Abstract
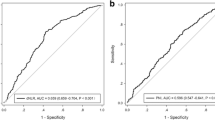
The systemic immune-inflammation index (SII), derived from neutrophil, platelet, and lymphocyte counts, has been associated with prognosis of patients with cancer. We performed a meta-analysis to evaluate the association between pretreatment SII and survival of patients with hepatocellular carcinoma (HCC) after transarterial chemoembolization (TACE). Cohort studies were identified by search of PubMed, Embase, Web of Science, CNKI, and Wanfang databases. Pooling the results was achieved with a random-effect model that incorporates potential heterogeneity between studies. Nine studies including 3557 patients with HCC contributed to the meta-analysis. Compared to patients with a lower SII, HCC patients with a higher pretreatment SII had poor overall survival (OS, hazard ratio [HR] 1.66, 95% confidence interval [CI] 1.25–2.21, p < 0.001; I2 = 80%) and poor progression-free survival (PFS, HR 1.28, 95% CI 1.05–1.56, p = 0.01; I2 = 0%) after TACE treatment. Further subgroup analyses confirmed a significant association between a high pretreatment SII and poor OS after TACE, which was not significantly affected by study country, sample size, age of the patients, cutoff values for SII, and adjustment of Child–Pugh score or alpha fetoprotein (p for subgroup effect all < 0.05). However, a higher SII was associated with poor OS in studies with follow-up duration ≤ 24 months (HR 1.94, 95% CI 1.39–2.72, p < 0.001), but the association was not statistically significant in studies with follow-up duration > 24 months (HR 1.27, 95% CI: 0.96–1.68, p = 0.09). A higher pretreatment SII was correlated with poor survival of HCC patients after TACE. A preliminary measurement of SII may be valuable for the prediction of the prognosis in HCC patients after TACE.



Similar content being viewed by others
Data availability
The data used to support the findings of this study are included within the article. The primary data used to support the findings of this study are available from the corresponding author upon request.
References
Xia C, Dong X, Li H, et al. Cancer statistics in China and United States, 2022: profiles, trends, and determinants. Chin Med J (Engl). 2022;135:584–90.
Siegel RL, Miller KD, Fuchs HE, et al. Cancer statistics, 2022. CA Cancer J Clin. 2022;72:7–33.
Mak LY, Cruz-Ramon V, Chinchilla-Lopez P, et al. Global Epidemiology, Prevention, and Management of Hepatocellular Carcinoma. Am Soc Clin Oncol Educ Book. 2018;38:262–79.
Chawla A, Ferrone C. Hepatocellular carcinoma surgical therapy: perspectives on the current limits to resection. Chin Clin Oncol. 2018;7:48.
Forner A, Reig M, Bruix J. Hepatocellular carcinoma. Lancet. 2018;391:1301–14.
Rizzo A, Nannini M, Novelli M, et al. Dose reduction and discontinuation of standard-dose regorafenib associated with adverse drug events in cancer patients: a systematic review and meta-analysis. Ther Adv Med Oncol. 2020;12:1758835920936932.
Rizzo A, Ricci AD, Gadaleta-Caldarola G, et al. First-line immune checkpoint inhibitor-based combinations in unresectable hepatocellular carcinoma: current management and future challenges. Expert Rev Gastroenterol Hepatol. 2021;15:1245–51.
De Lorenzo S, Tovoli F, Barbera MA, Garuti F, Palloni A, Frega G, Garajovà I, Rizzo A, Trevisani F, Brandi G. Metronomic capecitabine vs. best supportive care in child-pugh B hepatocellular carcinoma: a proof of concept. Scientific Reports. 2018. https://doi.org/10.1038/s41598-018-28337-6.
Raoul JL, Forner A, Bolondi L, et al. Updated use of TACE for hepatocellular carcinoma treatment: how and when to use it based on clinical evidence. Cancer Treat Rev. 2019;72:28–36.
Reig M, Forner A, Rimola J, et al. BCLC strategy for prognosis prediction and treatment recommendation: The 2022 update. J Hepatol. 2022;76:681–93.
Xie DY, Ren ZG, Zhou J, et al. 2019 Chinese clinical guidelines for the management of hepatocellular carcinoma: updates and insights. Hepatobiliary Surg Nutr. 2020;9:452–63.
Llovet JM, De Baere T, Kulik L, et al. Locoregional therapies in the era of molecular and immune treatments for hepatocellular carcinoma. Nat Rev Gastroen Hepatol. 2021;18:293–313.
