Abstract
Purpose
Idiopathic pulmonary fibrosis (IPF) is a type of interstitial lung disease found mostly in elderly persons, characterized by a high symptom burden and frequent encounters with health services. This study aimed to quantify the economic burden of IPF in Australia with a focus on resource utilization and associated direct costs.
Methods
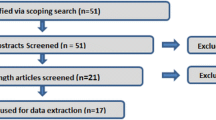
Participants were recruited from the Australian IPF Registry (AIPFR) between August 2018 and December 2019. Data on resource utilization and costs were collected via cost diaries and linked administrative data. Clinical data were collected from the AIPFR. A “bottom up” costing methodology was utilized, and the costing was performed from a partial societal perspective focusing primarily on direct medical and non-medical costs. Costs were standardized to 2021 Australian dollars ($).
Results
The average annual total direct costs per person with IPF was $31,655 (95% confidence interval (95% CI): $27,723–$35,757). Extrapolating costs based on prevalence estimates, the total annual costs in Australia are projected to be $299 million (95% CI: $262 million–$338 million). Costs were mainly driven by antifibrotic medication, hospital admissions and medications for comorbidities. Disease severity, comorbidities and antifibrotic medication all had varying impacts on resource utilization and costs.
Conclusion
This cost-of-illness study provides the first comprehensive assessment of IPF-related direct costs in Australia, identifies the key cost drivers and provides a framework for future health economic analyses. Additionally, it provided insight into the major cost drivers which include antifibrotic medication, hospital admissions and medications related to comorbidities. Our findings emphasize the importance of the appropriate management of comorbidities in the care of people with IPF as this was one of the main reasons for hospitalizations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Idiopathic pulmonary fibrosis (IPF) is a form of interstitial lung disease (ILD) characterized by progressive fibrosis of the lung parenchyma which results in a progressive decline in lung function, respiratory failure and eventual death [1]. It more commonly occurs in elderly persons above the age of 60 years, most frequently in males. Median survival time is typically 3–5 years from diagnosis [1, 2]. IPF is usually associated with a high symptom burden, typified by progressively worsening cough and shortness of breath, which have a significant impact on health-related quality of life (HRQoL) [1]. Considering that IPF often affects elderly persons, multiple comorbidities are commonly present, and it is now understood that these some of these comorbidities have an important impact on clinical outcomes [3]. Given the aforementioned, persons with IPF generally have frequent encounters with health services which can place an immense burden on health resources [4].
Disease specific therapeutic options for IPF are limited. Only two antifibrotic medications (pirfenidone and nintedanib) have been approved for persons with mild to moderate IPF [1]. Antifibrotic medication is quite costly with costs varying across countries from $2000 to $14,000 per person per month [4, 5]. These were approved for subsidization 2017 in Australia and incurred costs of approximately $139 million over a 3-year period (2017–2020) [6]. In addition to costly medications, people with IPF may require long-term oxygen, palliative care or lung transplants, all of which are costly [4, 7].
Internationally, there is a limited body of evidence on costs and resource utilization associated with IPF and almost no data from after the approval of antifibrotic treatment [4]. This is also the case in Australia [6]. Quantifying the economic burden of diseases is essential for health-care decision-making, to maximize efficient use of limited resources and to ensure access to essential treatments and services. For this reason, this study sought to characterize the economic burden of IPF in Australia, by assessing the direct costs and associated health care resource utilization over a 12-month period in a cohort of people living with IPF.
Methods
Study perspective
This retrospective cost of illness study was part of a broader study under the National Health and Medical Research Council (NHMRC), Centre for Research Excellence for Pulmonary Fibrosis (CRE-PF) [8]. Costs were analyzed for the 12-month period prior to recruitment into the study. A “bottom up” costing methodology was utilized, and the costing was performed from a partial societal perspective (Australian Government and patient) focusing primarily on direct costs, which are costs incurred by the health system, society, family or individual patient [9]. Indirect costs, which include productivity losses due to morbidity and mortality, borne by the individual, family, society, or the employer, were not included in this analysis as most participants were of retirement age [9].
Study participants
Participants for this study were recruited between August 2018 and December 2019 from the Australian IPF Registry (AIPFR), a national multi-centre, prospective registry of IPF patients facilitated by the Lung Foundation of Australia (LFA) [10, 11]. Details on the recruitment methodology for the AIFPR have been previously described [10]. Participation was voluntary through informed consent, and withdrawal was possible at any time without reason. More details are provided in supplement S1.
Data sources
Cost diary data were collected via a predesigned paper-based survey instrument, which also collected socio-demographic information, information on treatment and on comorbidities. Clinical information was retrieved from the AIPFR database and included pulmonary function tests (PFT) to ascertain disease severity levels, and body mass index (BMI). Administrative data for health resource utilization and associated costs were obtained via data linkage from the Commonwealth Department of Health, the Centre for Health Record Linkage (CHeReL), the Tasmanian Data Linkage Unit (TDLU) and the Centre for Victorian Data Linkage. Medicare Benefits Schedule (MBS) and Pharmaceutical Benefits Scheme (PBS) were obtained for all participants who consented, while hospital use data were only collected for participants from Victoria (VIC), Tasmania (TAS), New South Wales (NSW), and the Australian Capital Territory (ACT), due to pragmatic considerations regarding multiple ethics applications. Further details on data elements collected can be found in the supplement (Table S1).
