between groups may have been impacted by residual confounding, as there were insufficient data to account for imbalances in important covariates between groups. Between-study statistical heterogeneity in effect estimates was moderate, with an estimated 55.8% of the variability being attributable to heterogeneity rather than sampling error according to the I2 statistic (95% CI: 27.9–72.9%).
Effect sizes were computed using the Mantel–Haenszel method, using restricted effects maximum likelihood estimation of the between-study variance component. The Hartung–Knapp adjustment was used for computing a 95% CI around the pooled effect size. A 95% PI for the pooled results is also displayed, showing where the expected effect size would lie in 95% of similar (i.e., exchangeable) studies. Overall, results show that the odds of all-cause mortality are 1.64 times as likely in the Hem group compared to the Tumor group (95% CI: 1.30–2.09), with moderate estimated statistical inconsistency between studies (I2 = 55.8% [95% CI: 27.9–72.9%]).
Hem = hematological malignancies; Tumor = solid tumors; CI = confidence interval; OR = odds ratio; and PI = prediction interval.
Of the 6 studies that provided multivariable analyses of direct or indirect comparisons of cancer type (Hem vs. Tumor) with respect to all-cause mortality [25, 26, 30, 32, 33, 42], all studies suggested an underlying difference in risk of mortality between groups, with the directionality of effect sizes tending to favor patients with solid tumors compared to patients with hematological malignancies; however, only two studies showed a significant difference at the α = 0.05 level [26, 32]. Due to differences in statistical methods and difficulty in obtaining key methodological details, data from multivariable analyses were not combined across studies to obtain a pooled, adjusted all-cause mortality rate. Findings from each of these studies are provided in turn below (see Additional File 2, Table S5 for details on study-level outcome comparisons).
Study-level all-cause mortality findings
Bhogal et al. conducted a multicenter retrospective chart review from six centers in the UK, identifying 179 cancer patients with COVID-19 (Hem: n = 52; Tumor: n = 127) [26]. After fitting a multivariable Cox regression model adjusted for age, platelet count, and C-reactive protein (CRP) level, results showed an overall higher instantaneous risk of mortality in the Hem group compared to the Tumor group (hazard ratio [HR] = 2.94 [95% CI: 1.59–5.59], p < 0.001). This study was deemed to be associated with a low risk of bias.
Fu et al. performed a multicenter retrospective chart review that included 233 COVID-19 patients with active cancer (Hem: n = 69, Tumor: n = 164). From a multivariable logistic regression adjusted for age, sex, race, obesity, D-dimer levels, and cancer treatment (no treatment vs. chemotherapy treatment in the past 3 months vs. other treatment), there was no statistically significant difference in odds of mortality between patients with hematological malignancies and solid tumors, although the directionality of the effect estimate favored patients with solid tumors (OR = 1.82 [95% CI: 0.88–3.77], p = 0.11) [29]. This study was deemed to be associated with a moderate risk of bias.
Hermel et al. performed a multicenter observational study of 246 cancer patients (Hem: n = 37, Tumor: n = 209) hospitalized for COVID-19. After performing a multivariable logistic regression analysis adjusted for age, sex, atrial fibrillation, deep vein thrombosis, and thrombocytopenia, the odds of mortality for patients with solid tumors were 0.54 times as likely as patients with hematological malignancies, but this difference was not statistically significant (OR = 0.54 [95% CI: 0.23–1.3], p = 0.157) [32]. This study was deemed to be associated with a moderate risk of bias.
Korkusuz et al. performed a single-center retrospective study of 282 cancer patients with confirmed diagnosis of COVID-19 (Hem: n = 43, Tumor: n = 239) [33]. After performing a multivariable logistic regression adjusted for tumor stage, chemotherapy use, computed tomography (CT) findings (mild, moderate, or severe), hypertension, and ICU admission, results showed that the odds of mortality for patients with solid tumors were 0.151 times as likely as patients with hematological malignancies (OR = 0.151 [95% CI: 0.036–0.638], p = 0.010). This study was deemed to be associated with a low risk of bias.
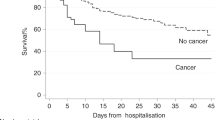
Plais et al. performed a multicenter ambidirectional study (data were collected retrospectively 3/12/2020–1/4/2021 and prospectively 1/4/2021–3/4/2021) to compare outcomes of COVID-19 patients requiring organ support [42]. Patients with and without cancer were matched at a 1:3 ratio from a larger sample (n = 2,608) using an inverse probability weighting approach based on a propensity score assessing the probability of cancer at admission. After patient matching, a sample of 420 patients was achieved (No cancer: n = 315, Hem: n = 51, Tumor: n = 54). After performing multivariable logistic regression on the matched cohort and adjusting for age at admission (dichotomized as > 70 vs. ≤ 70 years), hydroxychloroquine + azithromycin combination treatment, antimicrobial treatment, admission after 8/1/2020, and norepinephrine use, results showed that both the Hem and the Tumor group were associated with increased odds of mortality compared to the No cancer group (OR = 4.144 [95% CI: 1.24–13.83] and OR = 2.344 [95% CI: 0.87–6.31], respectively). Although this study was not specifically designed to compare mortality rates between the Hem and the Tumor group, the directionality and magnitude of the effects relative to the No cancer group may suggest that patients with hematological malignancies are at a higher risk of mortality compared to patients with solid tumors. This study was deemed to be associated with a moderate risk of bias.
Findings from Bernard et al. suggested that patients with metastatic solid tumors have increased odds of all-cause mortality compared to those with hematological malignancies while solid tumors without metastasis have decreased odds of all-cause mortality [25]. Based on a multivariable logistic regression model from data from 15,104 patients and adjusted for sex, dementia, heart failure, COPD, cirrhosis, diabetes, anemia, and pulmonary bacterial infection, patients with hematological cancers, solid cancers without metastasis, and solid cancers with metastasis all showed to have increased odds of all-cause mortality compared to patients without cancer, but solid cancers with metastasis showed the largest difference relative to patients without cancer (OR = 2.2 [95% CI: 2.0–2.5], OR = 1.4 [95% CI: 1.3–1.5], and OR = 3.6 [95% CI: 3.2–4.0], respectively). This study was deemed to be associated with a moderate risk of bias.