Chang Young, Jeong Soung Won, Jang Jae Young, Kim Yong Jae. Recent updates of transarterial chemoembolilzation in hepatocellular carcinoma. Int J Mol Sci. 2020;21(21):8165. https://doi.org/10.3390/ijms21218165.
Sieghart W, Hucke F, Peck-Radosavljevic M. Transarterial chemoembolization: modalities, indication, and patient selection. J Hepatol. 2015;62:1187–95.
Bozzato Alessandro Marco, Martingano Paola, Mucelli Roberta Antea Pozzi, Cavallaro Marco Francesco Maria, Cesarotto Matteo, Marcello Cristina, Tiribelli Claudio, Pascut Devis, Pizzolato Riccardo, Mucelli Fabio Pozzi, Giuffrè Mauro, Crocè Lory Saveria, Cova Maria Assunta. MicroRNAs related to tace treatment response: a review of the literature from a radiological point of view. Diagnostics. 2022;12(2):374. https://doi.org/10.3390/diagnostics12020374.
Diakos CI, Charles KA, McMillan DC, et al. Cancer-related inflammation and treatment effectiveness. Lancet Oncol. 2014;15:e493-503.
Oura Kyoko, Morishita Asahiro, Tani Joji, Masaki Tsutomu. Tumor immune microenvironment and immunosuppressive therapy in hepatocellular carcinoma: a review. Int J Mol Sci. 2021;22(11):5801. https://doi.org/10.3390/ijms22115801.
Yang R, Chang Q, Meng X, et al. Prognostic value of Systemic immune-inflammation index in cancer: A meta-analysis. J Cancer. 2018;9:3295–302.
Marques P, de Vries F, Dekkers OM, et al. Serum Inflammation-based Scores in Endocrine Tumors. J Clin Endocrinol Metab. 2021;106:e3796–819.
Hu B, Yang XR, Xu Y, et al. Systemic immune-inflammation index predicts prognosis of patients after curative resection for hepatocellular carcinoma. Clin Cancer Res. 2014;20:6212–22.
Yang Z, Zhang J, Lu Y, et al. Aspartate aminotransferase-lymphocyte ratio index and systemic immune-inflammation index predict overall survival in HBV-related hepatocellular carcinoma patients after transcatheter arterial chemoembolization. Oncotarget. 2015;6:43090–8.
Cho EJ, Yu SJ, Cho H, et al. Prognostic values of inflammation and immune-based scores in patients with hepatocellular carcinoma who undergo transarterial chemoembolization. Hepatology. 2016;64:661A.
Gu J, Zhang X, Cui R, et al. Prognostic predictors for patients with hepatocellular carcinoma receiving adjuvant transcatheter arterial chemoembolization. Eur J Gastroenterol Hepatol. 2019;31:836–44.
Zhao LY, Yang DD, Ma XK, et al. The Prognostic Value of aspartate aminotransferase to lymphocyte ratio and systemic immune-inflammation index for Overall Survival of Hepatocellular Carcinoma Patients Treated with palliative Treatments. J Cancer. 2019;10:2299–311.
Muller L, Hahn F, Mahringer-Kunz A, et al. Immunonutritive Scoring for Patients with Hepatocellular Carcinoma Undergoing Transarterial Chemoembolization: Evaluation of the CALLY Index. Cancers (Basel) 2021;13.
Yu X, Cheng SH, Cao L, et al. Analysis of the correlation between the preoperative systemic immune inflammatory index and the prognosis in liver cancer patients receiving transarterial chemoembolization. J Intervent Radiol. 2021;30:461–5.
Liu Y, Shi M, Chen S, et al. Intermediate stage hepatocellular carcinoma: Comparison of the value of inflammation-based scores in predicting progression-free survival of patients receiving transarterial chemoembolization. J Cancer Res Ther. 2021;17:740–8.
Lu LH, Wei W, Li SH, et al. The lymphocyte-C-reactive protein ratio as the optimal inflammation-based score in patients with hepatocellular carcinoma underwent TACE. Aging (Albany NY). 2021;13:5358–68.
Young S, Cam I, Gencturk M, et al. Inflammatory scores: comparison and utility in hcc patients undergoing transarterial chemoembolization in a north american cohort. J Hepatocell Carcinoma. 2021;8:1513–24.
Page MJ, Moher D, Bossuyt PM, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372: n160.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372: n71.