Assessment of disease severity
A number of methods are used to assess disease severity of IPF; however, there is no consensus on a single staging system [12, 13]. Physiologic measurements using pulmonary function test (PFT) parameters such as the forced vital capacity as a percent predicted (FVC%) or diffusion capacity for carbon monoxide (DLco) have been commonly used, as well as composite measures of several physiologic values or demographic features [12, 14,15,16,17]. For our study we used the following three methods, the FVC%, and two composite measures, the Composite Physiological Index (CPI) [15, 18] and the Gender, Age, Physiology (GAP) assessment [14].
Thresholds for the FVC% were based on previous studies [14,15,16,17] with FVC% > 75% considered as mild disease, FVC% between 50 and 75% as moderate disease, and FVC% < 50% as severe disease. For the CPI we used a predetermined formula [15, 18] based on the FVC%, DLco% and the forced expiratory volume as a percent predicted (FEV%). A CPI ≤ 40 is considered as mild disease and CPI > 40 as moderate to severe disease [15]. GAP staging [14] uses the four parameters gender, age, FVC% and the diffusing capacity of the lungs for carbon monoxide percent predicted (DLco%). A GAP index ranging from 0 to 8 is generated from the summation of the scores from each category. The index then allows for classification into the following stages: Stage I (GAP: 0–3), Stage II (GAP: 4–5) and Stage III (GAP: 6–8), with Stage I being the least severe.
In cases where lung function was not available for participants, we categorized participants as “not classified” but still included them in the analysis.
IPF medications
For the purpose of this analysis, we classified medications used in the treatment of IPF based on international guidelines [19]. Pirfenidone and nintedanib were categorized as “antifibrotics”, anti-reflux medications were classified as “Other IPF medications (with limited evidence)” and prednisolone, n-acetylcysteine, warfarin and azathioprine as, “medications not recommended for IPF treatment” [19].
Cost analysis
Costs are analyzed retrospectively for the 12-month period prior to participants’ recruitment (from August 2018 to December 2019). All costs were standardized to Australian dollars ($) 2021, using the Australian Consumer Price Index from the Australian Bureau of Statistics (ABS) [20]. Table 1 provides a summary of the cost categories considered in this analysis.
Outcome variables
This study focused primarily on the following four outcome variables: annualized total direct costs, total direct medical costs, total direct non-medical costs and service utilization for major cost drivers. Costs were further stratified by disease severity, participant characteristics and to illustrate the government costs and out of pocket costs (OOP).
Medication data
Prescription medication costs and quantity were extracted from the PBS data and were classified based on the Australian Medicines Handbook [21]. For the purposes of this analysis, we categorized prescription medications into the following:(1) antifibrotics; (2) other respiratory medications; and (3) medications for comorbidities. Annual prescription costs were summarized for each participant for the three categories. For this category costs were considered from the government and patient perspective, i.e., OOP costs.
Non-prescription medication costs and quantity were extracted from the cost diaries, and these were reported for a period of 4 weeks. Where costs were not recorded for medications, we estimated an average cost, using costs from the four largest pharmacies in Australia [22]. Monthly costs were extrapolated to annual costs with the assumption that the same utilization patterns were maintained. For this category, only OOP costs were considered.
Ambulatory care data
Ambulatory care costs and visits were extracted from MBS data. All services that were not flagged as inpatient services were included in this category and included healthcare professionals and medical and diagnostic tests (Table 1). For this category, costs were considered from the government perspective and patient perspective.
Hospital data
Admitted patient costs and visits were derived from the Australian Refined Diagnosis Related Groups (AR-DRGs) classification system for public hospital funding published by Independent Hospital Pricing Authority (IHPA [23]. Private hospital admission costs were estimated using adjustments recommended by the IHPA [23].
Emergency department attendances were costed based on Urgency Related Groups (URGs) [23].
Sub-acute admissions (rehabilitation, palliative, and geriatric evaluation/management care) were costed based on the Australian National Subacute and Non-acute Patient Classification (AN-SNAP) [23].
Medical equipment
We estimated costs for medical equipment based on participants’ responses in the cost diary. For consumables/accessories where the time frame for use was not provided, an assumed the life span of 1 month was used [24,25,26]. Where no participant costs were incurred, we assumed that the equipment was covered by a government agency and categorized it as a government cost.
Community services
Community service attendances and costs were based on participants’ responses in the cost diary. Where costs were not provided by participants, we assumed that services were supplied based on hourly rates, in accordance with the National Summary of Home Care Prices and applicable government subsidies [27]. OOP costs were assumed to be the hourly costs less the government and other subsidies including Department of Veterans' Affairs (DVA) [27]. Monthly costs were extrapolated to annual costs.
Transportation
Transportation use and costs were based on responses from the cost diary on distance travelled over a 4-week period that was IPF related. Fuel costs per kilometer were based on average fuel consumption patterns for a passenger vehicle and the average national fuel price for 2019 [28, 29]. Other costs included in this category were travel costs to other states for services related to IPF, taxi charges, public transportation, and parking costs. Monthly costs were then extrapolated to annual costs for each participant. For this category, only OOP costs were considered.
Statistical analysis
Statistical analyses were conducted using R Software [30]. Characteristics of participants are presented descriptively as means and standard deviations (SD) for continuous variables or counts and proportions for categorical variables. Two sample t test or Chi-squared tests were used where appropriate to compare (i) participants in the study and persons in the AIPFR who did not consent to the study and (ii) participants with PFTs and participants with incomplete or missing PFTs. A p value less than 0.05 was used as a test for statistical significance.
All costs were summarized as mean costs per person and 95% confidence intervals (95% CI). Summary costs by participants’ characteristics were summarized as mean costs per person (95% CI) and median costs and the interquartile range (IQR). Resource utilization was summarized as the mean (SD) per person and where appropriate as the median per person and IQR.