COVID-19-related mortality
Only 5 studies specifically reported on COVID-19-related in-hospital mortality, and they were consistent in reporting hematological malignancy as having a higher mortality rate compared to solid tumor [31, 36,37,38, 40]. All studies included in the analysis of COVID-19-related mortality were deemed to be associated with a high risk of bias. The overall unadjusted COVID-19-related mortality rate for the Hem group was 36.5% (95% CI: 26.3–48.1%), and for the Tumor group, it was 23.8% (95% CI: 18.6–29.9%). Overall, the odds of COVID-19-related mortality were higher in the Hem group compared to the Tumor group (OR = 1.86 [95% CI: 1.38–2.49]; Fig. 3). Although effect size estimates of the observed studies were roughly homogenous, the predicted between-study statistical heterogeneity is imprecisely estimated due to limited study data (I2 = 0.0% [95% CI: 0.0–79.2%]). None of the studies included in this review provided robust multivariable or matched cohort analyses explicitly comparing COVID-19-related mortality between the Hem group and the Tumor group, thus making it difficult to make inferences about any underlying difference attributable to cancer type. See Additional File 2, Table S6 for details on study-level outcome comparisons.
Effect sizes were computed using the Mantel–Haenszel method, using restricted effects maximum likelihood estimation of the between-study variance component. The Hartung–Knapp adjustment was used for computing a 95% CI around the pooled effect size. A 95% PI for the pooled results is also displayed, showing where the expected effect size would lie in 95% of similar (i.e., exchangeable) studies. Overall, results show that the odds of COVID-19-related mortality are 1.86 times as likely in the Hem group compared to the Tumor group (95% CI: 1.38–2.49), with low to moderate estimated statistical inconsistency between studies (I2 = 0.0% [95% CI: 0.0–79.2%]).
Hem = hematological malignancies; Tumor = solid tumors; CI = confidence interval; OR = odds ratio; and PI = prediction interval.
Secondary outcomes
Invasive mechanical ventilation (IMV)
Seven studies had sufficient data to compare IMV rates between groups [14, 32, 37, 40,41,42, 45]. Of these, 2 were associated with a moderate risk of bias and 5 were associated with a high risk of bias. The studies were inconsistent. Of seven studies, four reported the Hem group as having a higher risk of IMV compared to the Tumor group. The overall IMV rate for the Hem group was 15.3% (95% CI: 8.5–26.1%), and for the Tumor group, it was 11.4% (95% CI: 6.3–19.8%). Overall, the odds of IMV were higher in the Hem group compared to the Tumor group, but this difference was not statistically significant (OR = 1.13 [95% CI: 0.64–2.00]; Fig. 4). The estimated between-study statistical heterogeneity in effect estimates ranged from low to high (I2 = 12.5% [95% CI: 0.0–77.8%]) and is imprecisely estimated due to the limited study data.
Effect sizes were computed using the Mantel–Haenszel method, using restricted effects maximum likelihood estimation of the between-study variance component. The Hartung–Knapp adjustment was used for computing a 95% CI around the pooled effect size. A 95% PI for the pooled results is also displayed, showing where the expected effect size would lie in 95% of similar (i.e., exchangeable) studies. Overall, results show that the odds of COVID-19-related mortality are 1.13 times as likely in the Hem group, but this difference was not statistically significant (95% CI: 0.64–2.00) and there were low to high levels of statistical inconsistency between studies (I2 = 12.5% [95% CI: 0.0–77.8%]).
IMV = invasive mechanical ventilation; Hem = hematological malignancies; Tumor = solid tumors; CI = confidence interval; OR = odds ratio; and PI = prediction interval.
Only one study included in the review provided a multivariable analysis that explicitly compared IMV rates between the Hem group and the Tumor group. After performing a multivariable logistic regression analysis adjusted for anemia, Hermel et al. showed that there was no significant difference in odds of IMV between patients with hematological malignancies and solid tumors (OR = 1.22 [95% CI: 0.44–4.02]) [32]. See Additional File 2, Table S7 for details on study-level outcome comparisons.
Admission to intensive care unit (ICU)
Eleven studies had sufficient data to compare ICU admission rates between groups [14, 25, 26, 30,31,32, 35, 37, 41, 43, 45]. Of these studies, 2 were associated with a low risk of bias, 3 were associated with a moderate risk of bias, and 6 were associated with a high risk of bias. The rates of ICU admission were largely consistent between studies with 8/11 reporting increased rates for the Hem group compared to the Tumor group. The overall ICU admission rate for the Hem group was 18.9% (95% CI: 12.6–27.3%), and for the Tumor group, it was 12.9% (95% CI: 9.7–16.9%). Overall, the odds of ICU admission were higher in the Hem group compared to the Tumor group, but this difference was not statistically significant (OR = 1.59 [95% CI: 0.95–2.66]; Fig. 5) and had a wide range of expected effects in 95% of exchangeable studies (95% PI: 0.43–5.92). The estimated between-study heterogeneity in effect estimates ranged from moderate to high (I2 = 67.4% [95% CI: 38.6–82.7%]). See Additional File 2, Table S7 for details on study-level outcome comparisons.
Only one study included in the review provided a multivariable analysis explicitly comparing ICU admission rates between the Hem group and the Tumor group. Hermel et al. did not find a significant difference in odds of ICU admission between patients with hematological malignancies and solid tumors after performing a multivariable logistic regression adjusted for anemia, asthma, and ethnicity [32].
Effect sizes were computed using the Mantel–Haenszel method, using restricted effects maximum likelihood estimation of the between-study variance component. The Hartung–Knapp adjustment was used for computing a 95% CI around the pooled effect size. A 95% PI for the pooled results is also displayed, showing where the expected effect size would lie in 95% of similar (i.e., exchangeable) studies. Overall, results show that the odds of COVID-19-related mortality are 1.59 times as likely in the Hem group compared to the Tumor group, but this difference was not statistically significant (95% CI: 0.95–2.67) and there were moderate to high levels of statistical inconsistency between studies (I2 = 67.4% [95% CI: 38.6–82.7%]).
ICU = intensive care unit; Hem = hematological malignancies; Tumor = solid tumors; CI = confidence interval; OR = odds ratio; and PI = prediction interval.
