Abstract
Patient management following a stroke currently represents a medical challenge. The presented study investigates the effect of immobilization on skeletal muscles in short positions after a stroke. A rat model was implemented in order to compare four situations within 14 days including control group, immobilization of one forelimb without stroke, stroke without immobilization and stroke with immobilization of the paretic forelimb. To analyze the changes of the mechanical properties of the passive skeletal muscle, the biological tissue is assumed to behave as a visco-hyperelastic and incompressible material characterized by the first-order Ogden’s strain energy function coupled with second-order Maxwell’s model. The material parameters were identified from inverse finite element method by using uniaxial relaxation tests data of skeletal muscle samples. Based on measurements of histological parameters, we observe that muscle immobilization led to microconstituents changes of skeletal muscles that were correlated with degradations of its mechanical properties. In the case of immobilization without stroke, the neurological behavior was also altered in the same manner as in the case of a stroke. We showed that immobilization of skeletal muscles in short positions produced contractile tissue atrophy, connective tissue thickening and alteration of passive mechanical behavior that were more damaging than the effects produced by a stroke. These results showed then that immobilization of skeletal muscles in short positions is highly deleterious with or without a stroke.






Similar content being viewed by others
References
Abo M, Miyano S, Eun SS, Yamauchi H (2004) Histochemical characterization of skeletal muscles in rats with photochemically-induced stroke. Brain Inj 18:1017–1024. https://doi.org/10.1080/02699050410001672305
Abraham AC, Kaufman KR, Donahue TLH (2013) Phenomenological consequences of sectioning and bathing on passive muscle mechanics of the New Zealand white rabbit tibialis anterior. J Mech Behav Biomed Mater 17:290–295. https://doi.org/10.1016/j.jmbbm.2012.10.003
Bloemberg D, Quadrilatero J (2012) Rapid determination of myosin heavy chain expression in rat, mouse, and human skeletal muscle using multicolor immunofluorescence analysis. PLoS ONE 7:e35273. https://doi.org/10.1371/journal.pone.0035273
Böl M, Kruse R, Ehret AE et al (2012) Compressive properties of passive skeletal muscle—the impact of precise sample geometry on parameter identification in inverse finite element analysis. J Biomech 45:2673–2679. https://doi.org/10.1016/j.jbiomech.2012.08.023
Böl M, Ehret AE, Leichsenring K et al (2014) On the anisotropy of skeletal muscle tissue under compression. Acta Biomater 10:3225–3234. https://doi.org/10.1016/j.actbio.2014.03.003
Booth FW, Kelso JR (1973) Effect of hind-limb immobilization on contractile and histochemical properties of skeletal muscle. Pflugers Arch 342:231–238
Booth CM, Cortina-Borja MJ, Theologis TN (2001) Collagen accumulation in muscles of children with cerebral palsy and correlation with severity of spasticity. Dev Med Child Neurol 43:314–320
Bosboom EMH, Hesselink MKC, Oomens CWJ et al (2001) Passive transverse mechanical properties of skeletal muscle under in vivo compression. J Biomech 34:1365–1368. https://doi.org/10.1016/S0021-9290(01)00083-5
Bouley J, Fisher M, Henninger N (2007) Comparison between coated vs. uncoated suture middle cerebral artery occlusion in the rat as assessed by perfusion/diffusion weighted imaging. Neurosci Lett 412:185–190. https://doi.org/10.1016/j.neulet.2006.11.003
Calvo B, Ramírez A, Alonso A et al (2010) Passive nonlinear elastic behaviour of skeletal muscle: experimental results and model formulation. J Biomech 43:318–325. https://doi.org/10.1016/j.jbiomech.2009.08.032