To estimate total annual population costs, we used a prevalence-based approach [9]. Population estimates were obtained from the ABS [31] and prevalence estimates for IPF were obtained from Cox et al. [32].
Service utilization was summarized as counts and proportions for the 12-month period and means and SDs or 95% CIs where applicable.
Generalized linear models (GLM) with gamma distribution and a log link function were used to model the effect of disease severity and other key sociodemographic and clinical variables on total direct costs [33, 34]. Additionally, we evaluated the effect of these variables on health service utilization, focusing on the major cost drivers, using negative binomial hurdle models [34, 35]. For regression analyses we used the continuous variables for disease severity and BMI. For FVC% and CPI we evaluated the outcome for every 10-unit increase of FVC% and the CPI index and for GAP and BMI every 1-unit increase. We first evaluated univariable models for each variable and then multivariable models based on each disease severity classification.
Results
Participant characteristics
Table 2 provides a summary of participant characteristics. From the AIPFR, the following 288 people were invited to participate: 162 participants consented corresponding to a 56% response rate. Persons who did not participate in the study (n = 126) had more comorbidities and were older than participants (Supplement Table S2). Participants with lung function tests (n = 112) were more likely to be on antifibrotic medications (Table 2).
Eighty-three percent of participants were retired and 80% were aged 65–85 years. The mean age for participants was 73.8 (7.6) years. Most participants were males (61%), Caucasian (90%), resident of major cities (61%) and were based in New South Wales (41%) which is Australia’s most populous state [31]. Approximately 80% had a comorbidity and 60% were on antifibrotic treatment. Sixty percent of participants had mild-moderate disease based on GAP staging and 67% based on FVC% classification. Based on CPI classification, 43% of participants had moderate to severe disease.
Costs
Table 3 provides a summary of costs for the 12-month study period. The mean total direct costs per person with IPF were $31,655 (95% CI $27,723–$35,757). The main cost drivers were antifibrotic medication (61% of total direct costs), hospital admissions (13%) and medications for comorbidities (7%) as illustrated in Fig. 1. The mean costs per person for antifibrotic medication, hospital admissions and medications for comorbidities were $19,340 (95% CI $16,238–$22,809), $4026 (95% CI $2590–$6483) and $2146 (95% CI $1602–$3214), respectively. Other high-cost categories included equipment (4%, $1134) which was driven mainly by oxygen concentrators, specialist costs (3%, $1081) and general practitioners (3%, $1021). Mean OOP costs per person for the period were $2,687 (95% CI $2148–$3478), representing 8% of the total costs. Mean government costs were $28,968 (95% CI $25,238–$33,084) representing 92% of the total mean costs per person. When we extrapolated our cost estimates to the population, prevalence-based total annual direct costs for IPF in Australia were $299 million (95% CI $262 million–$338 million), with government costs and OOP costs being $274 million (95% CI $239 million–$313 million) and $25.4 million ($20.3 million–$32.9 million), respectively.
A closer evaluation of costs based on participant characteristics (Table 4) demonstrated higher mean costs were incurred by persons who were 75–85 years old, persons in outer regional or remote areas and persons with comorbidities had higher costs than those without. In general, there was an increase in mean total direct costs per person with increasing disease severity when evaluated using GAP staging and the CPI index, but this pattern was not seen when disease severity was evaluated using the FVC%. For GAP staging, costs were $28,248 ($21,759–$34,737), $35,563 ($28,043–$43,084) and $39,198 ($19,308–$59,088) for stage 1, 2 and 3, respectively. For the CPI classification, costs were $25,335 ($17,823–$32,847) and $36,828 ($30,750–$42,906) for mild disease and moderate to severe disease, respectively. For the FVC% classification costs were highest for moderate disease, $34,596 ($23,097–$46,095) with costs for mild and severe disease being $31,095 ($25,730–$36,460) and $28,710 ($0–$63,084), respectively. Persons on antifibrotic medication had the highest costs when compared to persons not on antifibrotic medication or on other regimens related to IPF treatment.
Disaggregation of the total direct costs by medical and non-medical components indicated that direct medical costs accounted for 98% of the total direct costs. Mean direct medical costs and mean direct non-medical costs per person were $31,018 ($27,260–$35,283) and $637 ($420–$1101), respectively. Seventy-nine percent of direct non-medical costs were OOP costs, with the majority of these attributable to transportation costs (Table 2).
Regression analyses (Table 5) demonstrated consistent results across the univariable and each of the multivariable models (based on the disease severity classification systems) for comorbidities, disease severity and antifibrotic medication variables. In the multivariable models, our results demonstrated that costs were reduced by a factor of 0.92 of the mean costs for each 10-unit increase in FVC%, for CPI a 10-unit increase corresponded to 1.17-fold increase in mean costs, and for GAP a 1-unit increase corresponded to 1.15-fold increase in mean costs. Participants with comorbidities had a 1.49– to 1.53-fold increase in mean costs compared to persons without comorbidities. Persons on antifibrotics had a 2.66–2.80-fold increase in mean costs when compared to persons not taking antifibrotics. For the FVC% multivariable model, we saw a 1.69-fold increase in costs for the age group 65–75 years, but this was not consistent with the GAP or CPI multivariable models. Likewise, for the GAP model we observed a 1.58-fold increase in mean costs in persons on treatment regimens that are not recommended when compared to those who were not on these regimens.
Predicted total per person costs for a hypothetical male aged between 65 and 75 years old with no comorbidities ranged between $22,815 ($15,367–$33,871) and $32,552 ($18,377–$56,602) for GAP classification, between $25,124 ($17,996–$35,075) and $30,784 ($13,032–$72,719) for FVC classification and between $21,852 ($14,976–$31,884) and $29,499 ($20,744–$41,950) for the CPI classification. Table S4 provides further details on selected hypothetical groupings.
