Abstract
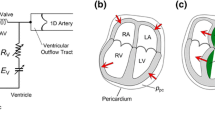
During diastole, coronary perfusion depends on the pressure drop between the myocardial tissue and the coronary origin located at the aortic root. This pressure difference is influenced by the flow field near the closing valve leaflets. Clinical evidence is conclusive that patients with severe aortic stenosis (AS) suffer from diastolic dysfunction during hyperemia, but show increased coronary blood flow (CBF) during rest. Transcatheter aortic valve implantation (TAVI) was shown to decrease rest CBF along with its main purpose of improving the aortic flow and reducing the risk of heart failure. Physiological or pathological factors do not provide a clear explanation for the increase in rest CBF due to AS and its decrease immediately after TAVI. In this manuscript, we present a numerical study that examines the impact of AS and TAVI on CBF during rest conditions. The study compares the hemodynamics of five different 2D numerical models: a baseline “healthy valve” case, two AS cases and two TAVI cases. The analysis used time-dependent computational fluid–structure interaction simulations of blood flow in the aortic root including the dynamics of the flexible valve leaflets and the varying resistance of the coronary arteries. Despite its simplifications, our 2D model succeeded to capture the major effects that dominate the hemodynamics in the aortic root and to explain the hemodynamic effect that leads to the changes in CBF found in in vitro and clinical studies.


















Similar content being viewed by others
References
ADINA R&D I (2000) ADINA theory and modeling guide vol Volumes I, II and III,. Watertown, MA
Ahn J-H et al (2016) Coronary microvascular dysfunction as a mechanism of angina in severe AS: prospective adenosine-stress CMR study. J Am Coll Cardiol 67:1412–142
Avrahami I (2012) Cardiovascular vortex in numerical simulations. In: Kheradvar A, Pedrizzetti G (eds) Vortex formation in cardiovascular system. Springer, Berlin
Bakhtiary F et al (2007) Impact of patient–prosthesis mismatch and aortic valve design on coronary flow reserve after aortic valve replacement. J Am Coll Cardiol 49:790–796
Bathe K-J (2006) Finite element procedures. Klaus-Jurgen Bathe, Berlin
Bellhouse B (1972) The fluid mechanics of heart valves. In: Bergel DH (ed) Cardiovascular fluid dynamics. Academic Press, London
Ben-Dor I et al (2009) Effects of percutaneous aortic valve replacement on coronary blood flow assessed with transesophageal Doppler echocardiography in patients with severe aortic stenosis. Am J Cardiol 104:850–855
Ben-Dor I et al (2014) Coronary blood flow in patients with severe aortic stenosis before and after transcatheter aortic valve implantation. Am J Cardiol 114:1264–1268
Berne R, Levy M (1986) Cardiovascular physiology. Mosby, St. Louis PN Watton et al./J Fluids Struct 24 (2008) 58 74:72
Bertrand ME, Lablanche JM, Tilmant PY, Thieuleux FP, Delforge MR, Carré AG (1981) Coronary sinusblood flow at rest and during isometric exercise in patients with aortic valve disease: mechanism of angina pectoris in presence of normal coronary arteries. Am J Cardiol 47:199–205
Bianchi M, Ghosh RP, Marom G, Slepian MJ, Bluestein D (2015) Simulation of transcatheter aortic valve replacement in patient-specific aortic roots: effect of crimping and positioning on device performance. In: Engineering in Medicine and Biology Society (EMBC), 2015 37th annual international conference of the IEEE, IEEE, pp 282–285
Bissell MM, Dall’Armellina E, Choudhury RP (2014) Flow vortices in the aortic root: in vivo 4D-MRI confirms predictions of Leonardo da Vinci European heart journal:ehu011
Bluestein D, Einav S (2001) Techniques in the stability analysis of pulsatile flow through heart valves. In: Leondes Cornelius T (ed) Cardiovascular techniques, biomechanical systems. techniques and applications. CRC Press, Boca Raton