Chapman MA, Pichika R, Lieber RL (2015) Collagen crosslinking does not dictate stiffness in a transgenic mouse model of skeletal muscle fibrosis. J Biomech 48:375–378. https://doi.org/10.1016/j.jbiomech.2014.12.005
Chawla A, Mukherjee S, Karthikeyan B (2009) Characterization of human passive muscles for impact loads using genetic algorithm and inverse finite element methods. Biomech Model Mechanobiol 8:67–76. https://doi.org/10.1007/s10237-008-0121-6
Cheung DK, Climans SA, Black SE et al (2016) Lesion characteristics of individuals with upper limb spasticity after stroke. Neurorehabil Neural Repair 30:63–70. https://doi.org/10.1177/1545968315585357
Coq JO, Xerri C (1999) Tactile impoverishment and sensorimotor restriction deteriorate the forepaw cutaneous map in the primary somatosensory cortex of adult rats. Exp Brain Res 129:518–531
de Bruin M, Smeulders MJ, Kreulen M et al (2014) Intramuscular connective tissue differences in spastic and control muscle: a mechanical and histological study. PLoS ONE 9:e101038. https://doi.org/10.1371/journal.pone.0101038
De Deyne PG, Hafer-Macko CE, Ivey FM et al (2004) Muscle molecular phenotype after stroke is associated with gait speed. Muscle Nerve 30:209–215. https://doi.org/10.1002/mus.20085
Desgeorges MM, Devillard X, Toutain J et al (2017) Pharmacological inhibition of myostatin improves skeletal muscle mass and function in a mouse model of stroke. Sci Rep. https://doi.org/10.1038/s41598-017-13912-0
Dirks ML, Wall BT, Snijders T et al (2014) Neuromuscular electrical stimulation prevents muscle disuse atrophy during leg immobilization in humans. Acta Physiol Oxf Engl 210:628–641. https://doi.org/10.1111/apha.12200
Fluri F, Schuhmann MK, Kleinschnitz C (2015) Animal models of ischemic stroke and their application in clinical research. Drug Des Dev Ther 9:3445–3454. https://doi.org/10.2147/DDDT.S56071
Gautier S, Ouk T, Petrault O et al (2009) Neutrophils contribute to intracerebral haemorrhages after treatment with recombinant tissue plasminogen activator following cerebral ischaemia. Br J Pharmacol 156:673–679. https://doi.org/10.1111/j.1476-5381.2009.00068.x
Ghoreishy MHR (2012) Determination of the parameters of the Prony series in hyper-viscoelastic material models using the finite element method. Mater Des 35:791–797. https://doi.org/10.1016/j.matdes.2011.05.057
Gillies AR, Chapman MA, Bushong EA et al (2017) High resolution three-dimensional reconstruction of fibrotic skeletal muscle extracellular matrix. J Physiol 595:1159–1171. https://doi.org/10.1113/JP273376
Gracies J-M (2005) Pathophysiology of spastic paresis. II: Emergence of muscle overactivity. Muscle Nerve 31:552–571. https://doi.org/10.1002/mus.20285
Gracies J-M (2015) Coefficients of impairment in deforming spastic paresis. Ann Phys Rehabil Med 58:173–178. https://doi.org/10.1016/j.rehab.2015.04.004
Gras L-L, Mitton D, Viot P, Laporte S (2012) Hyper-elastic properties of the human sternocleidomastoideus muscle in tension. J Mech Behav Biomed Mater 15:131–140. https://doi.org/10.1016/j.jmbbm.2012.06.013
Gras L-L, Mitton D, Viot P, Laporte S (2013) Viscoelastic properties of the human sternocleidomastoideus muscle of aged women in relaxation. J Mech Behav Biomed Mater 27:77–83. https://doi.org/10.1016/j.jmbbm.2013.06.010
Gregory CM, Vandenborne K, Castro MJ, Dudley GA (2003) Human and rat skeletal muscle adaptations to spinal cord injury. Can J Appl Physiol Rev Can Physiol Appl 28:491–500
Hafer-Macko CE, Ryan AS, Ivey FM, Macko RF (2008) Skeletal muscle changes after hemiparetic stroke and potential beneficial effects of exercise intervention strategies. J Rehabil Res Dev 45:261–272