Resource utilization
Table 3 provides a summary of resource utilization for this cohort. Medications for comorbidities accounted for the highest rate of prescriptions (82%), followed by antifibrotic medications (11%). GP visits (59%) and specialist visits (30%) were the most frequent encounters with healthcare professionals. Diagnostic tests were the most used resource in the “medical tests and procedures” category, and non-IPF diagnostics and procedures were more frequently used than IPF diagnostics and procedures. A total of 75 emergency department visits and 106 hospital admissions occurred during the 12-month period with an average of 1 admission/visit per person. On average, 1 piece of home use equipment related to IPF care was acquired, 1 h of community service care was used, and 64 km were travelled for services related to IPF, per person in the cohort per year.
As hospital admissions were of high-cost category, we undertook a more detailed analysis of those. Most admissions were for respiratory diseases (35%), followed by circulatory system diseases (13%) and digestive system diseases (8%). This is in keeping with the comorbidity profile of the participants (Supplement Table S3). Sixty-four percent of all admissions were for comorbidities. The total length of stay (LOS) over the 12-month period for respiratory diseases was 120 days with a mean LOS of 3 days, for circulatory diseases the total number of days was 59 with a mean LOS of 4 days and for digestive system diseases the total was 11 with a mean LOS of 1 day. Nervous system admissions were the fifth most frequent reason for admission but contributed a total of 43 days. On average persons with nervous system disorders were admitted for 7 days, with the longest stay being 28 days. While respiratory disease admissions were the most frequent cause of admission, they did not incur the highest total costs or mean costs per admission. Circulatory system diseases admissions incurred the highest mean costs per admission and total costs. Table 6 provides more details.
A closer look at admissions based on participant characteristics (Table 7) demonstrated that the mean number of admissions were higher in persons older than 85 years, males, persons living in outer regional or remote areas and who were obese. Participants with comorbidities had a higher mean number of admissions than those without comorbidities. Eleven percent of participants with comorbidities had 1 admission and 19% had more than 1 admission. Persons who were not on antifibrotic medication had a higher mean number of admissions and similarly persons on regimens not recommended for treatment of IPF had a higher number of admissions. The CPI classification for disease severity demonstrated that persons with moderate/severe disease had a higher mean number of admissions than persons with mild disease. GAP and FVC% disease classification did not demonstrate this pattern.
Table 8 provides a summary of the hurdle regression analysis for hospital admissions. When the odds ratios for hospitalization were assessed, there were no statistically significant relationships, meaning that the probability of having an admission versus not having an admission was not different between participant sub-groups. When the length of stay and number of admissions was evaluated in those subjects who had an admission, comorbidities had a statistically significant impact. The mean number of admissions increased by a 4.07– to 6.55-fold for persons with comorbidities when compared to those without. Univariable models for GAP, FVC% and CPI index also demonstrated statistically significant count part models. For the GAP disease classification multivariable model, there was a 1.53-fold increase in the mean number of admissions for each 1-unit increase in GAP index. For the FVC% disease classification multivariable model, there was a 0.83-fold decrease in the mean number of admissions for each 10-unit increase in FVC%. For the CPI disease classification multivariable model, there was a 1.43-fold increase in the mean number admissions for each 10-unit increase in CPI index. This significant relationship only persisted in the GAP disease classification multivariable model.
Discussion
Our study is the first to provide a comprehensive analysis of costs and service utilization for Australians with IPF. Given the importance of nationally relevant economic data for decision making related to health financing and resource allocation in public health, this study has addressed important evidence gaps. Our results demonstrated that the average total direct costs per person for a 12-month period were $31,655, 98% of which were direct medical costs. The total prevalence-based costs of IPF in Australia were $299 million. This cost estimate was mainly driven by antifibrotic medication, medications for comorbidities and hospital admissions. Participants had frequent encounters with GPs and specialists and had numerous diagnostic tests and prescriptions related to comorbidities. Disease severity, comorbidities and antifibrotic medication all had an influence on costs. The main cost driver for direct non-medical costs were transportation costs. Ninety-two percent of costs were incurred by the Australian government with OOP costs accounting for 8% of the total direct costs.
We reported total direct costs per person of $31,655 for a 12-month period. When compared to the average per capita health expenditure for Australia for 2019 ($7927, 2021 dollars) [36], our estimate is approximately four times this average. Additionally, when compared to published per capita health expenditure for the age group 65–74 years, our estimated total direct costs for males and females were 2.2 and 1.6 times more than the average per capita health costs for this age group [37]. A comparison with IPF resource costs per person in other countries showed that expenditure which included antifibrotic medication was higher in the United States (USA), Canada, France, Belgium, Germany, Spain and Greece than in Australia [38,39,40,41,42,43,44] (Supplement Table S5). Comparison of the costs reported in these studies to the respective per capita national health expenditure [45] demonstrated that the ratio of costs in other countries was higher than for Australia. The ratios ranged from 5 times the average national health expenditure in Belgium and Canada, to as much as 16-fold higher in the USA [38,39,40,41,42,43,44] (Supplement Table S5). Consideration should, however, be given to varying practice guidelines and payer systems when considering these differences. Further comparison with other disease conditions that are common in this age group in Australia [36, 46,47,48,49] illustrated that the ratio between the costs per person and national average health expenditure was lower than the ratio for IPF for persons with asthma, chronic obstructive pulmonary disease (COPD), cardiovascular disease, osteoarthritis, or type II diabetes. This ratio was, however, higher for lung cancer than for IPF. These were also some of the comorbidities encountered in this cohort, acting as an additive factor for cost, as we have demonstrated higher costs in persons with comorbidities when compared to those without. We also observed that costs increased with increasing disease severity. With GAP and CPI classifications, persons with severe disease incurred the highest cost. It must, however, be noted that persons in this group would not generally qualify for antifibrotic medication (the most expensive category) under current guidelines unless they were started when the disease was less severe and hence persons with severe disease incur significant costs, which we noted were mostly driven by hospital admissions. In view of the aforementioned, it is evident that IPF poses a substantial cost burden more specifically, when compared to other respiratory conditions and other diseases of this age group.
