Abstract
It is suggested that gastric mucins, and in particular some specific glycan structures that can act as carbohydrate receptors, are involved in the interactions with Helicobacter pylori adhesins. The main aim of our study was to evaluate glycosylation pattern of glycoproteins of gastric juice before and at the end of eradication therapy. Gastric juices were taken from 13 clinical patients and subjected to analysis. Pooled fractions of the void volume obtained after gel filtration were subjected to ELISA tests. To assess the relative amounts of carbohydrate structures, lectins and monoclonal antibodies were used. Changes in the level of MUC 1 and MUC 5AC mucins and of carbohydrate structures, which are suggested to be receptors for Helicobacter pylori adhesins, were observed by the end of the eradication treatment. Our results support the idea about the involvement of MUC 5AC and MUC 1 with some specific sugar structures in the mechanism of Helicobacter pylori infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
It is believed that gastric mucus gel layer forms an effective protective barrier against various pathogens, such as Helicobacter pylori, the major etiological agent of chronic gastritis, peptic ulcers, and gastric cancers [1–3]. The main components of mucus are the heavily O-glycosylated proteins known as mucins. Three of them are present in human stomach. MUC 5AC and MUC 6 mucins are all secreted into gastric juice; the former being expressed by the surface epithelium and the latter by the deeper antrum gland epithelium [4]. In addition, the epithelial membrane-associated MUC 1 mucin is also present in the stomach [5]. The glycans in mucins are mainly O-linked with blood group antigens often present terminally. Mucin-type oligosaccharides are structurally very diverse; the glycans in the same molecule can exhibit a high degree of subtle variations in their structure depending on dynamic physiological and pathological biochemical conditions that exist in the body at the time when the structures are formed [6]. The glycosyltransferases expressed by the individual determine glycan profiles of mucins in that individual [7].
Helicobacter pylori can colonize gastric epithelium by interactions with carbohydrates receptors [8]. Lewis b structure is one of the known receptors for bacterial adhesins (BabA–the blood group antigen–binding adhesin), and it is considered that MUC 5AC mucin is the main carrier of this structure [8, 9]. Some other glycoform structures (e. g. H type 1 structure, sialyl Lewis x) are also suggested to be implicated in binding with H. pylori adhesins [10–12]. It has been recently proposed that apart from MUC 5AC mucin, also MUC 1 can be carrier of receptors for bacterial adhesins and can be involved in development of infection [7, 13, 14]. There are suggestions that changes in glycoforms can affect the protective functions of gastric mucins and H. pylori colonization. It is postulated that alterations that occur during H. pylori infection are completely reversed after eradication [14].
The main aim of our study was to check whether there are changes in the pattern of glycosylation of the mucins of gastric juice before and after eradication of H. pylori. We assumed that carbohydrates present in gastric juice originate from gastric mucosa. Among them, there are secreted MUC 5AC mucin and soluble form of membrane-bound MUC 1. We suppose a parallel relationship between MUC 1 cell membrane expression and its shedding to gastric juice. To test the changes in glycosylation, we used ELISA method with monoclonal antibodies against gastric mucins and some glycan epitopes and biotinylated lectins with well-known sugar specificity.
Materials and methods
Patients and specimens
Thirteen Helicobacter pylori–infected patients with duodenal ulcers (9 men, 4 women; age range 24–60, mean age 44), hospitalized in the Department of Medicine and Gastroenterology of Regional Hospital of Białystok, Poland, were included in the study. Each patient was treated for 2 weeks with oral administration of omeprazole (2 × 20 mg per day), amoxiciline (2 × 1,000 mg), and tynidazole (2 × 500 mg). All subjects were on standard hospital diet served for the peptic ulcer patients. The tested gastric juices were taken before and on days 11–13 of the treatment. They were collected by aspiration for 15 min with a gastric catheter inserted through the nares. The procedure was performed in the morning hours after overnight fasting. At the first gastric test, no drugs were allowed for at least 14 days, at the second gastric test the last doses of the drugs (omeprazole, amoxicillin, and tinidazole) were taken in the evening preceding the day of the examination.