Additionally, Rugge et al. compared ICU admission across several cancer subtypes in 823 patients with available data from a population-based study in northeastern Italy [43]. After performing a multivariable logistic regression adjusted for age, sex, and comorbidities (none vs. respiratory vs. others), there was no significant difference in ICU admission rates between patients without cancer, breast cancer, colorectum cancer, prostate cancer, urinary/bladder cancer, lung cancer, hematological cancers, or other cancer types. However, this study was not designed to make inferences about overall ICU admission rates between the two cancer groups of interest.
Discussion
This systematic review and meta-analysis of 12,057 cancer patients with COVID-19 found that patients with hematological malignancies had significantly higher odds of all-cause mortality and COVID-19-related mortality compared to those with solid tumors. Patients with hematological malignancy tended to have higher odds of IMV and admission to the ICU, though these differences were not significant. Nearly all included studies that provided multivariable analyses of all-cause mortality were in agreement that hematological malignancy placed patients at higher risk compared to solid tumors; for other outcomes, there were limited and lower quality analyses available at the individual study level. The current study provides a thorough inventory of the current literature on cancer and COVID-19 and offers substantial evidence that hematological malignancy is a greater hazard for patients with COVID-19 compared to solid tumors.
This meta-analysis fills a gap in the literature by comparing mortality for patients with hematological versus solid cancers. Earlier meta-analyses have simply described in-hospital mortality rates for segments of this patient population; one meta-analysis of 3,377 hematological cancer patients with COVID-19 found that mortality occurred in 34% of cases (95% CI: 28–39%) [46], and another meta-analysis of solely hematological cancer patients (N = 2,395) found that mortality was 21.3% [47]. A large survey study (N = 3,801) by the European Hematology Association reported that all-cause mortality for hematological cancer patients was 31.2% [48]. These all-cause mortality rates are slightly lower but generally comparable to those observed in this meta-analysis.
A small handful of previous meta-analyses have included indirect comparisons of hematological and solid cancer patients with COVID-19, but with much smaller sample sizes and without a focus on all-cause or COVID-19-related mortality. In a meta-analysis of 15 studies with 3,019 patients, Zhang et al. described univariate analyses of a composite outcome (death or IMV or ICU admission) for lung cancer versus other solid cancers, as well as for hematological cancer versus lung cancer, and found that neither of these groups differed significantly [49]. However, it should be noted that these groupings do not reflect the categories in the current review, and that multiple studies have previously identified lung cancer specifically and hematological cancer as placing patients at significantly higher risk for severe COVID-19 [13, 14]. Another meta-analysis by Liu et al. included 29 studies with 5,121 cancer patients and reported that patients with hematological malignancy had significantly increased mortality if administered chemotherapy compared to those that did not receive chemotherapy (Relative Risk [RR]: 2.68, 95% CI: 1.90–3.78), but patients with solid tumors saw no difference in mortality based on chemotherapy treatment (RR: 1.16, 95% CI: 0.57–2.36) [50]. However, they did not directly compare mortality for hematological versus solid cancers.
While the mechanism of action is unclear, it is possible that the hematological manifestations of COVID-19 interact with the hematological cancer disease state to result in worse outcomes for these patients. COVID-19 is known to cause leukopenia, lymphopenia, and thrombocytopenia in those infected, which contribute to a prothrombotic state and can serve as predictors of patient outcome [51]. D-dimer levels are also associated with thrombosis, and studies have shown that underlying cancer may elevate D-dimer levels for patients with COVID-19, increasing likelihood of severe illness or mortality [52]. Furthermore, evidence shows that hematological cancer patients have a significantly lower seroconversion rate following COVID-19 vaccination compared to those with solid tumors [53], suggesting a weaker immune response upon infection with COVID-19. Additional research on the pathophysiology of COVID-19 is needed so that cancer patients and the general population can be better protected from serious illness.
Eight studies included in this review provided further analysis by reporting mortality solid cancers with versus without metastasis; advanced metastatic disease was often associated with worse outcomes, though only two studies found differences in outcomes to be significant. In their multicenter study of 105 cancer patients and 536 age-matched non-cancer patients, Dai et al. found that patients with metastatic cancer had significantly higher rates of mortality (OR: 5.58 [95% CI: 1.71–18.23]), IMV (OR: 55.42 [95% CI: 13.21–232.47]), and ICU admission (OR: 6.59 [95% CI: 2.32–18.72]) compared to those with non-metastatic cancer [14]. Similarly, Liang et al. reported that a significantly higher proportion of deceased patients had metastatic cancer compared to those who survived (52.1% vs. 12.3%, p < 0.001) [36]. Some researchers have hypothesized mechanisms linking COVID-19 infection and metastatic tumor response, saying that inflammasome activation, interleukin-1β production, impaired T-cell functioning, and high cytokine levels due to COVID-19 may worsen metastasis [54, 55].
By contrast, the remaining studies that investigated metastasis did not find significant associations with mortality based on solid tumor disease progression, or they did not provide direct comparisons [25, 31, 32, 37, 41, 44]. For example, Bernard et al. reported the highest odds of mortality for patients with solid, metastatic cancer (OR = 3.6 [95% CI: 3.2–4.0]), followed by patients with hematological cancers (OR = 2.2 [95% CI: 2.0–2.5]), and the lowest odds for patients with solid, non-metastatic cancer (OR = 1.4 [95% CI: 1.3–1.5]) compared to those without cancer, but they did not provide any direct comparisons of these groups [25]. Given the mixed evidence around metastasis and COVID-19 outcomes, further study on this topic is needed.