Holzapfel GA (1996) On large strain viscoelasticity: continuum formulation and finite element applications to elastomeric structures. Int J Numer Methods Eng 39:3903–3926. https://doi.org/10.1002/(SICI)1097-0207(19961130)39:22%3c3903:AID-NME34%3e3.0.CO;2-C
Honda Y, Sakamoto J, Nakano J et al (2015) Upregulation of interleukin-1β/transforming growth factor-β1 and hypoxia relate to molecular mechanisms underlying immobilization-induced muscle contracture. Muscle Nerve 52:419–427. https://doi.org/10.1002/mus.24558
Honda Y, Tanaka M, Tanaka N et al (2018) Relationship between extensibility and collagen expression in immobilized rat skeletal muscle. Muscle Nerve 57:672–678. https://doi.org/10.1002/mus.26011
Jalal N, Zidi M (2018) Effect of cryopreservation at −80°C on visco-hyperelastic properties of skeletal muscle tissue. J Mech Behav Biomed Mater 77:572–577. https://doi.org/10.1016/j.jmbbm.2017.10.006
Järvinen TAH, Józsa L, Kannus P et al (2002) Organization and distribution of intramuscular connective tissue in normal and immobilized skeletal muscles. An immunohistochemical, polarization and scanning electron microscopic study. J Muscle Res Cell Motil 23:245–254
Jones TA, Schallert T (1994) Use-dependent growth of pyramidal neurons after neocortical damage. J Neurosci Off J Soc Neurosci 14:2140–2152
Junqueira LC, Bignolas G, Brentani RR (1979) Picrosirius staining plus polarization microscopy, a specific method for collagen detection in tissue sections. Histochem J 11:447–455
Kneppers A, Leermakers P, Pansters N et al (2018) Coordinated regulation of skeletal muscle mass and metabolic plasticity during recovery from disuse. FASEB J. https://doi.org/10.1096/fj.201701403RRR
Lee SSM, Spear S, Rymer WZ (2015) Quantifying changes in material properties of stroke-impaired muscle. Clin Biomech 30:269–275. https://doi.org/10.1016/j.clinbiomech.2015.01.004
Leeuw T, Pette D (1996) Coordinate changes of myosin light and heavy chain isoforms during forced fiber type transitions in rabbit muscle. Dev Genet 19:163–168. https://doi.org/10.1002/(SICI)1520-6408(1996)19:2%3c163:AID-DVG8%3e3.0.CO;2-7
Li L, Rong W, Ke Z et al (2011) Muscle activation changes during body weight support treadmill training after focal cortical ischemia: a rat hindlimb model. J Electromyogr Kinesiol Off J Int Soc Electrophysiol Kinesiol 21:318–326. https://doi.org/10.1016/j.jelekin.2010.09.008
Lieber RL, Fridén J (2002) Spasticity causes a fundamental rearrangement of muscle-joint interaction. Muscle Nerve 25:265–270
Liu Y, Zhao Y, Huang F et al (2016) Combination of early constraint-induced movement therapy and fasudil enhances motor recovery after ischemic stroke in rats. Int J Neurosci 126:168–173. https://doi.org/10.3109/00207454.2014.998759
Longa EZ, Weinstein PR, Carlson S, Cummins R (1989) Reversible middle cerebral artery occlusion without craniectomy in rats. Stroke J Cereb Circ 20:84–91
Meyer GA, Lieber RL (2011) Elucidation of extracellular matrix mechanics from muscle fibers and fiber bundles. J Biomech 44:771–773. https://doi.org/10.1016/j.jbiomech.2010.10.044
Mohammadkhah M, Murphy P, Simms CK (2016) The in vitro passive elastic response of chicken pectoralis muscle to applied tensile and compressive deformation. J Mech Behav Biomed Mater 62:468–480. https://doi.org/10.1016/j.jmbbm.2016.05.021
Myers BS, Woolley CT, Slotter TL et al (1998) The influence of strain rate on the passive and stimulated engineering stress–large strain behavior of the rabbit tibialis anterior muscle. J Biomech Eng 120:126–132
Norvang OP, Hokstad A, Taraldsen K, et al (2018) Time spent lying, sitting, and upright during hospitalization after stroke: a prospective observation study. BMC Neurol 18:138. https://doi.org/10.1186/s12883-018-1134-0