The presence of the bacterium was examined histologically and by urease test with gastric cells scraped under endoscopic examination. It was done before and at the end of the treatment. The eradication therapy was successful in all the patients at the second endoscopy assessment.
Enzyme-linked immunosorbent assay
The juice was initially treated as described before [15]. High molecular mass material obtained in the void volume after gel filtration was subjected to further analysis. To assess relative amounts of carbohydrate structures in examined material, ELISA tests with monoclonal antibodies and biotinylated lectins were performed. Specifications of antibodies employed in this study are listed in Table 1. For carbohydrate specificity of lectins, see Table 2. Samples of gastric juices were diluted to the identical protein concentration 5 μg/mL, and aliquots (50 μL) were coated onto microtiter plates (NUNC F96; Maxisorp, Roskilde, Denmark) at room temperature overnight. The protein content was determined using bicinchoninic acid [16]. The plates were washed 3 times (100 μL) with PBS, pH 7.4, 0.05% Tween (PBS-T; washing buffer) between all ensuing steps. Unbound sites were blocked with 100 μL of 1% blocking reagent for ELISA (Roche Diagnostics, Mannheim, Germany) for 1 h. The microtiter plates were incubated with 100 μL of biotinylated lectins (1 h) diluted to 0.5 μg/mL in PBS-T, 1% bovine serum albumin, BSA (Sigma, St Luis, MO, USA). Some lectin solutions were supplemented with metal cations: DSA, UEA, SNA, LTA, PNA, and GNA with 0.1 mmol/L CaCl2; MAA and VVA with 0.1 mmol/L CaCl2 and 0.01 mmol/L MnCl2. Plates were then incubated with 100 μL of horseradish peroxidase avidin D (Vector, Burlingame, CA, USA) (1 : 2 500) in PBS-T, 1% BSA for 1 h. Next, plates were washed 4 times in PBS, and the colored reaction was developed by incubating with 2,2′-azino-bis(3-ethylbenzthiazoline-6-sulfonic acid) (ABTS)–liquid substrate for horseradish peroxidase (Sigma, St Luis, MO, USA). Absorbance at 405 nm was measured after 30–45 min. For analysis with monoclonal antibodies (diluted in washing buffer, 1% BSA), the plates were coated with 100 μL of antibody for 1 h. Next, they were incubated with secondary antibody, horseradish peroxidase–conjugated anti-mouse IgG (for anti-MUC 1, MUC 5AC, Lewis b, and H type 1 structures) or anti-mouse IgM (for anti-sialyl Lewis x structure). The colored reaction was developed as mentioned earlier. As controls wells with no gastric juices were used.
Statistical analyses
The relative amounts of examined structures (based on absorbance at 405 nm obtained from ELISA tests) were subjected to statistical analysis (by STATISTICA 7.1 StatSoft program). All the data revealed normal distribution, and two-sided t-test was used. Statistical significance was assumed at P < 0.05. Pearson’s correlations of two variables (the relative amounts of MUC 1 and MUC 5AC mucins before and at the end of the treatment versus the relative amounts of examined carbohydrate structures before and at the end of the therapy) were calculated.
The study was approved by the Institutional Ethical Committee and conducted according to the principles of the Declaration of Helsinki. Informed consent was obtained from all the patients.
Results
Juices from 13 patients were divided into two groups: before eradication and at the end of eradication therapy (11–13 day of the treatment). High molecular mass material of void volume obtained after gel filtration of gastric juices was taken for glycan analysis.
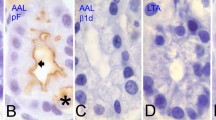
Glycans of all gastric juices examined revealed reactivity with monoclonal antibodies (Fig. 1) and lectins (Fig. 2) employed in this study. The analysis of the interactions of gastric juices with specific anti-MUC 1 and MUC 5AC monoclonal antibodies revealed higher levels of both mucins in juices at the end of eradication treatment. In case of MUC 1, the difference was statistically significant (P = 0.000066) (Fig. 3).