Moving forward, it is unclear what treatment plans result in the best outcomes for cancer patients with COVID-19. Many meta-analyses have found that administration of anticancer therapies (including chemotherapy, surgery, immunotherapy, targeted therapy, and/or radiotherapy) does not significantly affect mortality rates or severe COVID-19 for cancer patients as a whole [46, 50, 56,57,58]. However, when chemotherapy alone is considered, just as many studies have found that active or recent chemotherapy (within 28–30 days of COVID-19 onset) is associated with significantly increased risk of mortality, though not severe COVID-19 [50, 58,59,60,61]. Additionally, there are studies that suggest a potential positive effect of check point inhibitors (CPIs) on mortality compared to those not receiving anticancer therapy [44]. There are plausible biological mechanisms for all these relationships. For example, the association between improved outcome and CPI may be that CPI enhances antiviral T-cell immunity without increasing inflammation [62]. It has been shown that CD8 + T-cells are important for combating viral infections. Therefore, enhancement of CD8 + T-cells would be beneficial for someone with cancer and COVID [63]. Conversely, CPI may be associated with worse outcomes due to its potential ability to amplify the immune system to a point where it is pathologic [64]. Although it is generally understood the mechanism by which CPIs work, it is still unclear in what context their use will lead to immune dysregulation or improved immune response.
The complexities of CPIs and their use during illness with COVID is augmented by the intricacy of the innate and adaptive immune response to COVID. It has been shown that type 1 interferon signaling pathways are perhaps responsible for the increased immune response for those with severe COVID [65]. Additionally, it has been shown that when administered early in the course of illness, interferons (IFNs) can have a protective effect. However, if administered too late in the course of the illness, IFNs can augment the immune response and result in immunopathology [66]. In a similar fashion, type 1 IFN’s role in cancer is quite complicated. There are mechanisms by which type I IFNs may both favor tumor regression and tumor progression [9]. For example, type I IFNs may upregulate PD-L1 signals, which can then inhibit T-cell destruction of tumor cells. This will lead to tumor progression. However, if taking a CPI such as a PD-1/PD-L1 blockade, the upregulation of PD-L1 as an immune response to COVID will be foiled since the T-cells will still be able to destroy the tumor cells due to the PD-L1 blockade. In fact, for some cancers, the combination therapy of PD-L1/PD-1 blockade and a type I interferon inducer has been shown to increase effectiveness [67]. Conversely, type I IFNs have been shown to have a protective effect as they enhance survival of CD8 + cells which are imperative for managing viral infections. Therefore, the complexity of type I interferon in response to COVID is amplified by the complexity of both of their interactions with cancer, and the mixed evidence of the outcomes for using CPIs during COVID infection is concordant with the various possible mechanisms that CPI could impact the immune system in the specific context of cancer patients having a possible type 1 interferon mediated immune response to COVID.
Ultimately, treatment plans should be tailored to meet each patient’s unique needs and set of circumstances. To develop robust, evidence-based guidelines for different types of cancer and different types of patients, further study on this topic with individual patient data is needed. However, this meta-analysis does provide quantitative evidence that can strengthen current guidelines and strong support for clinical trials to provide cancer subtype breakdowns in their analyses.
Limitations and future directions
The major limitations of this systematic literature review include the retrospective nature of the included studies and inability to perform truly randomized studies. As such, it is difficult to make causal inferences about the impact of malignancy type on the clinical outcomes of interest. Additionally, there were limited study data regarding COVID-19-related mortality, mechanical ventilation, and ICU admission rates, possibly making pooled estimates of the overall population imprecise. This meta-analysis also does not include comparisons of specific malignancy types (e.g., metastatic breast cancer vs. chronic myeloid leukemia), and was only able to form pooled estimates from aggregated cancer groups. A meta-analysis of individual patient data is needed to more precisely assess the impact of the specific cancer types on patient outcomes, as well as to identify optimal treatment strategies across specific patient subsets. Beyond clinical trials providing patient-level data on cancer subtypes, new clinical trials should provide patient-level data on the genomic variation for cancers of the same site of origin and design their trials to stratify their enrollments that way as well. Cancer is a disease driven by genetic mutation and immune dysregulation, and the specific genetic mutation is imperative to testing and developing treatments. It a formidable challenge for clinical trials to be designed this way given the high cost and time commitment [68], and a limitation of this review is that more direction on the implementation of genomic directed stratification for clinical trials is not evident. However, the importance of genomic stratification in future clinical trials cannot be understated.
Conclusion
Cancer is a serious comorbidity which is associated with high rates of mortality and severe outcomes in COVID-19 patients. The odds of mortality are especially alarming in patients with hematological malignancies and are typically higher than patients with most types of solid tumors. A meta-analysis of individual patient data is needed in order to more precisely assess the impact of the specific cancer types on patient outcomes as well as to identify optimal treatment strategies across specific patient subsets.
Data availability
The dataset supporting the conclusions of this article is available online on the Nested Knowledge platform at https://nested-knowledge.com/nest/590.
Abbreviations
- CI:
-
Confidence interval
- COPD:
-
Chronic obstructive pulmonary disease
- Hem:
-
Hematological malignancy group
- HR:
-
Hazard ratio
- ICU:
-
Intensive care unit
- IMV:
-
Invasive mechanical ventilation
- OR:
-
Odds ratio
- PI:
-
Prediction interval
- Tumor:
-
Solid tumors group
References
COVID-19 dashboard by the center for systems science and engineering (CSSE) at Johns Hopkins University. In. Coronavirus resource center: Johns Hopkins University & Medicine. 2020
Singh AK, Gillies CL, Singh R, Singh A, Chudasama Y, Coles B, Seidu S, Zaccardi F, Davies MJ, Khunti K. Prevalence of co-morbidities and their association with mortality in patients with COVID-19: a systematic review and meta-analysis. Diabetes Obes Metab. 1915;22(10):2020.
Dessie ZG, Zewotir T. Mortality-related risk factors of COVID-19: a systematic review and meta-analysis of 42 studies and 423,117 patients. BMC Infect Dis. 2021;21(1):855.
Izcovich A, Ragusa MA, Tortosa F, Lavena Marzio MA, Agnoletti C, Bengolea A, Ceirano A, Espinosa F, Saavedra E, Sanguine V, Tassara A, Cid C, Catalano HN, Agarwal A, Foroutan F, Rada G. Prognostic factors for severity and mortality in patients infected with COVID-19: a systematic review. PLoS ONE. 2020;15(11): e0241955.
Parohan M, Yaghoubi S, Seraji A, Javanbakht MH, Sarraf P, Djalali M. Risk factors for mortality in patients with Coronavirus disease 2019 (COVID-19) infection: a systematic review and meta-analysis of observational studies. Aging Male. 2020;23(5):1416.