Okita M, Yoshimura T, Nakano J et al (2004) Effects of reduced joint mobility on sarcomere length, collagen fibril arrangement in the endomysium, and hyaluronan in rat soleus muscle. J Muscle Res Cell Motil 25:159–166
Ouk T (2009) Ischémie cérébrale et interactions leucocyte-endothélium : modulation pharmacologique par les récepteurs nucléaires PPARs. Lille 2
Ouk T, Laprais M, Bastide M et al (2009) Withdrawal of fenofibrate treatment partially abrogates preventive neuroprotection in stroke via loss of vascular protection. Vasc Pharmacol 51:323–330. https://doi.org/10.1016/j.vph.2009.08.002
Parkkinen S, Ortega FJ, Kuptsova K et al (2013) Gait impairment in a rat model of focal cerebral ischemia. Stroke Res Treat 2013:410972. https://doi.org/10.1155/2013/410972
Picelli A, Tamburin S, Gajofatto F et al (2014) Association between severe upper limb spasticity and brain lesion location in stroke patients. Biomed Res Int 2014:e162754. https://doi.org/10.1155/2014/162754
Pontén EM, Stål PS (2007) Decreased capillarization and a shift to fast myosin heavy chain IIx in the biceps brachii muscle from young adults with spastic paresis. J Neurol Sci 253:25–33. https://doi.org/10.1016/j.jns.2006.11.006
Pontén E, Gantelius S, Lieber RL (2007) Intraoperative muscle measurements reveal a relationship between contracture formation and muscle remodeling. Muscle Nerve 36:47–54. https://doi.org/10.1002/mus.20780
Prado LG, Makarenko I, Andresen C et al (2005) Isoform diversity of giant proteins in relation to passive and active contractile properties of rabbit skeletal muscles. J Gen Physiol 126:461–480. https://doi.org/10.1085/jgp.200509364
Rogers DC, Campbell CA, Stretton JL, Mackay KB (1997) Correlation between motor impairment and infarct volume after permanent and transient middle cerebral artery occlusion in the rat. Stroke 28:2060–2066. https://doi.org/10.1161/01.STR.28.10.2060
Schipke J, Brandenberger C, Rajces A et al (2017) Assessment of cardiac fibrosis: a morphometric method comparison for collagen quantification. J Appl Physiol Bethesda Md 1985 122:1019–1030. https://doi.org/10.1152/japplphysiol.00987.2016
Shortland AP, Harris CA, Gough M, Robinson RO (2002) Architecture of the medial gastrocnemius in children with spastic diplegia. Dev Med Child Neurol 44:158–163
Smith LR, Barton ER (2014) Collagen content does not alter the passive mechanical properties of fibrotic skeletal muscle in mdx mice. Am J Physiol Cell Physiol 306:C889–898. https://doi.org/10.1152/ajpcell.00383.2013
Smith LR, Lee KS, Ward SR et al (2011) Hamstring contractures in children with spastic cerebral palsy result from a stiffer extracellular matrix and increased in vivo sarcomere length. J Physiol 589:2625–2639. https://doi.org/10.1113/jphysiol.2010.203364
Spector SA, Simard CP, Fournier M et al (1982) Architectural alterations of rat hind-limb skeletal muscles immobilized at different lengths. Exp Neurol 76:94–110. https://doi.org/10.1016/0014-4886(82)90104-2
Stevens L, Sultan KR, Peuker H et al (1999) Time-dependent changes in myosin chain mRNA and protein isoforms in unloaded soleus muscles of rat. Am J Physiol 277(6 Pt 1):C1122–C1129
Stevens L, Bastide B, Bozzo C, Mounier Y (2004) Hybrid fibres under slow-to-fast transformations: expression is of myosin heavy and light chains in rat soleus muscle. Pflüg Arch 448:507–514. https://doi.org/10.1007/s00424-004-1287-0
Strata F, Coq J-O, Byl N, Merzenich MM (2004) Effects of sensorimotor restriction and anoxia on gait and motor cortex organization: implications for a rodent model of cerebral palsy. Neuroscience 129:141–156. https://doi.org/10.1016/j.neuroscience.2004.07.024
