Abstract
Purposes
Patients with hematologic malignancies (HM) are among the individuals with highest risk of COVID-19 complications. We report the impact of remdesivir in patients with hematologic malignancies (HM) during Omicron in Mexico City.
Methods
All patients with HM and COVID-19 during December 2021–March 2022 were included. Socio-demographic and clinical data were collected. The primary outcome was COVID-19 progression. Variables associated with progression were analyzed.
Results
115 patients were included. Median age was 50 years (IQR 35–63); 36% (N = 41) had at least one comorbidity. Fifty-two percent had non-Hodgkin lymphoma. Fifty patients (44%) had at least two doses of SARS-CoV-2 vaccine. COVID-19 was classified as mild (52.6%), moderate (9.7%), and severe/critical (28%). Twenty-eight patients (24%) received remdesivir. Nine patients received remdesivir at the ambulatory clinic (33%), the rest during hospital admission. Overall, 22(19%) patients progressed to severe/critical COVID-19; nine died due to COVID-19(8%). Hospital admission for non-COVID-19 causes was associated with higher odds of progression. Remdesivir did not reduce the risk of progression in hospitalized patients; none of the patients who received remdesivir in the ambulatory clinic progressed to severe COVID-19 or died.
Conclusions
Patients with HM and COVID-19 continue to present with high risk of complications. More prospective studies are needed to define the impact of antivirals in this high-risk group, including the best duration of treatment. Also, better vaccine coverage and access to treatment are mandatory.
Similar content being viewed by others
Introduction
Since the rollout of the vaccines, hospitalizations and mortality associated with the COVID-19 Pandemic have decreased overall. The Omicron variant of SARS-CoV-2 appeared in November 2021 in South Africa, and soon after, spread globally replacing the Delta strain. The Omicron variant has been characterized by a higher transmissibility, but lower virulence than other strains, with a lower rate of hospitalization and mortality in the general population and vaccinated individuals, compared to Delta variant [1,2,3]. Mexico’s fourth wave was characterized by a rapid increase in cases in the last week of December 2021 [4] up to March 2022. The National Genomic surveillance reported the presence of Omicron (B.1.1.529, BA.1, BA.1.1, BA.2) in late December 2021, with an escalating predominance to > 90% of sequences in Mexico City by early January 2022 [5].
Despite a high proportion of vaccinated individuals, immunosuppression and advanced age are high-risk conditions for worse outcomes [6,7,8]. Patients with COVID-19 and cancer have a higher risk of adverse outcomes, with increased mortality compared to the general population [8]. They have a poor humoral response to vaccines compared to non-immunosuppressed individuals and frequent breakthrough infections, which is particularly the case of patients with hematologic malignancies (HM) [9,10,11]. Moreover, in Mexico, many different vaccines have been approved besides mRNA vaccines and AZ1222, including other viral vector vaccines (Sputnik-V and Cansino) and inactivated vaccines (Sinovac) [12], all with different efficacy rates. The clinical outcomes of the infection with the Omicron variant in immunosuppressed patients have been poorly reported [7, 13,14,15,16], and much more focused on the protection conferred by the mRNA vaccines [17,18,19].
Access to antivirals for SARS-CoV-2 has been scarce in Mexico, even for patients with cancer. In January 2022, with the surge of the fourth wave caused by Omicron, remdesivir was made available for a subset of patients at our Institution. We report the clinical characteristics and outcomes of a cohort of patients with HM during the Omicron wave and the impact of remdesivir use in these high-risk patients.
Methods
Setting
Instituto Nacional de Cancerología (Incan) is a 133-bed tertiary care hospital located in Mexico City, that serves uninsured patients with cancer coming mostly from the central region of the country. During the Pandemic, INCan worked as a hybrid hospital and kept receiving patients for treatment and follow up of their cancer. However, an area of the hospital was reconverted for COVID-19 care, with a consultation for respiratory triage and COVID testing, and a ward for hospitalization and critical care of severe COVID-19 patients. During 2020 and 2021, there was no access to antivirals or monoclonal antibodies, and SARS-COV2 infected patients were only treated for severe disease to mitigate the inflammatory response. At the end of January 2022, remdesivir was available in the hospital for patients with active cancer and less than 7 days of symptoms.