The relative amounts of specific carbohydrate structures Lewis b, sialyl Lewis x, and H type 1 recognized by monoclonal antibodies were found to be higher at the end of eradication therapy. For sialyl Lewis x and H type 1 structures, the differences were statistically significant (P = 0,00208 and 0.00209 for sialyl Lewis x and H type 1, respectively) (Fig. 3).
Fucosylation profile was examined by LTA, UEA, and AAA lectins. The lowest amount was observed for Fuc α 1-3 bond. The relative amounts of all fucosylated structures were higher at the end of eradication treatment. The differences were statistically significant for AAA and UEA lectins (P = 0.000124 and 0.03475, respectively) (Fig. 4).
SNA and MAA are lectins specific for sialic acid. The analysis of interactions of these lectins with glycoproteins of juices showed a little higher amount of SA α 2–3 than SA α 2–6 linkage. In both cases, higher level of these specific structures was observed at the end of the treatment with statistically significant difference for SNA (P = 0.003475) (Fig. 4).
PNA and VVA lectins recognize T and Tn antigens, respectively. The results of our analyses revealed almost the same level of binding of both lectins to glycans present in two examined groups of juices (Fig. 4).
The relative amounts of complexes formed between sugar structures of gastric juices and DSA lectin (specific for Gal β 1–4 GlcNAc-R and GlcNAc-R linkages) were significantly higher after eradication treatment (P = 0.011) (Fig. 4).
NPA and GNA are lectins with specificity toward α 1–6 and α 1–3 linked mannose, present especially in N-glycoproteins. The relative amounts of above linkages were low in comparison with bonds revealed by other lectins, with very similar level before and at the end of eradication treatment (Fig. 4).
Pearson’s correlations between the amounts of examined sugar structures and the amounts of MUC 5AC and MUC 1 mucins in juices before treatment and at the end of eradication therapy were calculated. Mostly, the correlations between mentioned structures in two examined groups of juices were rather low. Moderate and high correlations in both groups of juices were found between the amounts of MUC 1 and H type 1 structure (r = 0.39 and 0.87 for juice before and at the end of the treatment, respectively). Such positive correlations were also revealed between MUC 5AC and structure recognized by SNA lectin (r = 0.47 and 0.46 for juice before and at the end of the treatment) and between MUC 5AC and structure recognized by LTA and UEA lectins (r = 0.8 and 0.48 for LTA and 0.39 and 0.32 for UEA for juice before and at the end of the eradication therapy, respectively). In case of MUC 5AC and Lewis b structure, correlations were also positive in both juices (r = 0.27 and 0.46). The values of all coefficients together with their statistical significances are summarized in Table 3.
Discussion
Analyses of carbohydrates of gastric juices before and at the end of eradication therapy revealed alterations caused likely by H. pylori infection. Because the examined material was taken from the void volume after gel filtration, we assume that analyzed structures originate mostly from high molecular mass mucins. Two mucins, MUC 1 and MUC 5AC, which are suggested to be involved in the mechanism of the infection, were analyzed. MUC 5AC is secretory one and can be normally present in gastric juice. MUC 1 is membrane-bound mucin, but it can be cleaved by host cell proteases and released to juice from gastric cell surface [17]. The higher level of both mucins was observed at the end of the treatment, which is in accordance with the results of some other investigations which revealed that H. pylori inhibits total mucin synthesis in gastric epithelial cells [18–20]. It is suggested that protective ability of gastric mucins may depend largely on their oligosaccharide chains. Alterations in the glycosylation pattern induced by the infection can impair the protective function of mucins. An increased level of MUC 1 mucin after eradication treatment was also observed in our earlier investigations when we examined this structure and also Lewis b and a blood group antigens using Western blotting and densitometry [15, 21].