Total direct costs were primarily driven by direct medical costs, with antifibrotic medication, hospital admissions and medications for comorbidities being the main cost drivers. There are few published studies which have comprehensively analysed the cost of IPF since the introduction of antifibrotic therapy and those which have, have primarly focused on costs associated with hospitalisations and the associated resource use. Despite this, our study results display general concordance with the limited published literature which identifies transplants, IPF specific medication, admissions and treatment of comorbidities as the key cost generating categories in the management of IPF [4]. Our study, however, did not include participants who had undergone transplants. Antifibrotic medications are known to be costly, and costs can vary between countries from $2000 to $14,000 per person per month [4, 5] dependent of pricing arrangements and payer systems. These medications have been proven to decrease IPF and respiratory related admissions by as much of 45% [50]. While this may be true, the burden of hospitalizations may also be driven by other factors such, medication interactions and general decline in the overall health [4]. The general decline in health may be due to multiple comorbidities which are frequent in this age group [4], and in our cohort (80%). In our cohort, 65% of all admissions were for comorbidities. The type and number of comorbidities were also contributing factors to costs. Forty-seven percent of participants had cardiovascular disease and 28% also had diabetes, both of which are associated with an increase in hospitalizations and associated costs [49]. Evaluating the influence of comorbidity types and combinations on costs will be a focus of our future research.
Our results demonstrated that participants had a high number of encounters with GPs and specialists as well as having numerous diagnostic tests and prescriptions related to medications for comorbidities. [51]. Polypharmacy is a frequent characteristic of multimorbidity, and this was evident as prescription medications for comorbidities were the most frequently supplied medications, in line with our participant comorbidity profile. Studies have shown that IPF patients have a higher need for health professionals and tests than patients without IPF, due to the high number of IPF clinical issues and comorbidities, adverse events related to antifibrotic medications and polypharmacy and the need for monitoring antifibrotic treatment [4, 52]. The introduction of the multidisciplinary team in the management of IPF also increases encounters with the varying health professionals that constitute the team [4]. Transportation was also a frequently used resource in the non-medical category. This is probably an indication of access to services and more specifically access to respiratory physicians. The number of specialists and waiting time to see a specialist varies by jurisdiction and waiting times can be longer in regional and remote areas when compared to major cities [53]. This may result in persons accessing specialist services further than their immediate surroundings. This is especially true for persons who are eligible for transplants as these services are only available in a few jurisdictions. This has been highlighted in a recent qualitative study in Australia [7].
The Australian health system was established on the premise of universal access, and this was more than evident in this analysis, as 92% of costs were covered by government sources. Not much literature is available on OOP costs for IPF [39], but a comparison with the average OOP cost in 2019 in Australia demonstrated that the average OOP for IPF was 1.6-times higher and represents 3.1% of the average income in Australia [36]. While this may seem small, this was based on the average income and not the average retiree’s income and this may still pose a significant strain on households. Despite universal access, health OOP expenses can still have an influence on patients’ ability to maintain other expenses in the household especially when retired. Studies have shown that up to 25–30% of seniors in Australia experience moderate to severe financial burden as a result of their healthcare expenses and as much as 78% reported hardship in a patient population of persons with COPD in NSW [54, 55]. It should be noted that this study did not include costs for admissions into aged care facilities, as there were no persons admitted at the time of collecting the survey. This may be as a result of persons with more severe disease being less likely to respond to the survey.
Our descriptive statistical analysis demonstrated that disease severity, comorbidities and antifibrotic use had an influence on costs and this was confirmed by the regression analysis. Comorbidities, antifibrotic treatment and increasing disease severity all increased costs. When we looked at resource use and more specifically at hospitalizations which accounted for the highest costs, we saw that comorbidities had the greatest effect. While there was no statistically significant difference between the probability of being admitted whether the participant had a comorbidity or not, when admitted the mean number of admissions was higher in persons with comorbidities than those without. The fact that the odds for admission were not statistically different may be due to improved models of care for persons with chronic complex conditions in Australia including care plans for selfcare and management [56], use of outpatient and GP services. Osteoarthritis was also one of the most frequent comorbidities and this is mostly self-managed or managed in primary care. More investigation into the complex relationships between comorbidity and IPF costs and resource utilization is needed and is the focus of our future work.