Tabary JC, Tabary C, Tardieu C et al (1972) Physiological and structural changes in the cat’s soleus muscle due to immobilization at different lengths by plaster casts*. J Physiol 224:231–244. https://doi.org/10.1113/jphysiol.1972.sp009891
Townsend JR, Hoffman JR, Fragala MS et al (2016) A microbiopsy method for immunohistological and morphological analysis: a pilot study. Med Sci Sports Exerc 48:331–335. https://doi.org/10.1249/MSS.0000000000000772
Udaka J, Ohmori S, Terui T et al (2008) Disuse-induced preferential loss of the giant protein titin depresses muscle performance via abnormal sarcomeric organization. J Gen Physiol 131:33–41. https://doi.org/10.1085/jgp.200709888
Urso ML, Scrimgeour AG, Chen Y-W et al (2006) Analysis of human skeletal muscle after 48 h immobilization reveals alterations in mRNA and protein for extracellular matrix components. J Appl Physiol Bethesda Md 1985 101:1136–1148. https://doi.org/10.1152/japplphysiol.00180.2006
Van Loocke M, Lyons CG, Simms CK (2006) A validated model of passive muscle in compression. J Biomech 39:2999–3009. https://doi.org/10.1016/j.jbiomech.2005.10.016
Van Loocke M, Lyons CG, Simms CK (2008) Viscoelastic properties of passive skeletal muscle in compression: stress-relaxation behaviour and constitutive modelling. J Biomech 41:1555–1566. https://doi.org/10.1016/j.jbiomech.2008.02.007
Wheatley BB, Morrow DA, Odegard GM et al (2016a) Skeletal muscle tensile strain dependence: hyperviscoelastic nonlinearity. J Mech Behav Biomed Mater 53:445–454. https://doi.org/10.1016/j.jmbbm.2015.08.041
Wheatley BB, Odegard GM, Kaufman KR, Donahue TLH (2016b) How does tissue preparation affect skeletal muscle transverse isotropy? J Biomech. https://doi.org/10.1016/j.jbiomech.2016.06.034
Williams PE, Goldspink G (1984) Connective tissue changes in immobilised muscle. J Anat 138:343–350
Yamori Y, Horie R, Handa H et al (1976) Pathogenetic similarity of strokes in stroke-prone spontaneously hypertensive rats and humans. Stroke 7:46–53
Yang L, van der Werf KO, Dijkstra PJ et al (2012) Micromechanical analysis of native and cross-linked collagen type I fibrils supports the existence of microfibrils. J Mech Behav Biomed Mater 6:148–158. https://doi.org/10.1016/j.jmbbm.2011.11.008
Yaşar E, Adigüzel E, Kesikburun S et al (2016) Assessment of forearm muscle spasticity with sonoelastography in patients with stroke. Br J Radiol 89:20160603. https://doi.org/10.1259/bjr.20160603
Ye F, Baligand C, Keener JE et al (2013) Hindlimb muscle morphology and function in a new atrophy model combining spinal cord injury and cast immobilization. J Neurotrauma 30:227–235. https://doi.org/10.1089/neu.2012.2504
Zhang P, Zhang Q, Pu H et al (2012) Very early-initiated physical rehabilitation protects against ischemic brain injury. Front Biosci Elite Ed 4:2476–2489
Zogby AM, Dayanidhi S, Chambers HG et al (2017) Skeletal muscle fiber-type specific succinate dehydrogenase activity in cerebral palsy. Muscle Nerve 55:122–124. https://doi.org/10.1002/mus.25379
Zvejniece L, Svalbe B, Liepinsh E et al (2012) The sensorimotor and cognitive deficits in rats following 90- and 120-min transient occlusion of the middle cerebral artery. J Neurosci Methods 208:197–204. https://doi.org/10.1016/j.jneumeth.2012.05.018
Acknowledgements
This work was supported by University Paris-Est Créteil. The authors would like to thank Cécile Lecointe and Richard Souktani (technical chirurgical platform of the small animal, IMRB, University Paris-Est Créteil), HistIm platform of Cochin Institute (Paris) for histochemical and immunofluorescence staining. Primaries antibodies (BA-F8) and (SC-71) were obtained from DSHB (University of Iowa, USA).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
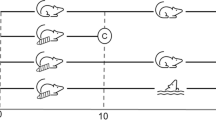
See Fig. 7.