Yu J, Ouyang W, Chua MLK, Xie C. SARS-CoV-2 transmission in patients with cancer at a tertiary care hospital in Wuhan. China JAMA Oncol. 2020;6(7):1108.
Patel RH, Vanaparthy R, Greene JN. COVID-19 in immunocompromised cancer patients: a case series and review of the literature. Cancer Control. 2021;28:10732748211044360.
Gupta K, Gandhi S, Mebane A 3rd, Singh A, Vishnuvardhan N, Patel E. Cancer patients and COVID-19: mortality, serious complications, biomarkers, and ways forward. Cancer Treat Res Commun. 2021;26: 100285.
Musella M, Manic G, De Maria R, Vitale I, Sistigu A. Type-I-interferons in infection and cancer: unanticipated dynamics with therapeutic implications. Oncoimmunology. 2017;6(5): e1314424.
Goldman JD, Robinson PC, Uldrick TS, Ljungman P. COVID-19 in immunocompromised populations: implications for prognosis and repurposing of immunotherapies. J Immunother Cancer. 2021;9(6): 002630.
Sheng JY, Santa-Maria CA, Mangini N, Norman H, Couzi R, Nunes R, Wilkinson M, Visvanathan K, Connolly RM, Roussos Torres ET, Fetting JH, Armstrong DK, Tao JJ, Jacobs L, Wright JL, Thorner ED, Hodgdon C, Horn S, Wolff AC, Stearns V, Smith KL. Management of breast cancer during the COVID-19 pandemic: a stage- and subtype-specific approach. JCO Oncol Pract. 2020;16(10):665.
Curigliano G, Banerjee S, Cervantes A, Garassino MC, Garrido P, Girard N, Haanen J, Jordan K, Lordick F, Machiels JP, Michielin O, Peters S, Tabernero J, Douillard JY, Pentheroudakis G. Managing cancer patients during the COVID-19 pandemic: an ESMO multidisciplinary expert consensus. Ann Oncol. 2020;31(10):1320.
Jee J, Foote MB, Lumish M, Stonestrom AJ, Wills B, Narendra V, Avutu V, Murciano-Goroff YR, Chan JE, Derkach A, Philip J, Belenkaya R, Kerpelev M, Maloy M, Watson A, Fong C, Janjigian Y, Diaz LA Jr, Bolton KL, Pessin MS. Chemotherapy and COVID-19 outcomes in patients with cancer. J Clin Oncol. 2020;38(30):3538.
Dai M, Liu D, Liu M, Zhou F, Li G, Chen Z, Zhang Z, You H, Wu M, Zheng Q, Xiong Y, Xiong H, Wang C, Chen C, Xiong F, Zhang Y, Peng Y, Ge S, Zhen B, Yu T, Wang L, Wang H, Liu Y, Chen Y, Mei J, Gao X, Li Z, Gan L, He C, Li Z, Shi Y, Qi Y, Yang J, Tenen DG, Chai L, Mucci LA, Santillana M, Cai H. Patients with cancer appear more vulnerable to SARS-CoV-2: a multicenter study during the COVID-19 outbreak. Cancer Discov. 2020;10(6):783.
Lee LYW, Cazier JB, Starkey T, Briggs SEW, Arnold R, Bisht V, Booth S, Campton NA, Cheng VWT, Collins G, Curley HM, Earwaker P, Fittall MW, Gennatas S, Goel A, Hartley S, Hughes DJ, Kerr D, Lee AJX, Lee RJ, Lee SM, McKenzie H, Middleton CP, Murugaesu N, Newsom-Davis T, Olsson-Brown AC, Palles C, Powles T, Protheroe EA, Purshouse K, Sharma-Oates A, Sivakumar S, Smith AJ, Topping O, Turnbull CD, Várnai C, Briggs ADM, Middleton G, Kerr R. COVID-19 prevalence and mortality in patients with cancer and the effect of primary tumour subtype and patient demographics: a prospective cohort study. Lancet Oncol. 2020;21(10):1309.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372: n71.
Lo CK, Mertz D, Loeb M. Newcastle-ottawa scale: comparing reviewers’ to authors’ assessments. BMC Med Res Methodol. 2014;14:45.
Balduzzi S, Rucker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health. 2019;22(4):153.
Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. 2010;36(3):1.
van Aert RCM, van Assen M, Viechtbauer W. Statistical properties of methods based on the Q-statistic for constructing a confidence interval for the between-study variance in meta-analysis. Res Synth Methods. 2019;10(2):225.
Knapp G, Hartung J. Improved tests for a random effects meta-regression with a single covariate. Stat Med. 2003;22(17):2693.
Riley RD, Higgins JPT, Deeks JJ. Interpretation of random effects meta-analyses. BMJ. 2011;342: d549.
Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ (Clinical Research ed). 2003;327(7414):557.
Asghar K, Abu Bakar M, Akram MJ, Farooq A, Siddique K, Rana IA, Ali J, Rashid MU, Khan AA, Loya A. Clinical characteristics of COVID-19-infected cancer patients in Pakistan: differences between survivors and non-survivors. Front Oncol. 2021;11: 655634.
Bernard A, Cottenet J, Bonniaud P, Piroth L, Arveux P, Tubert-Bitter P, Quantin C. Comparison of cancer patients to non-cancer patients among COVID-19 inpatients at a national level. Cancers (Basel). 2021;13(6):1436.
Bhogal T, Khan UT, Lee R, Stockdale A, Hesford C, Potti-Dhananjaya V, Jathanna A, Rahman S, Tivey A, Shotton R, Sundar R, Valerio C, Norouzi A, Walker P, Suckling R, Armstrong A, Brearton G, Pettitt A, Kalakonda N, Palmer DH, Jackson R, Turtle L, Palmieri C. Haematological malignancy and nosocomial transmission are associated with an increased risk of death from COVID-19: results of a multi-center UK cohort. Leuk Lymphoma. 2021;62(7):1682.
Chai C, Feng X, Lu M, Li S, Chen K, Wang H, Wang W, Tang Z, Cheng G, Wu X, Li Y, Wen Y, Da B, Fan H, Wang L, Ai F, Li W, Peng C, Zhang H, Wen S, Zhang J, Weng Y, Tang Z. One-year mortality and consequences of COVID-19 in cancer patients: a cohort study. IUBMB Life. 2021;73(10):1244.