This study generated cost estimates for a cohort of Australians living with IPF. There were, however, some limitations. First, our sample size was small but given that IPF is a rare and severe disease, this was expected. Based on the estimated number of persons with IPF in Australia, our sample size represents an 8% margin of error with 95% confidence level [32]. This was also evident with the large confidence intervals on some of the cost estimates especially in subgroups with few participants. Following on from this, the representiveness of the sample may affect the accuracy of estimates. We acknowledge that certain subgroups especially older and more severely affected individuals may disproportionately represented affecting the estimates. While we acknowledge this limitation and the margin of error, we are confident that given the uniqueness of the AIPFR registry that we are including a good representation of the Australian population. The AIPFR is based on national collaboration between respiratory physicians both within major public hospitals and the private service [15]. Notwithstanding this, we are cognizant that a triangulation method to provide concrete evidence is necessary which we have included as part of our future research. Third, while most of the costing was based on administrative data, we also used a retrospective cost diary to obtain some of our category estimates, namely transportation, non-prescription medications and community services which may be subject to recall bias. Another limitation to the analysis was the aggregated format of the administrative data which did not allow a microanalysis of factors such as ICU costs. In addition, our prevalence values used in this analysis were based on estimates derived from IPF diagnosis based on International Classification of Diseases (ICD), and this may be slightly higher than actual diagnosed cases based on international guidelines [32]. Finally, we did not include indirect costs in our analysis as most of our cohort was retired, deaths as we conducted a retrospective analysis 12 months prior to the completion of the survey or seasonal variability Including this would have provided a more comprehensive estimate, and we will look further into assessing this appropriately in our cohort in future studies. Despite these limitations, our estimates will be a useful input for health economic evaluations, especially given the estimation of costs for disease severity.
Conclusion
This cost-of-illness study is the first study to provide comprehensive direct costs related to IPF management in Australia and provides a framework for future health economics studies/evaluation. It also addresses current evidence gaps which are important for reimbursement and policy decisions related to IPF management. Additionally, it provided insight into the major cost drivers which include antifibrotic medication, hospital admissions and medications related to comorbidities. Furthermore, it emphasizes the importance of early diagnosis, early initiation of antifibrotic therapy and the appropriate management of comorbidities in the care of people with IPF as they all have a significant impact on the well-being of persons living with the disease.
Data and code availability
The datasets generated and code used for the analysis are available from the corresponding author upon reasonable request.
References
Richeldi, L., Collard, H.R., Jones, M.G.: Idiopathic pulmonary fibrosis. The Lancet. 389(10082), 1941–1952 (2017)
Akgun, K.M., Crothers, K., Pisani, M.: Epidemiology and management of common pulmonary diseases in older persons. J. Gerontol. A Biol. Sci. Med. Sci. 67(3), 276–291 (2012)
Raghu, G., Amatto, V.C., Behr, J., Stowasser, S.: Comorbidities in idiopathic pulmonary fibrosis patients: a systematic literature review. Eur Respir J. 46(4), 1113–1130 (2015)
Hibbert, C.L., Boes, S., Kinter, E., Vaidya, S.: Identification of key cost generating events for idiopathic pulmonary fibrosis: a systematic review. Lung. 195(1), 1–8 (2017)
Maqhuzu, P.N., Kreuter, M., Bahmer, T., Kahn, N., Claussen, M., Holle, R., et al.: Cost drivers in the pharmacological treatment of interstitial lung disease. Respir. Res. 22(1), 218 (2021)
Cox, I.A., de Graaff, B., Corte, T.J., Glaspole, I., Chambers, D.C., Moodley, Y., et al.: Recent trends in pirfenidone and nintedanib use for idiopathic pulmonary fibrosis in Australia. Aust. Health Rev. 45(6), 718–727 (2021)
Burnett, K., Glaspole, I., Holland, A.E.: Understanding the patient’s experience of care in idiopathic pulmonary fibrosis. Respirology 24(3), 270–277 (2019)
Corte, T., Knight, D., Laurent, G., Holland, A., Chambers, D., Moodley, Y., Walters, E.H., Westall, G., Glaspole, I., Palmer, A.J.: Centre for Research Excellence in Pulmonary Fibrosis (PF-CRE) A comprehensive and integrated clinical research program for PF: transforming the approach to PF in Australia (2015)
Jo, C.: Cost-of-illness studies: concepts, scopes, and methods. Clin. Mol. Hepatol. 20(4), 327–337 (2014)
Moodley, Y., Goh, N., Glaspole, I., Macansh, S., Walters, E.H., Chapman, S., et al.: Australian idiopathic pulmonary fibrosis registry: vital lessons from a national prospective collaborative project. Respirology 19(7), 1088–1091 (2014)
Cox, I.A., de Graaff, B., Ahmed, H., Campbell, J., Otahal, P., Corte, T.J., et al.: The impact of idiopathic pulmonary fibrosis on health state utility values: evidence from Australia. Qual. Life Res. 30(9), 2615–2632 (2021)
Kolb, M., Collard, H.R.: Staging of idiopathic pulmonary fibrosis: past, present and future. Eur. Respir. Rev.: Off. J. Eur. Respir. Soc. 23(132), 220–224 (2014)
Puxeddu, E., Rogliani, P.: Prognostic scoring systems for clinical course and survival in idiopathic pulmonary fibrosis. World J. Respirol. 6(1), 14–23 (2016)
Ley, B., Ryerson, C.J., Vittinghoff, E., Ryu, J.H., Tomassetti, S., Lee, J.S., et al.: A multidimensional index and staging system for idiopathic pulmonary fibrosis. Ann. Intern. Med. 156(10), 684–695 (2012)