Borazjani I (2013) Fluid-structure interaction, immersed boundary-finite element method simulations of bio-prosthetic heart valves. Computer Methods in Applied Mechanics and Engineering 257:103–116
Broyd CJ, Sen S, Mikhail GW, Francis DP, Mayet J, Davies JE (2013) Myocardial ischemia in aortic stenosis: insights from arterial pulse-wave dynamics after percutaneous aortic valve replacement. Trends Cardiovasc Med 23:185–191
Burwash IG et al (2008) Myocardial blood flow in patients with low-flow, low-gradient aortic stenosis: differences between true and pseudo-severe aortic stenosis Results from the multicentre TOPAS (Truly or Pseudo-Severe Aortic Stenosis). Study Heart 94:1627–1633
Calderan J, Mao W, Sirois E, Sun W (2015) Development of an in vitro model to characterize the effects of transcatheter aortic valve on coronary artery flow. Artif Org 40:612–619
Camici PG, Olivotto I, Rimoldi OE (2012) The coronary circulation and blood flow in left ventricular hypertrophy. J Mol Cell Cardiol 52:857–864
Cao C, Virk S, Liou K, Pathan F, Wilcox C, Novis E, Yan T (2015) A systematic review and meta-analysis of clinical and cost-effective outcomes of transcatheter aortic valve implantation versus surgical aortic valve replacement Heart. Lung Circ 24:S258
Carroll R, Falsetti H (1976) Retrograde coronary artery flow in aortic valve disease. Circulation 54:494–499
Christie GW, Barratt-Boyes BG (1995) Age-dependent changes in the radial stretch of human aortic valve leaflets determined by biaxial testing. Ann Thorac Surg 60:S156–S159
Danson E, Hansen P, Sen S, Davies J, Meredith I, Bhindi R (2016) Assessment, treatment, and prognostic implications of CAD in patients undergoing TAVI. Nat Rev Cardiol 13:276
Dasi L, Ge L, Simon H, Sotiropoulos F, Yoganathan A (2007) Vorticity dynamics of a bileaflet mechanical heart valve in an axisymmetric aorta. Phys Fluids 19:067105
Davies JE et al (2011) Arterial pulse wave dynamics after percutaneous aortic valve replacement fall in coronary diastolic suction with increasing heart rate as a basis for angina symptoms in aortic stenosis. Circulation 124:1565–1572
De Tullio MD, Cristallo A, Balaras E, Verzicco R (2009) Direct numerical simulation of the pulsatile flow through an aortic bileaflet mechanical heart valve. J Fluid Mech 622:259–290
De Vita F, de Tullio M, Verzicco R (2016) Numerical simulation of the non-Newtonian blood flow through a mechanical aortic valve. Theor Comput Fluid Dyn 30:129–138
Doyle MG, Tavoularis S, Bourgault Y (2010) Application of parallelprocessing to the simulation of heart mechanics. In: Mewhort DJK (ed) High performance computing systems and applications, Springer, Berlin, pp 30–47
Ducci A, Tzamtzis S, Mullen M, Burriesci G (2012) Phase-resolved velocity measurements in the Valsalva sinus downstream of a Transcatheter Aortic Valve. In: 16th International symposium on applications of laser techniques to fluid mechanics, Lisbon, Portugal, pp 9–12
Dvir D et al (2012) Multicenter evaluation of Edwards SAPIEN positioning during transcatheter aortic valve implantation with correlates for device movement during final deployment. JACC Cardiovasc Interv 5(5):563–570
Dvir D, Lavi I, Kornowski R (2013) Transcatheter aortic valve implantation of a CoreValve device using novel real-time imaging guidance. Cardiovasc Revascularization Med 14(1):49–52
Eberli F, Ritter M, Schwitter J, Bortone A, Schneider J, Hess O, Krayenbuehl H (1991) Coronary reserve in patients with aortic valve disease before and after successful aortic valve replacement. Eur Heart J 12:127–138
Fung YC (1993) Biomechanics: mechanical properties of living tissues. Springer, Berlin
Gaillard E, Garcia D, Kadem L, Pibarot P, Durand L-G (2010) In vitro investigation of the impact of aortic valve stenosis severity on left coronary artery flow. J Biomech Eng 132:044502