Higgins J, Thomas J, Chandler J, et al. Cochrane Handbook for Systematic Reviews of Interventions version 6.2. The Cochrane Collaboration 2021;www.training.cochrane.org/handbook.
Wells GA, Shea B, O'Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2010;http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58.
Patsopoulos NA, Evangelou E, Ioannidis JP. Sensitivity of between-study heterogeneity in meta-analysis: proposed metrics and empirical evaluation. Int J Epidemiol. 2008;37:1148–57.
Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34.
Zhang Y, Chen B, Wang L, et al. Systemic immune-inflammation index is a promising noninvasive marker to predict survival of lung cancer: A meta-analysis. Medicine (Baltimore). 2019;98: e13788.
Zhang Y, Sun Y, Zhang Q. Prognostic value of the systemic immune-inflammation index in patients with breast cancer: a meta-analysis. Cancer Cell Int. 2020;20:224.
Qiu Y, Zhang Z, Chen Y. Prognostic value of pretreatment systemic immune-inflammation index in gastric cancer: a meta-analysis. Front Oncol. 2021;11: 537140.
Dong M, Shi Y, Yang J, et al. Prognostic and clinicopathological significance of systemic immune-inflammation index in colorectal cancer: a meta-analysis. Ther Adv Med Oncol. 2020;12:1758835920937425.
Li Mao, Li Zhenlu, Wang Zihe, Yue Chao, Weiming Hu, Huimin Lu. Prognostic value of systemic immune-inflammation index in patients with pancreatic cancer: a meta-analysis. Clin Experi Med. 2022. https://doi.org/10.1007/s10238-021-00785-x.
Wang B, Huang Y, Lin T. Prognostic impact of elevated pre-treatment systemic immune-inflammation index (SII) in hepatocellular carcinoma: a meta-analysis. Medicine (Baltimore). 2020;99: e18571.
Elinav E, Nowarski R, Thaiss CA, et al. Inflammation-induced cancer: crosstalk between tumours, immune cells and microorganisms. Nat Rev Cancer. 2013;13:759–71.
Rahat MA, Coffelt SB, Granot Z, et al. Macrophages and neutrophils: regulation of the inflammatory microenvironment in autoimmunity and cancer. Mediators Inflamm. 2016;2016:5894347.
Coffelt SB, Wellenstein MD, de Visser KE. Neutrophils in cancer: neutral no more. Nat Rev Cancer. 2016;16:431–46.
Faria AVS, Andrade SS, Peppelenbosch MP, et al. Platelets in aging and cancer-”double-edged sword”. Cancer Metastasis Rev. 2020;39:1205–21.
Catani MV, Savini I, Tullio V, et al. The “Janus Face” of platelets in cancer. Int J Mol Sci. 2020;21(3):788.
Schreiber RD, Old LJ, Smyth MJ. Cancer immunoediting: integrating immunity’s roles in cancer suppression and promotion. Science. 2011;331:1565–70.
St Paul M, Ohashi PS. The Roles of CD8(+) T Cell Subsets in Antitumor Immunity. Trends Cell Biol. 2020;30:695–704.
Wu Y, Tu C, Shao C. The value of preoperative systemic immune-inflammation index in predicting vascular invasion of hepatocellular carcinoma: a meta-analysis. Braz J Med Biol Res. 2021;54: e10273.
Shimada S, Kamiyama T, Orimo T, et al. Long-term prognostic factors of patients with hepatocellular carcinoma who survive over 10 years after hepatectomy. J Surg Oncol. 2020;121:1209–17.
Acknowledgements
We would like to thank the researchers and study participants for their contributions.
Funding
None.
Author information
Authors and Affiliations
Contributions
DL and XZ conceived the study. DL and XP performed literature search, data extraction, and quality evaluation. DL, XZ, KW, and DS performed statistical analyses and interpreted the data. DL and XZ drafted the manuscript. All authors revised the manuscript and approved the submission.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that there are no conflicts of interest regarding the publication of this paper.
Consent for publication
This manuscript does not contain any individual person’s data in any form [including any individual details, images, or videos). So the “Consent of for publications” is not appropriate for our manuscript.
Ethics approval
This manuscript does not report studies involving human participants, human data, or human tissue. So the “ethics approval and consent to participate” is not appropriate for our manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, D., Zhao, X., Pi, X. et al. Systemic immune-inflammation index and the survival of hepatocellular carcinoma patients after transarterial chemoembolization: a meta-analysis. Clin Exp Med 23, 2105–2114 (2023). https://doi.org/10.1007/s10238-022-00889-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10238-022-00889-y