Procedures
An algorithm was created to prioritize the highest risk patients for severe COVID-19, which included patients with active HM among others [20] (see Fig. 1, supplementary material). An ambulatory clinic was established to administer a three-day regimen of remdesivir for patients with mild COVID-19 and no criteria for hospitalization. If patients were hospitalized with mild COVID-19, due to other conditions (such as febrile neutropenia), or with severe COVID, they received remdesivir in the hospital. According to the protocol of our hospital, and based on the evidence reported [21], mild to moderate cases with no oxygen requirement received only three days of remdesivir. Patients with oxygen requirements received 5 days of treatment [22, 23]. Severity of COVID-19 was defined according to World Health Organization and National Institutes of health as mild (tested positive for SARS-CoV-2 with or without COVID-19 symptoms and absence of dyspnea or abnormal chest imaging), moderate (evidence of pneumonia on clinical assessment or chest imaging with saturation > 94%), severe (evidence of pneumonia on clinical assessment or chest imaging with saturation > 90%) and critical (acute respiratory distress syndrome, mechanical ventilation or shock) [21, 24].
Study participants
For study purposes, we included all patients with an HM diagnosed with COVID-19 from December 1st, 2021, to March 31st, 2022. The diagnosis was based on a positive SARS-CoV-2 PCR or rapid antigen test in symptomatic patients with fever or respiratory symptoms. Asymptomatic positive patients to PCR screening prior to chemotherapy were also included. Information was collected from the electronic files, including socio-demographic data, days of symptoms, type of neoplasm, COVID-19 severity, vaccine status, treatment received, progression of COVID-19 and death. For remdesivir use, we describe the number of days of remdesivir administered, the setting (ambulatory vs. hospitalized) and time from initiation of symptoms. We defined COVID-19 progression as the change of patient's clinical status from mild/moderate to any category with oxygen requirements [21].
Statistical analysis
We described data as simple proportions and median interquartile range (IQR) for qualitative and quantitative variables, respectively. The outcomes of interest were progression to a more severe clinical presentation, and death. We performed a univariate analysis of variables associated with progression and death and compared the risk of progression in patients who received remdesivir for 3 or 5 days. We used the Chi-square or Fisher exact test for qualitative variables, and Mann–Whitney test for quantitative variables, as appropriate. For analysis purpose, we excluded asymptomatic patients (detected through pre-chemotherapy screening) and critical patients (which were already progressed) from the univariate and multivariate analysis of outcomes. To compare progression proportions with or without the use of remdesivir, we excluded patients who received it after seven days of symptoms. To account for confounders, we performed a multivariate analysis using all variables with a p value < 0.2 in the univariate analysis, for both outcomes of progression and death.
Results
We included 115 patients. The characteristics of the cohort are presented in Table 1. Women represented 35% (N = 40) of the sample. Median age was 50 years (IQR 35–63); 35.7% (N = 41) had at least one comorbidity, mainly obesity, diabetes, and high blood pressure. Eleven patients (10%) were living with HIV, and the median CD4 count closest to COVID-19 was 294 cells/mm3. Nine patients (82%) were on antiretroviral (ARV) therapy with undetectable viral load. Two patients had recently been diagnosed with HIV and not on ARV. The main oncological diagnosis was non-Hodgkin lymphoma (N = 60, 52.2%), followed by acute lymphoblastic leukemia (N = 16, 14%), acute myeloid leukemia 12 (10.4%) and Hodgkin Lymphoma (N = 12, 10.4%). Ten patients had received a bone marrow transplant (8.7%). Almost 50% (N = 54) had received chemotherapy within the last month, and 30.4% (N = 35) had received rituximab (RTX) within the last six months. Only 16.5% (N = 19) were not on active treatment.