Garcia D, Camici PG, Durand L-G, Rajappan K, Gaillard E, Rimoldi OE, Pibarot P (2009) Impairment of coronary flow reserve in aortic stenosis. J Appl Physiol 106:113–121
Garcia D, Kadem L, Savéry D, Pibarot P, Durand L-G (2006) Analytical modeling of the instantaneous maximal transvalvular pressure gradient in aortic stenosis. J Biomech 39:3036–3044
Ge L, Leo HL, Sotiropoulos F, Yoganathan AP (2005) Flow in a mechanical bileaflet heart valve at laminar and near-peak systole flow rates: CFD simulations and experiments. J Biomech Eng Trans ASME 127:782–797
Ge L, Sotiropoulos F (2010) Direction and magnitude of blood flow shear stresses on the leaflets of aortic valves: is there a link with valve calcification? J Biomech Eng Trans ASME 132:014505
Gharib M, Kremers D, Koochesfahani M, Kemp M (2002) Leonardo’s vision of flow visualization. Exp Fluids 33:219–223
Gilmanov A, Le TB, Sotiropoulos F (2015) A numerical approach for simulating fluid structure interaction of flexible thin shells undergoing arbitrarily large deformations in complex domains. J Comput Phys 300:814–843
Gould K, Lipscomb K, Hamilton G, Kennedy J (1976) Retrograde coronary artery flow in aortic valve disease. Circulation 54:494–499
Gould KL, Carabello BA (2003) Why angina in aortic stenosis with normal coronary arteriograms? Circulation 107:3121–3123
Gould KL, Johnson NP (2016a) Imaging coronary blood flow in AS: let the data talk. Again J Am Coll Cardiol 67:1423–1426
Gould KL, Johnson NP (2016b) Ischemia in aortic stenosis: new insights and potential clinical relevance. J Am Coll Cardiol 68:698–701
Grande-Allen KJ, Cochran RP, Reinhall PG, Kunzelman KS (2000) Re-creation of sinuses is important for sparing the aortic valve: a finite element study. J Thorac Cardiovascul Surg 119:753–763
Grande-Allen KJ, Cochran RP, Reinhall PG, Kunzelman KS (2001) Finite-element analysis of aortic valve-sparing: influence of graft shape and stiffness. IEEE Trans Biomed Eng 48:647–659
Griffith BE (2012) Immersed boundary model of aortic heart valve dynamics with physiological driving and loading conditions. Int J Numer Methods Biomed Eng 28:317–345
Hongo M et al (1993) Relation of phasic coronary flow velocity profile to clinical andhemodynamic characteristics of patients with aortic valve disease. Circulation 88:953–960
Julius BK, Spillmann M, Vassalli G, Villari B, Eberli FR, Hess OM (1997) Angina pectoris in patients with aortic stenosis and normal coronary arteries mechanisms and pathophysiological concepts. Circulation 95:892–898
Kelly TA, Rothbart RM, Cooper CM, Kaiser DL, Smucker ML, Gibson RS (1988) Comparison of outcome of asymptomatic to symptomatic patients older than 20 years of age with valvular aortic stenosis. Am J Cardiol 61:123–130
Kilner PJ, Yang GZ, Mohiaddin RH, Firmin DN, Longmore DB (1993) Helical and retrograde secondary flow patterns in the aortic arch studied by three-directional magnetic resonance velocity mapping. Circulation 88:2235–2247
Kim HJ, Vignon-Clementel IE, Coogan JS, Figueroa CA, Jansen KE, Taylor CA (2008) Patient-specific modeling of blood flow and pressure in human coronary arteries. Ann Biomed Eng 38:3195–3209
Klabunde R (2011) Cardiovascular physiology concepts. Lippincott Williams and Wilkins, Philadelphia
Kolh P et al (2014) 2014 ESC/EACTS guidelines on myocardial revascularization the task force on myocardial revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur J Cardio-Thorac Surg 46:517–592
Kopanidis A, Pantos I, Alexopoulos N, Theodorakakos A, Efstathopoulos E, Katritsis D (2015) Aortic Flow patterns after simulated implantation of transcatheter aortic valves. Hell J Cardiol 56:418–428
Kupari M et al (1992) Exclusion of coronary artery disease by exercise thallium-201 tomography in patients withaortic valve stenosis. Am J Cardiol 70:635–640