Dang MKM, Bhatt I, Dulu AO, Zhang H, Kostelecky N, Pastores SM. Clinical characteristics, management, and outcomes of cancer patients with coronavirus disease 2019 admitted to the ICU. Crit Care Explor. 2021;3(9): e0535.
De-la-Rosa-Martinez D, Aranda-Audelo M, Martin-Onraet A, Islas-Muñoz B, Perez-Jimenez C, Alatorre-Fernandez P, Cornejo-Juarez P, Ruiz-Garcia E, Zinser-Peniche P, Nuñez-Luna L, Meneses-Garcia A, Herrera-Gomez A, Vilar-Compte D. Clinical characteristics and outcomes in a cohort of oncologic patients with COVID-19 during the first year of the pandemic in Mexico. Cancer Med. 1827;11(8):2022.
Fu C, Stoeckle JH, Masri L, Pandey A, Cao M, Littman D, Rybstein M, Saith SE, Yarta K, Rohatgi A, Makarov DV, Sherman SE, Morrissey C, Jordan AC, Razzo B, Theprungsirikul P, Tsai J, Becker DJ. COVID-19 outcomes in hospitalized patients with active cancer: experiences from a major New York City health care system. Cancer. 2021;127(18):3466.
Goudsmit A, Cubilier E, Meert AP, Aftimos P, Stathopoulos K, Spilleboudt C, Loizidou A. Factors associated with SARS-CoV-2 infection and outcome in patients with solid tumors or hematological malignancies: a single-center study. Support Care Cancer. 2021;29(11):6271.
Hermel DJ, Cham J, Spierling Bagsic SR, Hong LK, Costantini CL, Mason JR, Saven A, Sigal DS. An observational study of hospitalized COVID-19 patients with cancer in San Diego county. Future Oncol. 2022;18(6):719.
Korkusuz R, Sahingoz Erdal G, Kibar Akilli I, Bilge M, Tural D, Kart YK. Changing characteristics of cancer patients during the COVID-19 pandemic. J Infect Dev Ctries. 2022;16(3):453.
Kumar R, Patel N, Kodan P, Aggarwal R, Dass C, Soni KD, Trikha A. Clinical profile and outcome of critically Ill COVID-19 patients with malignancy admitted in intensive care unit of a tertiary COVID center. India Cureus. 2021;13(7): e16553.
Li Q, Chen L, Li Q, He W, Yu J, Chen L, Cao Y, Chen W, Di W, Dong F, Cai L, Ran Q, Li L, Liu Q, Ren W, Gao F, Wang H, Chen Z, Gale RP, Hu Y. Cancer increases risk of in-hospital death from COVID-19 in persons <65 years and those not in complete remission. Leukemia. 2020;34(9):2384.
Liang J, Jin G, Liu T, Wen J, Li G, Chen L, Wang W, Wang Y, Liao W, Song J, Ding Z, Chen XP, Zhang B. Clinical characteristics and risk factors for mortality in cancer patients with COVID-19. Front Med. 2021;15(2):264.
Mehta V, Goel S, Kabarriti R, Cole D, Goldfinger M, Acuna-Villaorduna A, Pradhan K, Thota R, Reissman S, Sparano JA, Gartrell BA, Smith RV, Ohri N, Garg M, Racine AD, Kalnicki S, Perez-Soler R, Halmos B, Verma A. Case fatality rate of cancer patients with COVID-19 in a New York hospital system. Cancer Discov. 2020;10(7):935.
Meng Y, Lu W, Guo E, Liu J, Yang B, Wu P, Lin S, Peng T, Fu Y, Li F, Wang Z, Li Y, Xiao R, Liu C, Huang Y, Lu F, Wu X, You L, Ma D, Sun C, Wu P, Chen G. Cancer history is an independent risk factor for mortality in hospitalized COVID-19 patients: a propensity score-matched analysis. J Hematol Oncol. 2020;13(1):75.
Monari C, Sagnelli C, Maggi P, Sangiovanni V, Numis FG, Gentile I, Masullo A, Rescigno C, Calabria G, Megna AS, Gambardella M, Manzillo E, Russo G, Esposito V, Camaioni C, Messina V, Pisaturo M, Allegorico E, Pinchera B, Pisapia R, Catalano M, Salzillo A, Porta G, Signoriello G, Coppola N. More severe COVID-19 in patients with active cancer: results of a multicenter cohort study. Front Oncol. 2021;11: 662746.
Nakamura S, Kanemasa Y, Atsuta Y, Fujiwara S, Tanaka M, Fukushima K, Kobayashi T, Shimoyama T, Omuro Y, Sekiya N, Imamura A. Characteristics and outcomes of coronavirus disease 2019 (COVID-19) patients with cancer: a single-center retrospective observational study in Tokyo. Japan Int J Clin Oncol. 2021;26(3):485.
Nomoto H, Suzuki S, Asai Y, Hayakawa K, Gatanaga H, Terada M, Suzuki K, Ohtsu H, Toyoda A, Ohmagari N. Clinical characteristics and prognosis of immunosuppressed inpatients with COVID-19 in Japan. J Infect Chemother. 2022;28(2):224.
Plais H, Labruyère M, Creutin T, Nay P, Plantefeve G, Tapponnier R, Jonas M, Ngapmen NT, Le Guennec L, De Roquetaillade C, Argaud L, Jamme M, Goulenok C, Merouani K, Leclerc M, Sauneuf B, Shidasp S, Stoclin A, Bardet A, Mir O, Ibrahimi N, Llitjos JF. Outcomes of patients with active cancer and COVID-19 in the intensive-care unit: a multicenter ambispective study. Front Oncol. 2022;12: 858276.
Rugge M, Zorzi M, Guzzinati S, Stocco C, Avossa F, Del Zotto S, Clagnan E, Bricca L, Dal Maso L, Serraino D. Outcomes of SARS-CoV-2 infection in cancer versus non-cancer-patients: a population-based study in northeastern Italy. Tumori. 2022. https://doi.org/10.1177/03008916211073771.