Regarding SARS-CoV-2 vaccination, 88 patients (77.2%) had been vaccinated with at least one dose; 44% (N = 50) had 2 doses and 20% (N = 23) had three doses. Of 83 patients who reported the type of vaccine, 32 (38.6%) received AZ1222, 22 (26.5%) BNT162b2 and 17 (20.5%) Sputnik-V. Twelve patients (14.5%) received other vaccines such as Cansino or Sinovac.
The median days from the onset of symptoms to COVID-19 diagnosis was 3 (IQR 2–6) days. COVID-19 was classified as mild in 52.6% of cases, moderate in 9.7%, and severe or critical in 28%. Eleven patients (9.7%) were asymptomatic at the time of diagnosis. These patients were diagnosed due to screening prior to chemotherapy. In total, 53 (46%) patients required hospitalization at some point of the disease; 30 of them were related to COVID-19. The other 23 patients were hospitalized due to other causes, such as febrile neutropenia (N = 15) or activity of the HM. Of the 53 patients who required hospitalization, 44 were hospitalized at COVID-19 diagnosis, and the rest (9 patients) were hospitalized days later, due to COVID-19 progression (Table 2).
Laboratory values at COVID-19 diagnosis were available for 43 patients. The median neutrophil count was 1.5 × 109/L, and the median lymphocyte count was 0.7 × 109/L. Patients who were hospitalized had significantly lower median neutrophil count (0.6 vs 2.450 × 109/L, p = 0.006) and median lymphocyte counts (0.3 vs 0.95 × 109/L, p < 0.001) at COVID-19 diagnosis, and differed in their hematological diagnosis (acute leukemias and non-Hodgkin lymphomas accounted for 84.5% of hospitalized patients vs. 77% of non-hospitalized patients, p = 0.009). Also, there were more patients with recently diagnosed, untreated hematological malignancies or with progression of their malignancy in the hospitalized group. There were no differences in the median neutrophil-to-lymphocyte ratio by hospital admission, COVID-19 progression, or death. Nine patients (7.8%) were diagnosed with COVID-19 more than 10 days after being admitted to the hospital (from 10 to 31 days after admission) which corresponds to 7.8% of the cohort. These were patients who had been admitted for workup of their hematologic diagnosis or febrile neutropenia; they were considered as nosocomial COVID-19.
Regarding treatment, 28 patients (24.4%) received remdesivir. Information on the timing of remdesivir is missing from one patient. For the 27 individuals left, remdesivir was administered during the first seven days of symptoms in 24 patients (88.9%). Twelve patients (44.4%) were treated in the first three days of symptoms. Two patients were treated in days 8 and 9. One patient who had prolonged COVID-19 received remdesivir during a flare, at day 47. Two patients were asymptomatic, 14 had mild COVID-19, 6 were moderate, and 6 were severe. None of the critical patients received remdesivir. Nineteen patients received three days of remdesivir; seven patients received five days of treatment. One patient received only two days of treatment (3.7%); remdesivir was stopped by the attending physician after receiving the Cycle threshold results for his initial PCR which were > 34. Nine patients with mild COVID-19 received remdesivir at the ambulatory clinic (33.3%). The rest were treated while being hospitalized. Of the 53 patients who were hospitalized, the median of hospital stay was 8 days (IQR 5-19) for patients who received remdesivir vs. 15 days (IQR 6-31) for those who did not receive the antiviral (p = 0.3). Among patients who were hospitalized for non-COVID reasons, median days of hospitalization were 11.5 (IQR 7-19) for those who received remdesivir, compared to 26 days (IQR 9-33) for those who did not (p = 0.2).