Kvitting J-PE, Ebbers T, Wigström L, Engvall J, Olin CL, Bolger AF (2004) Flow patterns in the aortic root and the aorta studied with time-resolved, 3-dimensional, phase-contrast magneticresonance imaging: implications for aortic valve-sparing surgery. J Thorac Cardiovascul Surg 127:1602–1607
Kwon S-S et al (2014) A novel patient-specific model to compute coronary fractional flow reserve. Prog Biophys Mol Biol 116:48–55
Labrosse MR, Beller CJ, Robicsek F, Thubrikar MJ (2006) Geometric modeling of functional trileaflet aortic valves: development and clinical applications. J Biomech 39:2665–2672
Lantz J, Ebbers T, Engvall J, Karlsson M (2013) Numerical and experimental assessment of turbulent kinetic energy in an aortic coarctation. J Biomech 46:1851–1858
Le TB, Gilmanov A, Sotiropoulos F (2013) High resolution simulation of tri-leaflet aortic heart valve in an idealized aorta. J Med Dev 7:030930
Lee J, Nordsletten D, Cookson A, Rivolo S, Smith N (2016) In silico coronary wave intensity analysis: application of an integrated one-dimensional and poromechanical model of cardiac perfusion. Biomech Model Mechanobiol 15:1535–1555
Lee J, Smith NP (2012) The multi-scale modelling of coronary blood flow. Ann Biomed Eng 40:2399–2413
Lumley M et al (2016) Coronary physiology during exercise and vasodilation in the healthy heart and in severe aorticstenosis. J Am Coll Cardiol 68:688–697
Mahmood F, Swaminathan M (2010) Stuck With a Decision: What Is the “True” aortic valve area—anatomic, geometric, or effective orifice area?. WB Saunders, Philadelphia
Marcus ML, Doty DB, Hiratzka LF, Wright CB, Eastham CL (1982) Decreased coronary reserve: a mechanism for angina pectoris in patients with aortic stenosis and normal coronary arteries. New Engl J Med 307:1362–1366
Marn J, Iljaž J, Žunič Z, Ternik P (2012) Non-Newtonian blood flow around healthy and regurgitated aortic valve with coronary blood flow involved Strojniški vestnik. J Mech Eng 58:482–491
Marom G, Haj-Ali R, Raanani E, Schäfers H-J, Rosenfeld M (2011) A fluid–structure interaction model of the aortic valve with coaptation and compliant aortic root. Med Biol Eng Comput Sci Eng 50:173–182
Marom G, Haj-Ali R, Raanani E, Schäfers H-J, Rosenfeld M (2012) A fluid-structure interaction model of the aortic valve with coaptation and compliant aorticroot. Med Biol Eng Comput 50:173–182
McQueen DM, Peskin CS (2000) A three-dimensional computer model of the human heart for studying cardiac fluid dynamics. Comput Gr Us 34:56–60
Meimoun P et al (2012) Factors associated with noninvasive coronary flow reserve in severe aortic stenosis. J Am Soc Echocardiogr 25:835–841
Miller JD, Weiss RM, Heistad DD (2011) Calcific aortic valve stenosis: methods, models, and mechanisms. Circ Res 108:1392–1412
Nicosia M, Cochran R, Einstein D, Rutland C, Kunzelman K (2003) A coupled fluid-structure finite element model of the aortic valve and root. J Heart Balve Dis 12:781–789
Nobari S, Mongrain R, Leask R, Cartier R (2013) The effectof aortic wall and aortic leaflet stiffening on coronary hemodynamic: a fluid-structure interaction study. Med Biol Eng Comput 51:923–936
Nobili M et al (2008) Numerical simulation of the dynamics of a bileaflet prosthetic heart valve using a fluid-structure interaction approach. J Biomech 41:2539–2550
Omran H, Fehske W, Rabahieh R, Hagendorff A, Lüderitz B (1996) Relation between symptoms and profiles of coronary artery blood flow velocities in patients with aortic valve stenosis: a study using transoesophageal Doppler echocardiography. Heart 75:377–383
Paradis J-M et al (2014) Aortic stenosis and coronary artery disease: What do we know? What don’t we know? A comprehensive review of the literature with proposed treatment algorithms. Eur Heart J 35:2069–2082
Peacock JA (1990) An in vitro study of the onset of turbulence in the sinus of Valsalva. Circ Res 67:448–460