Our results revealed increased level at the end of eradication therapy for only of those carbohydrate structures that are proposed to be involved in the interactions with H. pylori adhesins. The expression of fucosylated glycans was examined by anti-Lewis b, anti-H type 1 monoclonal antibodies, and AAA, UEA, and LTA lectins. Fuc α 1–2 linkage, which seems to be the most abundant, is present especially in peripheral Gal residues, which can be easily available for bacterial adhesins. Fuc α 1–2 bond is present in Lewis b and H type 1 structures, and these glycans were also observed in higher level at the end of the treatment. Therefore, our results support hypothesis about involvement of Lewis b and H type 1 structures in interactions with H. pylori [7–9, 11]. The depletion of these antigens in the infectious state might promote infection by enhancing the access of the bacterium to the epithelial surface [18]. Another explanation can also be taken into account. The decreased level of these possible bacterial receptors that can be located in MUC 1 and MUC 5AC mucin is suggested to be a kind of host defense. Some authors propose hypothesis with MUC 1 as a releasable decoy ligand for H. pylori that can be released from cell surface together with the adhered bacterium [7, 18]. Carbohydrate structures of MUC 1 mucin that possess long filamentous extracellular domain are considered to be the point of first direct contact between host cells and pathogenic organisms that penetrate the secreted mucus layer.
It is said that sialylated glycan structures are not typical for gastric mucins; they account for only about 3% of the total oligosaccharides (present in MUC 5AC mucin) [18], but they are also considered by some authors as potential receptors for bacterial adhesins [10, 12]. Sialylated forms are characteristic in H. pylori–infected specimens, and they decrease after eradication [10]. Surprisingly, in our study for both examined kinds of linkages, SA α 2–3 and SA α 2–6, the increased level in the recovered state was revealed. It is likely that high level of sialylation is due to the presence of highly sialylated, salivary MUC 5B mucin in gastric juice [22]. However, it was not explored in our study. The increase in sialyl Lewis x structure (with α SA 2–3 bond; recognized by monoclonal antibody) at the end of eradication therapy was significantly higher than that for SA α 2–3 bond detected by MAA lectin. This discrepancy can be explained by higher specificity of monoclonal antibodies than lectins during detection. Sialylation through α 2–6 bond is typical especially for short core carbohydrate structures and in our experiments was detected in low level, although with slight increase at the end of the therapy.
Gal β 1-4 GlcNAc structure (detected by DSA lectin), typical for O-glycosylated mucins, found also in sialyl Lewis x glycoform, was more abundant at the end of eradication treatment. This result is in accordance with general tendency of the increased level of examined mucins and glycoforms involved in interactions with H. pylori at the end of the treatment.
We observed no influence of the infection on the levels of short Tn and T carbohydrate structures. This result confirms the proposal that H. pylori influences only the peripheral sugar structures. Mannose residues, not typical in O-glycosidic chains, were detected in very low levels. These probably originate from rare N-glycosidic oligosaccharides that can be present in mucins [17].
As the mechanism of H. pylori infection has not been elucidated thoroughly, it is difficult to explain the mechanism of alterations induced by the bacterium. One possible explanation is that H. pylori can change the expression of genes involved in glycan synthesis such as transferases, crucial for the biosynthesis of potential bacterial receptors [18]. Interesting hypothesis about kind of relationship between two mucins (MUC 5AC and MUC 1) likely involved in the mechanism of infection has been proposed. MUC 5AC as more abundant one may at first catch Helicobacter pylori and then deliver it to the membrane-associated MUC 1 mucin. This mucin can cause signal transduction over the epithelial barrier and act as a releasable decoy. In this way, mucins together with the bacterium can be flushed away (Fig. 5) [7, 23]. The level of both mucins, with some specific sugar structures, acting as receptors for bacterial adhesins, decreases. These alterations are completely reversed after eradication [14].
The influence of omeprazole alone on examined structures also cannot be excluded. It is said that pH change (after omeprazole treatment) in Helicobacter pylori environment can result in its affinity to mucins, and bacteria cannot remain efficiently bound to mucus and are flushed away [12, 15, 24]. However, this was not examined in the present study.
From our results, we are not able to tell which of the glycan epitopes are present in which mucin. We can only suggest that H type 1 structure comes mostly from MUC 1 mucin as correlations between them in both groups of patients examined were positive (on moderate and high level). Similar assumptions can be taken for MUC 5 AC and Lewis b, SA α 2–6, Fuc α 1–3, and α 1–2 linkages because of positive values of Pearson’s coefficients. However, we should emphasize that above sugar structures can be also present in other glycoproteins not examined in this study. So we state that our concepts should be supported by more detailed examinations.