Várnai C, Palles C, Arnold R, Curley HM, Purshouse K, Cheng VWT, Booth S, Campton NA, Collins GP, Hughes DJ, Kulasekararaj AG, Lee AJX, Olsson-Brown AC, Sharma-Oates A, Van Hemelrijck M, Lee LYW, Kerr R, Middleton G, Cazier JB. Mortality among adults with cancer undergoing chemotherapy or immunotherapy and infected With COVID-19. JAMA Netw Open. 2022;5(2): e220130.
Yang K, Sheng Y, Huang C, Jin Y, Xiong N, Jiang K, Lu H, Liu J, Yang J, Dong Y, Pan D, Shu C, Li J, Wei J, Huang Y, Peng L, Wu M, Zhang R, Wu B, Li Y, Cai L, Li G, Zhang T, Wu G. Clinical characteristics, outcomes, and risk factors for mortality in patients with cancer and COVID-19 in Hubei, China: a multicentre, retrospective, cohort study. Lancet Oncol. 2020;21(7):904.
Vijenthira A, Gong IY, Fox TA, Booth S, Cook G, Fattizzo B, Martín-Moro F, Razanamahery J, Riches JC, Zwicker J, Patell R, Vekemans MC, Scarfò L, Chatzikonstantinou T, Yildiz H, Lattenist R, Mantzaris I, Wood WA, Hicks LK. Outcomes of patients with hematologic malignancies and COVID-19: a systematic review and meta-analysis of 3377 patients. Blood. 2020;136(25):2881.
Naimi A, Yashmi I, Jebeleh R, Imani Mofrad M, Azimian Abhar S, Jannesar Y, Heidary M, Pakzad R. Comorbidities and mortality rate in COVID-19 patients with hematological malignancies: a systematic review and meta-analysis. J Clin Lab Anal. 2022;36(5): e24387.
Pagano L, Salmanton-García J, Marchesi F, Busca A, Corradini P, Hoenigl M, Klimko N, Koehler P, Pagliuca A, Passamonti F, Verga L, Víšek B, Ilhan O, Nadali G, Weinbergerová B, Córdoba-Mascuñano R, Marchetti M, Collins GP, Farina F, Cattaneo C, Cabirta A, Gomes-Silva M, Itri F, van Doesum J, Ledoux M-P, Čerňan M, Jakšić O, Duarte RF, Magliano G, Omrani AS, Fracchiolla NS, Kulasekararaj A, Valković T, Poulsen CB, Machado M, Glenthøj A, Stoma I, Ráčil Z, Piukovics K, Navrátil M, Emarah Z, Sili U, Maertens J, Blennow O, Bergantim R, García-Vidal C, Prezioso L, Guidetti A, Del Principe MI, Popova M, de Jonge N, Ormazabal-Vélez I, Fernández N, Falces-Romero I, Cuccaro A, Meers S, Buquicchio C, Antić D, Al-Khabori M, García-Sanz R, Biernat MM, Tisi MC, Sal E, Rahimli L, Čolović N, Schönlein M, Calbacho M, Tascini C, Miranda-Castillo C, Khanna N, Méndez G-A, Petzer V, Novák J, Besson C, Duléry R, Lamure S, Nucci M, Zambrotta G, Žák P, Seval GC, Bonuomo V, Mayer J, López-García A, Sacchi MV, Booth S, Ciceri F, Oberti M, Salvini M, Izuzquiza M, Nunes-Rodrigues R, Ammatuna E, Obr A, Herbrecht R, Núñez-Martín-Buitrago L, Mancini V, Shwaylia H, Sciumè M, Essame J, Nygaard M, Batinić J, Gonzaga Y, Regalado-Artamendi I, Karlsson LK, Shapetska M, Hanakova M, El-Ashwah S, Borbényi Z, Çolak GM, Nordlander A, Dragonetti G, Maraglino AME, Rinaldi A, De Ramón-Sánchez C, Cornely OA, Group Ew. COVID-19 infection in adult patients with hematological malignancies: a European hematology association survey (EPICOVIDEHA). J Hematol Oncol. 2021;14(1):168.
Zhang H, Han H, He T, Labbe KE, Hernandez AV, Chen H, Velcheti V, Stebbing J, Wong KK. Clinical characteristics and outcomes of COVID-19-infected cancer patients: a systematic review and meta-analysis. J Natl Cancer Inst. 2021;113(4):371.
Liu H, Yang D, Chen X, Sun Z, Zou Y, Chen C, Sun S. The effect of anticancer treatment on cancer patients with COVID-19: a systematic review and meta-analysis. Cancer Med. 2021;10(3):1043.
Mina A, van Besien K, Platanias LC. Hematological manifestations of COVID-19. Leuk Lymphoma. 2020;61(12):2790.
Rostami M, Mansouritorghabeh H. D-dimer level in COVID-19 infection: a systematic review. Expert Rev Hematol. 2020;13(11):1265.
Thakkar A, Gonzalez-Lugo JD, Goradia N, Gali R, Shapiro LC, Pradhan K, Rahman S, Kim SY, Ko B, Sica RA, Kornblum N, Bachier-Rodriguez L, McCort M, Goel S, Perez-Soler R, Packer S, Sparano J, Gartrell B, Makower D, Goldstein YD, Wolgast L, Verma A, Halmos B. Seroconversion rates following COVID-19 vaccination among patients with cancer. Cancer Cell. 2021;39(8):1081.
du Plessis M, Fourie C, Riedemann J, de Villiers WJS, Engelbrecht AM. Cancer and Covid-19: collectively catastrophic. Cytokine Growth Factor Rev. 2022;63:78.
Rahimmanesh I, Shariati L, Dana N, Esmaeili Y, Vaseghi G, Haghjooy JS. Cancer occurrence as the upcoming complications of COVID-19. Front Mol Biosci. 2021;8: 813175.
Liu Y, Lu H, Wang W, Liu Q, Zhu C. Clinical risk factors for mortality in patients with cancer and COVID-19: a systematic review and meta-analysis of recent observational studies. Expert Rev Anticancer Ther. 2021;21(1):107.
Lin Z, Chen J, Han S. Impact of anti-cancer therapy on disease severity and mortality in cancer patients with COVID-19: a systematic review and meta-analysis. Expert Rev Anticancer Ther. 2021;21(9):1055.