Jo, H.E., Glaspole, I., Moodley, Y., Chapman, S., Ellis, S., Goh, N., et al.: Disease progression in idiopathic pulmonary fibrosis with mild physiological impairment: analysis from the Australian IPF registry. BMC Pulm. Med. 18(1), 1–8 (2018)
Erbes, R., Schaberg, T., Loddenkemper, R.: Lung function tests in patients with idiopathic pulmonary fibrosis: are they helpful for predicting outcome? Chest 111(1), 51–57 (1997)
Lopes, A.J., Capone, D., Mogami, R., Lanzillotti, R.S., Melo, P.L., Jansen, J.M.: Severity classification for idiopathic pulmonary fibrosis by using fuzzy logic. Clinics. 66(6), 1015–9 (2011)
Wells, A.U., Desai, S.R., Rubens, M.B., Goh, N.S.L., Cramer, D., Nicholson, A.G., et al.: Idiopathic pulmonary fibrosis: a composite physiologic index derived from disease extent observed by computed tomography. Am. J. Respir. Crit. Care Med. 167(7), 962–969 (2003)
Raghu, G., Rochwerg, B., Zhang, Y., Garcia, C.A.C., Azuma, A., Behr, J., et al.: An official ATS/ERS/JRS/ALAT clinical practice guideline: treatment of idiopathic pulmonary fibrosis. An update of the 2011 clinical practice guideline. Am. J. Respir. Crit. Care Med. 192(2), e3–e19 (2015)
Australian Bureau of Statistics. Consumer price index, Australia Australian Capital Territory, Australia: Australian Bureau of Statistics; 2021. Available from: https://www.abs.gov.au/statistics/economy/price-indexes-and-inflation/consumer-price-index-australia/latest-release#methodology
Australian Medicines Handbook Pty Ltd. Australian Medicines Handbook. [Electronic resource]: AMH Australia: Australian Medicines Handbook Pty Ltd; 2021. Available from: https://login.ezproxy.utas.edu.au/login?url=https://search.ebscohost.com/login.aspx?direct=true&db=cat02831a&AN=UTas.b1703795&site=eds-live
Medicine. 6 Big Australian Pharmacy Groups by Revenue 2019. Available from: https://www.medicine.com.au/the-big-6-australian-pharmacy-groups-by-revenue/
Independent Hospital Pricing Authority. National efficient price determination Australia: Independent Hospital Pricing Authority (2021)
World Health Organization. Technical specifications for oxygen concentrators. (WHO Medical Device Technical Series). Switzerland: World Health Organization (2015)
Hukins, C., Duce, B.: Asset life span in a government funded CPAP device program. J. Clin. Sleep Med.: JCSM: Off. Publ. Am. Acad. Sleep Med. 17(3), 375–380 (2021)
State of Victoria Department of Health and Human Services. Victorian aids and equipment program guidelines. Melbourne, Victoria, Australia: State of Victoria, Department of Health and Human Services (2020)
Department of Health National summary of home care prices. In: Health Do, editor. Canberra, Australia: Department of Health (2021)
Australian Bureau of Statistics. Survey of Motor Vehicle Use, Australia Canberra, Australia: Australian Bureau of Statistics; 2020. Available from: https://www.abs.gov.au/statistics/industry/tourism-and-transport/survey-motor-vehicle-use-australia/12-months-ended-30-june-2020
Australian Institute of Petroleum. AIP Annual Retail Price Data Canberra, Australia: Australian Institute of Petroleum; Available from: https://www.aip.com.au/aip-annual-retail-price-data
R Core Team. R: A language and environment for statistical computing. 3.5.1 ed. Vienna, Austria: R Foundation for Statistical Computing (2019)
Australian Bureau of Statistics. Australian Demographic Statistics Canberra: Australian Bureau of Statistics; 2021. Available from: https://www.abs.gov.au/Population
Cox, I.A., Otahal, P., de Graaff, B., Corte, T.J., Moodley, Y., Zappala, C., Glaspole, I., Hopkins, P., Macansh, S., Walters, E.H., Palmer, A.J.: Incidence, prevalence, and mortality of idiopathic pulmonary fibrosis in Australia. Respirology. 27(3), 209–216 (2021)
Gregori, D., Petrinco, M., Bo, S., Desideri, A., Merletti, F., Pagano, E.: Regression models for analyzing costs and their determinants in health care: an introductory review. Int. J. Qual. Health Care 23(3), 331–341 (2011)
Theobald, E.J., Aikens, M., Eddy, S., Jordt, H.: Beyond linear regression: A reference for analyzing common data types in discipline based education research. Phys. Rev. Phys. Educ. Res. 15(2), 020110 (2019)
Desjardins, C.: Evaluating the performance of two competing models of school suspension under simulation - the zero-inflated negative binomial and the negative binomial hurdle (2015)
Australian Institute of Health and Welfare. Health expenditure Australia 2018–19. Canberra, Australia: Australian Institute of Health and Welfare (2020)
The Productivity Commission. Technical paper 4-Total Health Expenditure. Canberra, Australia: The Productivity Commission (2005)
Corral, M., Chang, E., Broder, M.S., Gokhale, S., Reddy, S.R.: Healthcare use and costs among Medicare enrollees on pirfenidone versus nintedanib for idiopathic pulmonary fibrosis. J. Comp. Eff. Res. 9(13), 933–943 (2020)
Kalluri, M., Lu-Song, J., Younus, S., Nabipoor, M., Richman-Eisenstat, J., Ohinmaa, A., et al.: Health care costs at the end of life for patients with idiopathic pulmonary fibrosis. Evaluation of a pilot multidisciplinary collaborative interstitial lung disease clinic. Ann. Am. Thorac. Soc. 17(6), 706–13 (2020)
Marijic, P., Schwarzkopf, L., Schwettmann, L., Ruhnke, T., Trudzinski, F., Kreuter, M.: Pirfenidone vs nintedanib in patients with idiopathic pulmonary fibrosis: a retrospective cohort study. Respir. Res. 22(1), 268 (2021)
Naoum, P., Skroumpelos, A., Athanasakis, K., Kyriopoulos, J.: Idiopathic pulmonary fibrosis: a cost of illness analysis in Greece. Value Health. 20(9), A643 (2017)
National Institute for Health. OASIS-IPF (Idiopathic Pulmonary Fibrosis) Study: Study results. United States of America: US National Library of Medicine 2021. Available from: https://clinicaltrials.gov/ct2/show/results/NCT03386994?view=results.