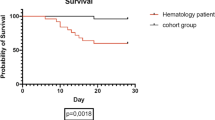
Twenty-two (19.1%) patients progressed to severe/critical COVID-19. None of the patients who received remdesivir in the ambulatory clinic progressed to severe COVID-19 or died. Overall, eleven patients died (9.7%), two due to acute leukemia, and nine died of COVID-19 (7.8%). The mortality rate in hospitalized patients was 16.9% (Table 2).
In the univariate analysis, patients who progressed were older than those who did not progress (56 years-old vs. 48 years, p = 0.018). Other variables associated with progression were active neoplasia, prior use of rituximab, being hospitalized at the diagnosis of COVID-19, and the initial severity of COVID-19 infection. Being vaccinated with one, two or three doses was not associated with less progression (Table 3). None of the patients in remission progressed (p = 0.016). Neutrophil count or lymphocyte count at COVID-19 diagnosis was not associated with the outcomes. Interestingly, patients who were hospitalized for non-COVID causes progressed more than patients not hospitalized (p = 0.025).
Regarding remdesivir recipients, patients who received three days of remdesivir progressed less than patients who received 5 days (16% vs 57%, p = 0.057). Sixteen percent of the patients who received remdesivir on the first seven days of symptoms progressed, compared to 100% of patients who received it after seven days (p = 0.012). None of the patients who received ambulatory remdesivir progressed, compared to 32% of those who received it during hospitalization (p = 0.036) (Table 4).
In the multivariate analysis, after adjusting for confounders, there was no association between the use of remdesivir and progression. However, there was still an association of progression with hospital admission for non-COVID-19 causes (Table 5).
When we analyzed death as an outcome, only age and hospitalization were associated with higher odds of dying in the univariate analysis, but this was not found in the multivariate analysis.
Discussion
We describe a cohort of individuals with HM and COVID-19 during the BA.1 and BA.2 Omicron wave of COVID-19 in Mexico. Most patients were diagnosed early, with a median onset of symptoms of three days, and more than half initially classified as mild (56%). Despite that Omicron has been reported to be milder, almost 20% of this cohort of cancer patients progressed to more severe forms of disease and 8% died due to COVID-19. The mortality rate among hospitalized patients was 16%. So far, few reports have been published on the outcomes of Omicron in immunosuppressed patients.
Publications have described cohorts of cancer with COVID-19 prior to Omicron. An Israeli study reported a mortality rate of 20% in hematologic patients, before the Delta wave [25]. At INCan, we reported a cohort of non-vaccinated patients with Cancer and COVID-19, with a mortality rate of 18% [26]. Regarding Omicron, Taenaka et al. reported an outbreak of 9 patients with HM in February 2022, with a mortality rate of 22% [13]. The OnCOVID European Study, a multisite European Registry of patients with cancer and COVID-19, compared the outcomes of Omicron to the “alpha-delta” variant phase and the pre-vaccination phase [14]. The case fatality rate at 28 days was 13% during Omicron, lower than the pre-vaccination phase (29%) and the alpha-delta phase (23.9%). However, after adjusting for vaccination, the mortality rate in unvaccinated patients during the Omicron phase was as high as the mortality reported during the pre-vaccination phase. The authors report an impact of vaccination in both alpha/delta and Omicron. However, most patients had solid tumors and there was only a small proportion of HM (only 63 patients during Omicron). Salmanton-García et al. recently reported the outcomes of 593 HM patients infected with Omicron from a multicenter Registry including mainly European Countries (EPICOVIDEHA) [15]. Their progression and mortality rates were like our findings (17% and 16% respectively). Older age, active malignancy and pre-existing pulmonary disease were associated with progression or death, as in our cohort. A higher lymphocyte count and the use of monoclonal antibodies were associated with a lower risk for mortality. They also reported a protective effect of 3 doses of the vaccine against progression to critical illness in hospitalized patients. Regarding vaccination, other reports have demonstrated protection of the vaccine in patients with HM. Piñana et al. reported the incidence of breakthrough infections in patients vaccinated with 2 doses of mainly mRNA vaccines from a prospective multicenter Spanish Registry of hematologic patients registered before Omicron [10]. They analyzed SARS-Cov2 antibodies titers and found lower levels in patients with breakthrough infections compared to patients without COVID-19. They also found more symptomatic disease, pneumonia, and hospitalization in individuals with titers less than 250 BAU/mL. In our cohort, 44% of patients were vaccinated with 2 doses, but we did not find an association of full vaccination status with better outcomes. This could be related to the fact that a higher proportion of our patients were vaccinated with non-mRNA vaccines, which have lower efficacy rates (only 26% received an mRNA vaccine). Also, a third of our patients were receiving rituximab, an anti-CD20 monoclonal antibody that has been associated with B cell depletion and poor vaccine response [27]. This B cell depletion can last up to 6 to 9 months after the end of the therapy, and many reports including hematologic and rheumatologic patients have shown reduced humoral response and less immunogenicity with the vaccines [28, 29]. Most of the studies report the efficacy using mRNA vaccines and the information with other vaccines is scarce. Rituximab has been reported to reduce antibody titers of inactivated vaccines (coronavac) as well [30].