In conclusion, the observed changes in glycosylation pattern induced by H. pylori support the idea about the involvement of mucins and other glycan structures in the mechanism of the infection. We suggest that the knowledge about the exact action of the bacterium could contribute to looking for new therapeutic strategies.
References
Corfield AP, Myerscough N, Longman R, Sylvester P, Arul S, Pignatelli M (2000) Mucins and mucosal protection in the gastrointestinal tract: new prospects for mucins in the pathology of gastrointestinal disease. Gut 47:589–594
Uemura N, Okamoto S, Yamamoto S et al (2001) Helicobacter pylori infection and the development of gastric cancer. N Engl J Med 11:784–789
Linden SK, Sutton P, Karlsson NG, Korolik V, McGuckin MA (2008) Mucins in the mucosal barrier to infection. Mucosal Immunol 1:183–197
Nordman H, Davies JR, Lindell G, de Bolos C, Real F, Carlstedt I (2002) Gastric MUC 5AC and MUC 6 are large oligomeric mucins that differ in size, glycosylation and tissue distribution. Biochem J 364:191–200
Gendler SJ (2001) MUC 1, the renaissance molecule. J Mammary Gland Biol Neoplasia 6:339–353
Orczyk-Pawiłowicz M, Floriański J, Zalewski J, Kątnik-Prastowska I (2005) Relative amounts of sialic acid and fucose of amniotic fluid glycoconjugates in relation to pregnancy age. Glycoconjugate J 22:433–442
Linden S, Mahdavi J, Hedenbro J, Boren T, Carlstedt I (2004) Effects of pH on Helicobacter pylori binding to human gastric mucins; identification of binding to non-MUC 5AC mucins. Biochem J 384:263–270
Bovenkamp JHB, Mahdavi J, Korteland-Van Male AM et al (2003) The MUC 5AC glycoprotein is the primary receptor for Helicobacter pylori in the human stomach. Helicobacter 8:521–532
Linden S, Nordman H, Hedenbro J, Hurtig M, Boren T, Carlstedt I (2002) Strain- and blood group—dependent binding of Helicobacter pylori to human gastric MUC 5AC glycoforms. Gastroenterology 123:1923–1930
Mahdavi J, Sonden B, Hurtig M et al (2002) Helicobacter pylori SabA adhesin in persistent infection and chronic inflammation. Science 297:573–578
Ilver D, Arnaqvist A, Őrgen J et al (1998) Helicobacter pylori adhesin binding fucosylated histo-blood group antigens revealed by retagging. Science 279:373–377
Sheu BS, Odenbreit S, Hung KH et al (2006) Interaction between host gastric sialyl-Lewis x and H. pylori SabA enhances H. pylori density in patients lacking gastric Lewis b antigen. Am J Gastroenterol 101:36–44
McGuckin MA, Every AL, Skene CD, Linden SK et al (2007) Muc 1 mucin limits both Helicobacter pylori colonization of the murine gastric mucosa and associated gastritis. Gastroenterology 133:1210–1218
Ota H, Nakayama J, Momose M et al (1998) Helicobacter pylori infection produces reversible glycosylation changes to gastric mucins. Virchows Arch 433:419–426
Radziejewska I, Borzym-Kluczyk M, Kisiel DG, Namiot Z, Wosek J, Gindzieński A (2008) The effect of Helicobacter pylori eradication tratment on the MUC 1 and Lewis antigens level in human gastric juice: a preliminary study. Dig Dis Sci 53:2641–2645
Smith PK, Krohn RJ, Hermanson GT (1985) Measurement of protein using bicinchoninic acid. Anal Chem 150:76–85
Hanisch FG, Muller S (2000) MUC 1: the polymorphic appearance of human mucin. Glycobiology 10:439–449
Cooke CL, An HJ, Kim J et al (2009) Modification of gastric mucin oligosaccharide expression in rhesus macaques after infection with Helicobacter pylori. Gastroenterology 137:1061–1071