Yekedüz E, Utkan G, Ürün Y. A systematic review and meta-analysis: the effect of active cancer treatment on severity of COVID-19. Eur J Cancer. 2020;141:92.
Wang B, Huang Y. Immunotherapy or other anti-cancer treatments and risk of exacerbation and mortality in cancer patients with COVID-19: a systematic review and meta-analysis. Oncoimmunology. 2020;9(1):1824646.
Wu Q, Luo S, Xie X. The impact of anti-tumor approaches on the outcomes of cancer patients with COVID-19: a meta-analysis based on 52 cohorts incorporating 9231 participants. BMC Cancer. 2022;22(1):241.
Park R, Lee SA, Kim SY, de Melo AC, Kasi A. Association of active oncologic treatment and risk of death in cancer patients with COVID-19: a systematic review and meta-analysis of patient data. Acta Oncol. 2021;60(1):13.
Yatim N, Boussier J, Tetu P, Smith N, Bruel T, Charbit B, Barnabei L, Corneau A, Da Meda L, Allayous C, Baroudjian B, Jebali M, Herms F, Grzelak L, Staropoli I, Calmettes V, Hadjadj J, Peyrony O, Cassius C, LeGoff J, Kramkimel N, Aractingi S, Fontes M, Blanc C, Rieux-Laucat F, Schwartz O, Terrier B, Duffy D, Lebbe C. Immune checkpoint inhibitors increase T cell immunity during SARS-CoV-2 infection. Sci Adv. 2021;7(34):eabg4081.
Peng Y, Mentzer AJ, Liu G, Yao X, Yin Z, Dong D, Dejnirattisai W, Rostron T, Supasa P, Liu C, Lopez-Camacho C, Slon-Campos J, Zhao Y, Stuart DI, Paesen GC, Grimes JM, Antson AA, Bayfield OW, Hawkins D, Ker DS, Wang B, Turtle L, Subramaniam K, Thomson P, Zhang P, Dold C, Ratcliff J, Simmonds P, de Silva T, Sopp P, Wellington D, Rajapaksa U, Chen YL, Salio M, Napolitani G, Paes W, Borrow P, Kessler BM, Fry JW, Schwabe NF, Semple MG, Baillie JK, Moore SC, Openshaw PJM, Ansari MA, Dunachie S, Barnes E, Frater J, Kerr G, Goulder P, Lockett T, Levin R, Zhang Y, Jing R, Ho LP, Oxford Immunology Network Covid-19 Response TcC, Investigators IC, Cornall RJ, Conlon CP, Klenerman P, Screaton GR, Mongkolsapaya J, McMichael A, Knight JC, Ogg G, Dong T. Broad and strong memory CD4(+) and CD8(+) T cells induced by SARS-CoV-2 in UK convalescent individuals following COVID-19. Nat Immunol. 2020;21(11):1336.
Moore JB, June CH. Cytokine release syndrome in severe COVID-19. Science. 2020;368(6490):473.
Karami H, Derakhshani A, Ghasemigol M, Fereidouni M, Miri-Moghaddam E, Baradaran B, Tabrizi NJ, Najafi S, Solimando AG, Marsh LM, Silvestris N, De Summa S, Paradiso AV, Racanelli V, Safarpour H. Weighted Gene Co-expression network analysis combined with machine learning validation to identify key modules and hub genes associated with SARS-CoV-2 infection. J Clin Med. 2021;10(16):3567.
Sodeifian F, Nikfarjam M, Kian N, Mohamed K, Rezaei N. The role of type I interferon in the treatment of COVID-19. J Med Virol. 2022;94(1):63.
Ioannou N, Hagner PR, Stokes M, Gandhi AK, Apollonio B, Fanous M, Papazoglou D, Sutton LA, Rosenquist R, Amini RM, Chiu H, Lopez-Girona A, Janardhanan P, Awan FT, Jones J, Kay NE, Shanafelt TD, Tallman MS, Stamatopoulos K, Patten PEM, Vardi A, Ramsay AG. Triggering interferon signaling in T cells with avadomide sensitizes CLL to anti-PD-L1/PD-1 immunotherapy. Blood. 2021;137(2):216.
Fountzilas E, Tsimberidou AM, Vo HH, Kurzrock R. Clinical trial design in the era of precision medicine. Genome Med. 2022;14(1):101.
Acknowledgements
We acknowledge Superior Medical Experts for drafting and editing assistance. The authors also acknowledge the software development team from Nested Knowledge, Stephen Mead, Jeffrey Johnson, and Darian Lehmann-Plantenberg for their input in designing Nested Knowledge.
Funding
This study was funded by Nested Knowledge, Inc.
Author information
Authors and Affiliations
Contributions
NH was involved in project management, data collection, data quality control, writing, and manuscript reviewing and editing; CV was responsible for project conceptualization, project management, and manuscript reviewing and editing; MM, JS, RG, YK, and MG collected the data and reviewed and edited the manuscript; JT took part in data collection, manuscript reviewing and editing, and risk of bias; AM wrote, reviewed, and edited the manuscript; JMP contributed to data quality control, meta-analysis, risk of bias (adjudication), writing, and manuscript reviewing and editing.; RT participated in data quality control and manuscript reviewing and editing; PO was involved in data quality control, manuscript reviewing and editing, and risk of bias; AG and RN were responsible for screening and manuscript reviewing and editing; PK, YP, and RR reviewed and edited the manuscript; KK participated in project management and manuscript reviewing and editing; TM took part in project conceptualization and manuscript reviewing and editing.
Corresponding author
Ethics declarations
Conflict of interest
JMP is employed by and holds equity in Superior Medical Experts and Nested Knowledge. AM is employed by Superior Medical Experts. NH is employed by and holds equity in Nested Knowledge. KK has ownership interest in Nested Knowledge, Inc. JT, RT, and PO are employed by Nested Knowledge.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hardy, N., Vegivinti, C.T.R., Mehta, M. et al. Mortality of COVID-19 in patients with hematological malignancies versus solid tumors: a systematic literature review and meta-analysis. Clin Exp Med 23, 1945–1959 (2023). https://doi.org/10.1007/s10238-023-01004-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10238-023-01004-5