Regarding SARS-CoV-2-targeted treatment options, few treatments have been approved for COVID-19. Recently, new antivirals have shown to reduce progression of COVID-19 [22, 31, 32]. Remdesivir administered for three days in the first 7 days of symptom onset in ambulatory patients showed an 87% reduction of the risk of hospitalization or death in patients with at least one risk factor for progression compared to placebo [22]. All patients from these trials were non-vaccinated individuals. Also, the proportion of immunosuppressed patients in these trials was low (less than 5% in all trials).
In our series, all patients had cancer and different degrees of immunosuppression; half of them were vaccinated with at least 2 doses of COVID-19 vaccines. Most patients who received remdesivir did so as a 3-day regimen for mild COVID-19, and early, following the Pinetree trial results [22]. Despite having a mild COVID-19, only 9 patients were treated on ambulatory basis, because they had other criteria for hospital admission at COVID-19 diagnosis. None of the 9 patients treated with ambulatory remdesivir progressed or died, which suggests a favorable impact of early treatment. A recent article published by Rajme and colleagues found a 84% reduction of hospitalization or death in patients with high-risk factors treated with early ambulatory remdesivir, from a tertiary care center in Mexico City [16]. Almost all patients were immunosuppressed, but only 12% had a hematologic disorder. In their study, authors only included patients who received ambulatory remdesivir. They did not include patients with mild COVID-19 who required hospital admission due to other causes. We included in our study mild COVID-19 cases admitted to the hospital, and we found that being hospitalized at diagnosis, or for non-COVID reasons, was associated with progression of COVID-19. In these patients there was no association of remdesivir use with better outcomes after adjusting for other variables. With these findings, it is difficult to say that remdesivir in mild COVID-19 had a positive impact on progression in hospitalized patients with non-COVID admission criteria.
One explanation for the lack of impact of remdesivir on progression in our cohort could be the duration of treatment in patients with prolonged shedding and poor capacity of neutralization [11, 19, 33, 34]. It is possible that immunosuppressed patients with mild COVID-19 could benefit from longer treatment with remdesivir, and further studies are needed to evaluate the best duration of treatment. Small reports have shown potential benefits of prolonged courses of remdesivir in these patients and an improved response with combination treatments of remdesivir and convalescent plasma [35, 36].
Our study has some limitations. It is a retrospective study from one center, and few patients had access to remdesivir (only 24% of our sample). A bigger sample of patients exposed to the antiviral will probably yield more valuable information. We did not measure viral load or Cycle thresholds routinely in our patients, to evaluate the viral dynamics with the use of remdesivir. This could help to understand the action of this antiviral in highly immunosuppressed patients such as the ones in this series and define the best duration of treatment in these patients. On the other hand, Incan is the most important oncologic referral center of the country and there is almost no literature published in middle income countries.