Petropoulakis PN, Kyriakidis MK, Tentolouris CA, Kourouclis CV, Toutouzas PK (1995) Changes in phasic coronary blood flow velocity profile in relation to changes in hemodynamic parameters during stress in patients with aortic valve stenosis. Circulation 92:1437–1447
Querzoli G, Fortini S, Espa S, Costantini M, Sorgini F (2014) Fluid dynamics of aortic root dilation in Marfan syndrome. J Biomech 47:3120–3128
Rajappan K, Rimoldi OE, Camici PG, Bellenger NG, Pennell DJ, Sheridan DJ (2003) Functional changes in coronary microcirculation after valve replacement in patients withaortic stenosis. Circulation 107:3170–3175
Rajappan K, Rimoldi OE, Dutka DP, Ariff B, Pennell DJ, Sheridan DJ, Camici PG (2002) Mechanisms of coronary microcirculatory dysfunction in patients with aortic stenosis and angiographically normal coronary arteries. Circulation 105:470–476
Rolandi MC et al (2016) Transcatheter replacement of stenotic aortic valve normalizes cardiac–coronary interaction by restoration of systolic coronary flow dynamics as assessed by wave intensity analysis. Circ Cardiovascul Interv 9:e002356
Rosenhek R et al (2010) Natural history of very severe aortic stenosis. Circulation 121:151–156
Sacks MS, Sun W (2003) Multiaxial mechanical behavior of biological materials. Annu Rev Biomed Eng 5:251–284
Scalone G, Niccoli G (2015) A focus on the prognosis and management of ischemic heart disease in patients without evidence of obstructive coronary artery disease. Expert Rev Cardiovasc Ther 13:1031–1044. doi:10.1586/14779072.2015.1077114
Schiestel R (2010) Modeling and simulation of turbulent flows, vol 4. Wiley, Hoboken
Schultz CJ et al (2009) Geometry and degree of apposition of the CoreValve ReValving system with multislice computed tomography after implantation in patients with aortic stenosis. J Am Coll Cardiol 54:911–918
Sen S, Davies JE (2015) Demystifying Complex Coronary Hemodynamics in Patients Undergoing Transcatheter Aortic Valve Replacement Sowing the Seeds for Coronary Physiological Assessment in the Future? Circ Cardiovasc Interv 8:e002909
Sotiropoulos F (2015) Fluid mechanics of heart valves and their replacements. Annu Rev Fluid Mech 48:259–283
Sotiropoulos F, Borazjani I (2009) A review of state-of-the-art numerical methods for simulating flow through mechanical heart valves. Med Biol Eng Comput 47:245–256
Stefanadis C, Wooley C, Bush C, Kolibash A, Boudoulas H (1988) Aortic distensibility in post-stenotic aortic dilatation: the effect of co-existing coronary artery disease. J Cardiol 18:189–195
Stefanini G, Stortecky S, Wenaweser P, Windecker S (2014) Coronary artery disease in patients undergoing TAVI: why, what, when and how to treat EuroIntervention: journal of EuroPCR in collaboration with the Working Group on InterventionalCardiology of the European Society of. Cardiology 10:U69–75
Thubrikar MJ (1989) The aortic valve. CRC Press, Boca Raton
Varghese SS, Frankel SH, Fischer PF (2008) Modeling transition to turbulence in eccentric stenotic flows. J Biomech Eng 130:014503–014507. doi:10.1115/1.2800832
Weinberg EJ, Mack PJ, Schoen FJ, García-Cardeña G, Mofrad MRK (2010) Hemodynamic environments from opposing sides of human aortic valve leaflets evoke distinct endothelial phenotypes in vitro. Cardiovasc Eng 10:5–11
Weinberg EJ, Schoen FJ, Mofrad MR (2009) A computational model of aging and calcification in the aortic heart valve. PloS ONE 4:e5960
Wiegerinck EM et al (2015) Impact of aortic valve stenosis on coronary hemodynamics and the instantaneouseffect of transcatheter aortic valve implantation. Circ Cardiovasc Interv 8:e002443
Yap CH, Saikrishnan N, Tamilselvan G, Yoganathan AP (2012) Experimental measurement of dynamic fluid shear stress on the aortic surface of the aortic valve leaflet. Biomech Model Mechanobiol 11:171–182
Yoganathan AP, Chandran KB, Sotiropoulos F (2005) Flow in prosthetic heart valves: state-of-the-art and future directions. Ann Biomed Eng 33:1689–1694