Byrd JC, Yunker CK, Xu Q-S, Sternberg LR, Bresalier RS (2000) Inhibition of gastric mucin synthesis by Helicobacter pylori. Gastroenterology 118:1072–1079
Kocer B, Ulas M, Ustundag Y et al (2004) A confirmatory report for the close interaction of Helicobacter pylori with gastric epithelial MUC 5AC expression. J Clin Gastroenterol 38:496–502
Radziejewska I, Kisiel DG, Borzym-Kluczyk M, Kluz A, Namiot Z, Gindzieński A (2007) MUC 1 mucin kontent in gastric juice of duodenal ulcer patients: effect of Helicobacter pylori eradication therapy. Clin Exp Med 7:72–76
Linden S, Wickstrom C, Lindell G, K Gilshenan, Carlstedt I (2008) Four models of adhesion are used during Helicobacter pylori binding to human mucins in the oral and gastric niches. Helicobacter 13:81–93
Linden S, Sheng Y, Every A et al (2009) MUC 1 limits Helicobacter pylori infection both by steric hindrance and by acting as releasable decoy. PLoS Pathog 5:e1000617
Radziejewska I, Gindzieński A, Wosek J, Kożuszyńska-Topór M, Namiot Z (2004) The influence of omeprazole treatment on MUC 1 mucin contents in gastric juice of Helicobacter pylori infected patients. Gastroenterol Pol 11:435–438
Yamashita K, Kochibe N, Ohkura T, Ueda I, Kobata A (1985) Fractionation of L-fucose-containing oligosaccharides on immobilized Aleuria auranta lectin. J Biol Chem 260:4688–4693
Audette GF, Vandonselaar M, Delbaere LTJ (2000) The 2.2 Å resolution structure of the O(H) blood-group-specific Lectin I from Ulex europaeus. J Mol Biol 304:423–433
Yan L, Wilkins PP, Alvarez-Manilla G, Do SI, Smith DF, Cummings RD (1997) Immobilized Lotus tetragonolobus agglutinin binds oligosaccharides containing the Lex determinant. Glycoconjugate J 14:45–55
Wang WC, Cummings RD (1988) The immobilized leukoagglutinin from the seeds of Maackia amurensis binds with high affinity to complex-type Asn-linked oligosaccharides containing terminal sialic acid-linked alpha-2, 3 to penultimate galactose residues. J Biol Chem 263:4576–4585
Shibuya N, Goldstein IJ, Broekaert WF, Nsimba-Lubaki M, Peeters B, Peumans WJ (1987) The elderberry (Sambucus nigra L.) bark lectin recognizes the Neu5Ac (alpha 2–6) Gal/GalNAc sequence. J Biol Chem 262:1596–1601
Sharma V, Vijayan M, Surolia A (1996) Imparting equisite specificity to peanut agglutinin for the tumor-associated Thomsen-Friedenreich antigen by redesign of its combining site. J Biol Chem 271:1209–21213
Wu AM (2004) Polyvalency of Tn (GalNAcα → Ser/Thr) glycotope as a critical factor for Vicia villosa B4 and glycoprotein interactions. FEBS Lett 562:51–58
Taketa K, Ichikawa E, Yamamoto T et al (1990) Datura stramonium agglutinin-reactive alpha-fetoprotein isoforms in hepatocellular carcinoma and other tumors. Tumour Biol 11:220–228
Lopez S, Codina C, Bastida J, Viladomat F, Davidson E, Stewart D (2002) Biodiversity of mannose-specific lectins within Narcissus species. J Agric Food Chem 50:2507–2513
Pusztai A, Grant G, Spencer RJ et al (1993) Kidney bean lectin-induced Escherichia coli overgrowth in the small intestine is blocked by GNA, a mannose-specific lectin. J Appl Bacteriol 75:360–368
Conflict of interest
None.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Radziejewska, I., Borzym-Kluczyk, M., Namiot, Z. et al. Glycosylation of mucins present in gastric juice: the effect of helicobacter pylori eradication treatment. Clin Exp Med 11, 81–88 (2011). https://doi.org/10.1007/s10238-010-0113-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10238-010-0113-6