In summary, we report a sample of hematologic patients with considerable morbi-mortality during the Omicron wave, early in 2022 in Mexico City. Only a quarter had access to an antiviral. Patients who received ambulatory remdesivir for three days did not progress to more severe COVID-19. However, in patients who were admitted to the hospital at COVID-19 diagnosis, remdesivir use was not associated with improved outcomes. These patients were more immunosuppressed than ambulatory patients, which is associated with poor outcomes. More prospective studies with larger samples are needed, and prolonged treatments should be considered in prospective trials. Finally, only two thirds of the cohort had a complete vaccination scheme, and there was no significant impact of the vaccine status in the outcomes. Although efficacy rates are lower, it is imperative to improve vaccine coverage in this group of patients. Also, better access to antivirals in these high-risk patients is mandatory.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Nyberg T, Ferguson NM, Nash SG, Webster HH, Flaxman S, Andrews N, et al. Comparative analysis of the risks of hospitalisation and death associated with SARS-CoV-2 omicron (B.1.1.529) and delta (B.1.617.2) variants in England: a cohort study. Lancet Lond Engl. 2022;399(10332):1303–12.
Shuai H, Chan JFW, Hu B, Chai Y, Yuen TTT, Yin F, et al. Attenuated replication and pathogenicity of SARS-CoV-2 B11529 Omicron. Nature. 2022;603(7902):693–9.
Zhao H, Lu L, Peng Z, Chen LL, Meng X, Zhang C, et al. SARS-CoV-2 Omicron variant shows less efficient replication and fusion activity when compared with delta variant in TMPRSS2-expressed cells. Emerg Microbes Infect. 2022;11(1):277–83.
John Hopkins University. Coronavirus resource center [Internet]. [cited 2022 Aug 31]. Available from: https://coronavirus.jhu.edu/region/mexico
CoViGen-Mex. Programa de Vigilancia Genómica del SARS-CoV-2 realizado por el CoViGen-Mex [Internet]. 2022. Available from: http://mexcov2.ibt.unam.mx:8080/COVID-TRACKER/open/reports/26%20de%20Enero%20del%202022.pdf
Kuderer NM, Choueiri TK, Shah DP, Shyr Y, Rubinstein SM, Rivera DR, et al. Clinical impact of COVID-19 on patients with cancer (CCC19): a cohort study. The Lancet. 2020;395(10241):1907–18.
Lee M, Quinn R, Pradhan K, Fedorov K, Levitz D, Fromowitz A, et al. Impact of COVID-19 on case fatality rate of patients with cancer during the Omicron wave. Cancer Cell. 2022;40(4):343–5.
Han S, Zhuang Q, Chiang J, Tan SH, Chua GWY, Xie C, et al. Impact of cancer diagnoses on the outcomes of patients with COVID-19: a systematic review and meta-analysis. BMJ Open. 2022;12(2): e044661.
Schmidt AL, Labaki C, Hsu CY, Bakouny Z, Balanchivadze N, Berg SA, et al. COVID-19 vaccination and breakthrough infections in patients with cancer. Ann Oncol Off J Eur Soc Med Oncol. 2022;33(3):340–6.
Piñana JL, López-Corral L, Martino R, Vazquez L, Pérez A, Martin-Martin G, et al. SARS-CoV-2 vaccine response and rate of breakthrough infection in patients with hematological disorders. J Hematol OncolJ Hematol Oncol. 2022;15(1):54.
Zeng C, Evans JP, Reisinger S, Woyach J, Liscynesky C, Boghdadly ZE, et al. Impaired neutralizing antibody response to COVID-19 mRNA vaccines in cancer patients. MedRxiv Prepr Serv Health Sci. 2021;11(1):16.