Zhang H, Bathe K-J (2001) Direct and iterative computing of fluid flows fully coupled with structures. In: Bathe KJ (ed), Computational fluid and solid mechanics. Elsevier, Amsterdam
Zingone B (2008) Impaired coronary flow reserve with aortic stenosis despite aortic valve replacement. J Cardiovasc Med 9:869–871
Acknowledgements
This work was conducted in Ariel Biomechanics Center (ABMC) in Ariel University. Shaily Wald was supported by scholarship provided by Ariel University. The research was partially supported by a grant from the Nicholas and Elizabeth Slezak Super Center for Cardiac Research and Biomedical Engineering at Tel Aviv University, in collaboration with Prof. Ran Kornowski, Rabin Medical Center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Appendix
Appendix
1.1 Model validation
1.1.1 Time step independence tests
Mesh and time step independence tests were conducted to validate the numerical model. To evaluate the optimal time step size for the transient simulations, simulations of the healthy case with the mesh of 30,000 nodes were performed using 5 different time step intervals of dt = 5, 10, 15, 20 and 25 ms. The resulted velocity magnitude for the different time steps intervals are shown in Fig. 19 corresponding to \(t=0.42\,\hbox {s}\).
For all the cases, at \(t = 0.5\,\hbox {s}\), the time step is reduced to dt = 1 ms to allow converge at the delicate stage of valve closure. Figure 20 shows a comparison of the average coronary velocity during the cardiac cycle for the five cases of time step resolutions.
To evaluate the discretization error, we calculated the relative difference (ERR) between the average coronary flow of each case and the finest time resolution case, as follows:
where \(V_{y}\) is the time-dependent average coronary velocity (as described by Eq. 5) and T is the cycle period. Table 5 details the average ERR of the different cases. The results show that the time step of dt = 10 ms is sufficient during systole, with ERR = 1.5%. During diastole (t > 0.5 s), steps of 1 ms were used to allow convergence. Therefore, for the transient analyses in this study, 551 steps were set per cycle.
1.1.2 Mesh independence tests
To evaluate the optimal mesh resolution, five models of the healthy base case with different mesh resolutions were built (with 20,000–60,000 nodes). The models were simulated during a period of one cardiac cycle. Figure 21 shows a comparison of the average coronary velocity during the cardiac cycle for the five mesh resolutions and Table 6 details the average relative differences of the different cases. Based on these results, mesh resolutions of 30,000 nodes were found suitable for our model with ERR = 4% of the finest mesh.
1.1.3 Comparison with in vitro results
The numerical study was conducted in parallel to an experimental study that was performed by another member in our group (to be published in a future publication). The study included a healthy, AS and TAVI in vitro models with similar characteristics as the numerical model described here (Fig. 22). The flow was driven by a pulsatile piston pump which was synchronized with a controlled coronary arteries resistance. Similar working conditions (HR and CO) were used. Measurement of coronary flow rates are shown as red columns in Fig. 23. Although only one AS model (severe AS) and one TAVI model (the long TAVI) were modeled in the in vitro study, the experimental results agree with the numerical results. AS case showed higher coronary flow than healthy case, and TAVI leads to normalization of the coronary flow.
Rights and permissions
About this article
Cite this article
Wald, S., Liberzon, A. & Avrahami, I. A numerical study of the hemodynamic effect of the aortic valve on coronary flow. Biomech Model Mechanobiol 17, 319–338 (2018). https://doi.org/10.1007/s10237-017-0962-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10237-017-0962-y