Spagnolo, P., Nolin, M., Dalon, F., Belhassen, M., Kirchgassler, K.-U., Chia, J., et al.: Healthcare resource use and related costs in patients receiving nintedanib or pirfenidone for idiopathic pulmonary fibrosis. Eur. Respir. J. 56(Supplement 64), (2020)
Strens, D., Wuyts, W., Bondue, B., Dahlqvist, C., Slabbynk, H., Guiot, J., et al.: Management-related costs of idiopathic pulmonary fibrosis (IPF) in Belgium. Eur. Respir J. 56(Supplement 64), (2020)
The World Bank. Current health expenditure per capita Geneva, Switzerland: The World Bank; 2021. Available from: https://data.worldbank.org/indicator/SH.XPD.CHEX.PC.CD?end=2015&start=2000.
Arthritis Australia. The current and future burden of arthritis: Counting the cost: part 1 healthcare costs. Australia: Arthritis Australia (2016)
Asthma Australia and National Asthma Council Australia. The hidden cost of asthma. Australia: Asthma Australia and National Asthma Council Australia (2015)
Goldsbury, D.E., Weber, M.F., Yap, S., Rankin, N.M., Ngo, P., Veerman, L., et al.: Health services costs for lung cancer care in Australia: estimates from the 45 and up study. PLoS ONE 15(8), e0238018 (2020)
Nutrition Research Australia. Healthcare expenditure and productivity cost savings resulting from increased intake of grain fiber in Australia. Australia: Nutrition Research Australia (2017)
Meyer, K.C., Nathan, S.D.: Idiopathic pulmonary fibrosis: a comprehensive clinical guide, 2nd edn. Springer, New York (2019)
Soley-Bori, M., Ashworth, M., Bisquera, A., Dodhia, H., Lynch, R., Wang, Y., et al.: Impact of multimorbidity on healthcare costs and utilization: a systematic review of the UK literature. Br. J. Gen. Pract. 71(702), e39–e46 (2020)
Diamantopoulos, A., Wright, E., Vlahopoulou, K., Cornic, L., Schoof, N., Maher, T.M.: The burden of illness of idiopathic pulmonary fibrosis: a comprehensive evidence review. Pharmacoeconomics 36(7), 779–807 (2018)
McIntyre, D., Chow, C.K.: Waiting time as an indicator for health services under strain: a narrative review. Inquiry. 57, 46958020910305 (2020)
Essue, B., Kelly, P., Roberts, M., Leeder, S., Jan, S.: We can’t afford my chronic illness! the out-of-pocket burden associated with managing chronic obstructive pulmonary disease in western Sydney, Australia. J. Health Serv. Res. Policy. 16(4), 226–231 (2011)
National Seniors Productive Ageing Centre. The health of senior Australians and the out-of-pocket healthcare costs they face. National Seniors Productive Ageing Centre (2012)
Department of Health. Primary health care advisory group final report: Better outcomes for people with chronic and complex health conditions. Canberra, Australia: Department of Health (2015)
Acknowledgements
Lung Foundation Australia facilitates the Australian IPF Registry with the generous support of unrestricted educational grants from Foundation partners Roche Products, Pty. Limited and Boehringer Ingelheim. The authors would like to acknowledge staff of the Australian IPF Registry and the Registry Coordinators around Australia.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. This study is part of the QUality of LIfE and Costs AssociaTed with Idiopathic Pulmonary Fibrosis Study (QUIET-IPF) a project funded through the NHMRC Centre of Research Excellence in Pulmonary Fibrosis (GNT1116371), and by Foundation partner Boehringer Ingelheim and Program Partners Roche and Galapagos.
Author information
Authors and Affiliations
Contributions
IAC: Conceptualization, Methodology, Formal analysis, Data curation, Data visualization, Validation, Writing original draft, Project administration; BG: Supervision, Conceptualization, Writing- Reviewing and Editing, Project administration; HA and JC, Methodology, Data curation, Writing- Reviewing and Editing; PO: Formal analysis, Validation, Writing- Reviewing and Editing; TJC, YM, NG, PH and SM: Funding, Writing- Reviewing and Editing; EHW: Supervision, Writing- Reviewing and Editing; AJP: Supervision, Conceptualization, Methodology, Validation, Writing- Reviewing and Editing. All authors approved of the final version of the report.
Corresponding author
Ethics declarations
Conflict of interest
TC reports grants and personal fees from Boehringer Ingelheim, grants and personal fees from Roche, grants and personal fees from BMS, personal fees from Promedior, personal fees from Ad Alta, grants from Avalyn Pharma, grants from Biogen, outside the submitted work. All other authors declare that they have no financial/competing interests.
Ethical approval
All study procedures were approved by the University of Tasmania Human Research Ethics Committee (H0016914), Sydney Local Health District, Royal Prince Alfred Zone (Protocol Number X18-0192, Project Number HREC/18/RPAH/269 and SSA/18/RPAH/435), Alfred Health (Site Authorization Letter 45217) and the Hunter New England Local Health District (SSA/19/HNE/23).
Consent to participate
The authors affirm that signed informed consent was obtained from all individual participants included in this study.
Consent for publication
The authors affirm that individual participants provided informed consent for publication of their data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cox, I.A., de Graaff, B., Ahmed, H. et al. The economic burden of idiopathic pulmonary fibrosis in Australia: a cost of illness study. Eur J Health Econ 24, 1121–1139 (2023). https://doi.org/10.1007/s10198-022-01538-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-022-01538-7