The model was done under isoflurane anesthesia (5% for induction, 2.25–2.5% for maintenance via artificial ventilation in 30% oxygen and 70% nitrous oxide at l L/min). Surgical procedures were carried out as previously described (Ouk et al. 2009). First, having exposed the right carotid, it consists of ligating pterygopalatine, common carotid and external carotid arteries with silk sutures. Then, a temporary knot and an aneurismal clip were placed successively downstream of the puncture site on the common carotid artery. A 4/0 monofilament nylon was introduced through the right common carotid artery. Once filament got to the aneurysm clip, the knot was tightened and the clip was removed. Finally, the monofilament was gently advanced of almost 20–22 mm into the internal carotid artery until resistance is felt, meaning that the rounded head of monofilament reached the middle cerebral artery. The monofilament rounded head was obtained by burning the filament end and optimized for a diameter of. After 60 min, the monofilament was removed until the rounded head was blocked by the ligature. All the silk sutures and the monofilament were left in place. Note that body temperature was maintained at by a heated surgery table. The recovering place is a controlled room at 27° with an oxygen adjunction. Then, once awake, rats were placed in a cage at ambient temperature with the possibility to eat and drink ad libitum. It should be underlined that the control operation (for control and immobilized groups) consists in 60-min anesthesia and same handling without advance the monofilament until the obstruction.
Illustration of the semiautomatic collagen analysis. a Initial part of red Sirius slice. b Analyzed slice from k-mean clustering (k = 4) with endomysium in blue and perimysium in red. c Cluster including muscle fiber. d Cluster including white background. e Cluster including endomysium f Cluster including perimysium. In order to illustrate the process, the endomysium and perimysium cluster was colored in blue and red, respectively. Some misallocations remain after first step (k-mean clustering). That is to say endomysium in perimysium cluster and vice versa. There were manually corrected by the user with a polygonal tool
Illustration of the semiautomatic immunohistology analysis. a Cross section incubated in primary antibody collagen against MHCI and MHCII. b Slice subdivision with selected region of interest (ROI) of one myofiber. Each myofiber was selected and a mean {Green;Blue} doublet was computed inside each ROI. c Myofiber automatically assigning using a K-mean clustering (k = 3)
Whether it is for all groups (black solid line), for immobilized group (orange dotted line) or non-immobilized group (blue dotted line), we observe a strong correlation between biceps brachii wet weight and body weight (Fig. 8a). Furthermore, we show that muscle weight and cerebral infarct size are negatively correlated as previously described by Parkkinen et al. (2013) (Fig. 8b).
Rights and permissions
About this article
Cite this article
Jalal, N., Gracies, JM. & Zidi, M. Mechanical and microstructural changes of skeletal muscle following immobilization and/or stroke. Biomech Model Mechanobiol 19, 61–80 (2020). https://doi.org/10.1007/s10237-019-01196-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10237-019-01196-4