Secretaria de Salud. Información de la Vacuna [Internet]. [cited 2022 Aug 31]. Available from: https://vacunacovid.gob.mx/wordpress/informacion-de-la-vacuna/
Taenaka R, Obara T, Kohno K, Aoki K, Ogawa R. Infections with the SARS-CoV-2 Omicron variant show a similar outcome as infections with the previous variants in patients with hematologic malignancies. Ann Hematol. 2022;101(8):1877–8.
Pinato DJ, Aguilar-Company J, Ferrante D, Hanbury G, Bower M, Salazar R, et al. Outcomes of the SARS-CoV-2 omicron (B.1.1.529) variant outbreak among vaccinated and unvaccinated patients with cancer in Europe: results from the retrospective, multicentre on Covid registry study. Lancet Oncol. 2022;23(7):865–75.
Blennow O, Salmanton-García J, Nowak P, Itri F, Van Doesum J, López-García A, et al. Outcome of infection with omicron SARS-CoV-2 variant in patients with hematological malignancies: an EPICOVIDEHA survey report. Am J Hematol. 2022;97(8):E312–7.
Rajme-López S, Martinez-Guerra BA, Zalapa-Soto J, Román-Montes CM, Tamez-Torres KM, González-Lara MF, et al. Early outpatient treatment with remdesivir in patients at high risk for severe COVID-19: a prospective cohort study. Open Forum Infect Dis. 2022;9(10):ofac502.
Mair MJ, Mitterer M, Gattinger P, Berger JM, Trutschnig W, Bathke AC, et al. Enhanced SARS-CoV-2 breakthrough infections in patients with hematologic and solid cancers due to Omicron. Cancer Cell. 2022;40(5):444–6.
Zeng C, Evans JP, Chakravarthy K, Qu P, Reisinger S, Song NJ, et al. COVID-19 mRNA booster vaccines elicit strong protection against SARS-CoV-2 Omicron variant in patients with cancer. Cancer Cell. 2022;40(2):117–9.
Fendler A, Shepherd STC, Au L, Wu M, Harvey R, Schmitt AM, et al. Omicron neutralising antibodies after third COVID-19 vaccine dose in patients with cancer. Lancet Lond Engl. 2022;399(10328):905–7.
National institutes of health. The COVID-19 treatment guidelines panel’s interim statement on patient prioritization for outpatient anti-SARS-CoV-2 therapies or preventive strategies when there are logistical or supply constraints [Internet]. [cited 2022 Aug 31]. Available from: https://www.covid19treatmentguidelines.nih.gov/
National institutes of health. Coronavirus disease 2019 (COVID-19) treatment guidelines [Internet]. [cited 2022 Aug 31]. Available from: https://www.covid19treatmentguidelines.nih.gov/
Gottlieb RL, Vaca CE, Paredes R, Mera J, Webb BJ, Perez G, et al. Early remdesivir to prevent progression to severe COVID-19 in outpatients. N Engl J Med. 2022;386(4):305–15.
Goldman JD, Lye DCB, Hui DS, Marks KM, Bruno R, Montejano R, et al. Remdesivir for 5 or 10 days in patients with severe COVID-19. N Engl J Med. 2020;383(19):1827–37.
World Health Organization. COVID-19 clinical management: living guidance. 2021 [cited 2022 Aug 31]. Available from: https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-2. Accessed 25 Jan 2021.
Levy I, Lavi A, Zimran E, Grisariu S, Aumann S, Itchaki G, et al. COVID-19 among patients with hematological malignancies: a national Israeli retrospective analysis with special emphasis on treatment and outcome. Leuk Lymphoma. 2021;62(14):3384–93.
De-la-Rosa-Martinez D, Aranda-Audelo M, Martin-Onraet A, Islas-Muñoz B, Perez-Jimenez C, Alatorre-Fernandez P, et al. Clinical characteristics and outcomes in a cohort of oncologic patients with COVID-19 during the first year of the pandemic in Mexico. Cancer Med. 2022;11(8):1827–36.
Furlan A, Forner G, Cipriani L, Vian E, Rigoli R, Gherlinzoni F, et al. COVID-19 in B cell-depleted patients after rituximab: a diagnostic and therapeutic challenge. Front Immunol. 2021;12: 763412.
Bacova B, Kohutova Z, Zubata I, Gaherova L, Kucera P, Heizer T, et al. Cellular and humoral immune response to SARS-CoV-2 mRNA vaccines in patients treated with either Ibrutinib or Rituximab. Clin Exp Med. 2022. https://doi.org/10.1007/s10238-022-00809-0.
Furer V, Eviatar T, Zisman D, Peleg H, Paran D, Levartovsky D, et al. Immunogenicity and safety of the BNT162b2 mRNA COVID-19 vaccine in adult patients with autoimmune inflammatory rheumatic diseases and in the general population: a multicentre study. Ann Rheum Dis. 2021;80(10):1330–8.
Seyahi E, Bakhdiyarli G, Oztas M, Kuskucu MA, Tok Y, Sut N, et al. Antibody response to inactivated COVID-19 vaccine (CoronaVac) in immune-mediated diseases: a controlled study among hospital workers and elderly. Rheumatol Int. 2021;41(8):1429–40.
Jayk Bernal A, Gomes da Silva MM, Musungaie DB, Kovalchuk E, Gonzalez A, Delos Reyes V, et al. Molnupiravir for oral treatment of COVID-19 in nonhospitalized patients. N Engl J Med 2022;386(6):509–20 https://doi.org/10.1056/NEJMoa2116044.
Hammond J, Leister-Tebbe H, Gardner A, Abreu P, Bao W, Wisemandle W, et al. Oral nirmatrelvir for high-risk, nonhospitalized adults with COVID-19. N Engl J Med. 2022;386(15):1397–408.
Altamirano-Molina M, Pacheco-Modesto I, Amado-Tineo J. Prolonged viral shedding of SARS-CoV-2 in patients with acute leukemia. Hematol Transfus Cell Ther. 2022;44(2):299–300.
Goubet AG, Dubuisson A, Geraud A, Danlos FX, Terrisse S, Silva CAC, et al. Prolonged SARS-CoV-2 RNA virus shedding and lymphopenia are hallmarks of COVID-19 in cancer patients with poor prognosis. Cell Death Differ. 2021;28(12):3297–315.
Weinbergerová B, Demel I, Víšek B, Válka J, Čerňan M, Jindra P, et al. Successful early use of anti-SARS-CoV-2 monoclonal neutralizing antibodies in SARS-CoV-2 infected hematological patients—a Czech multicenter experience. Hematol Oncol. 2022;40(2):280–6.
Furlan A, Forner G, Cipriani L, Vian E, Rigoli R, Gherlinzoni F, et al. Dramatic response to convalescent hyperimmune plasma in association with an extended course of remdesivir in 4 B cell-depleted non-hodgkin lymphoma patients with SARS-Cov-2 pneumonia after rituximab therapy. Clin Lymphoma Myeloma Leuk. 2021;21(9):e731–5.
Acknowledgements
To all the patients and staff who have had to work hard during COVID-19 times.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
AMO, DVC and CBF designed the study. CBF collected the data. AMO, CBF, DVC, CPJ and PAF analyzed and interpreted the data and integrated the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Consent to participate
Due to the retrospective and observational nature of the study, the INCan’s “Comité de Ética en Investigación” waived the written informed consent.
Ethics approval
The study was performed in line with the principles of the Declaration of Helsinki and approved by the Institutional Review Committee “Comité de Ética en Investigación” of the INCan, #INCAN/CI0234/2022.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Martin-Onraët, A., Barrientos-Flores, C., Vilar-Compte, D. et al. Use of remdesivir for COVID-19 in patients with hematologic cancer. Clin Exp Med 23, 2231–2238 (2023). https://doi.org/10.1007/s10238-022-00964-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10238-022-00964-4