Abstract
Background
Managed entry agreements (MEAs) continue to emerge in health technology assessment (HTA)-based decision-making, to address evidentiary uncertainties arising therein. Evidence on the HTA criteria that influence MEAs' uptake remains scarce. This study explores the HTA criteria that determine (i) if an HTA funding decision will be listed with conditions (LWC) other than a MEA, or with a MEA as a condition (LWCMEA), and ii) the MEA type implemented (i.e., financial, outcomes based, or combination).
Methods
HTA reports of all oncology medicines approved since 2009 in Australia, England, Scotland, and Sweden were searched to capture the clinical/economic evidence uncertainties raised in the decision-making process, the Social Value Judgements (SVJs) considered therein and the final coverage decision. Binary and multinomial logit models captured the probability (odds ratio (OR)) of a coverage decision being LWCMEA vs. LWC, and of the MEA being financial, outcomes based, or combination, based on the HTA criteria studied.
Results
23 (12%) LWC and 163 (88%) LWCMEA decisions were identified; 136 (83.4%) comprised financial, 10 (6.2%) outcomes based and 17 (10.4%) combination MEAs. LWCMEA decisions were driven by economic model utilities' uncertainties (7.16 < OR < 26.7, p < .05), and the innovation (8.5 < OR < 11.7, p < .05) SVJ. Outcomes based contracts were influenced by clinical evidence (OR = 69.2, p < .05) and relevance to clinical practice (OR = 26.4, p < .05) uncertainties, and rarity (OR = 46.2, p < .05) and severity (OR = 23.3, p < .05) SVJs. Financial MEAs were influenced by innovation (8.9 < OR < 9.3, p < .05) and societal impact (OR = 17.7, p < .0001) SVJs.
Conclusions
This study provides an empirical framework on the HTA criteria that shape payers' preferences in funding with MEAs, when faced with uncertainty.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background and objectives
The rapid progress of therapeutic innovation and the respective introduction of new, high-cost, therapies might be favourable from the patient’s perspective, but from the payer’s perspective, it poses challenges in managing the market entry and long-term affordability of these therapies [1]. To mitigate these pressures, countries are developing policies to facilitate decision-making about the reimbursement of novel, high-cost pharmaceuticals, such as the cost-effectiveness appraisal of these technologies. In many countries worldwide, these evaluations take the form of health technology assessment (HTA), a process where the clinical and cost-effectiveness of these products is assessed by national competent authorities, to understand if these products demonstrate the “value-for-money” profile required by different healthcare systems to enable coverage [2, 3]. In the HTA process, challenges may arise due to evidentiary uncertainties generated by the immature or early phase evidence submitted by manufactures for appraisal. The uncertainties facing decision-makers have been classified into three broader categories including (i) clinical (e.g., the applicability of study endpoints and treatment population to the actual clinical practice in the country of interest), (ii) financial (e.g., the actual number of doses and treatment duration required in real-world practice and the respective aggregate budget impact) and (iii) utilisation uncertainties (e.g., the appropriate prescribing of the product for the patient population in which it is deemed to be cost-effective) [2, 4]. To address uncertainties arising in the HTA-based decision-making, managed entry agreements (MEAs) between payers and manufacturers are increasingly being employed in many countries as part of the process. Depending on the type of uncertainty to be addressed, literature has classified MEAs in two broader categories, namely outcome- and financial-based agreements depending on whether they aim to mitigate uncertainties related to drug performance or not respectively, while combination agreements with financial and outcome-based aspects have also been observed [2, 5, 6]. Literature has shown that even in cases where countries implemented a MEA for the same medicine-indication pair, often presenting with similar uncertainties, there was still variation in the types of agreements implemented and the respective objective targeted by these agreements [7,8,9]. Descriptive studies have suggested that health system-specific considerations and perceptions of “risk” across settings might play a role in explaining such differences [4, 8, 10]. Furthermore, a descriptive, comparative analysis of MEAs for cancer medicines in different settings, found that cross-country differences may arise chiefly due to payers’ preferences on social value considerations, such as the socioeconomic and Quality of Life (QoL) impact of the treatment appraised, followed by setting-specific requirements on the economic model, and the comparators, costs, and utilities included in the model [11].
Despite the growing utilisation of MEAs, quantitative, empirical research on the HTA factors that have an impact on the uptake of MEAs across settings remains scarce [12, 13]. This has significant implications for the transparency of “best-practice” guidelines on MEA negotiation and implementation processes across and within countries [6, 13]. To address this literature gap, this paper provides a quantitative assessment of the key HTA criteria that have been suggested by previous, descriptive research as potential determinants of MEAs. Ultimately, the objective of this analysis is twofold: first, to identify the relative importance of these criteria in comparison to each other towards shaping decision-making under uncertainty and second, using specifically a quantitative approach, to map the HTA criteria that determine coverage with a MEA or not, and if so, the criteria that determine the type of MEA.
Methods
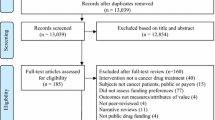
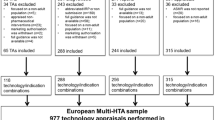
Sample selection
All oncology medicines which obtained regulatory approval by the European Medicines Agency (EMA) in Europe and by the Therapeutic Goods Administration (TGA) in Australia between 1st January 2009 and 15th June 2018 (at the medicine-indication pair level) were studied in Australia (AUS), England (ENG), Scotland (SCOT) and Sweden (SE). Oncology was selected as the study therapeutic class because it has been documented to be the therapeutic class with the largest proportion of implemented MEAs and the therapeutic class where MEAs continue to be increasingly implemented [2]. Study countries were selected because they all implement MEAs, they all have long-established HTA policies and processes to guide their coverage decisions, they have both a publicly available list of MEAs and HTA reports (or publicly available documents where MEAs and other HTA criteria can be inferred from, such as the Public Summary Documents in Australia) and they use similar approaches in their pricing and reimbursement decision-making process (i.e., clinical and cost-effectiveness approach), allowing for comparability across agencies [14].
Data collection
The conceptual framework underpinning data collection operates under the overarching hypothesis that HTA coverage decisions (whether positive, negative or restricted) are primarily shaped by the HTA process itself, including the evidence appraised therein (whether clinical, economic or otherwise), the way this evidence is interpreted/assessed by the decision-makers, and the broader socioeconomic and political context in which the decision-making takes place [11, 14, 15].
Essentially, this framework divides the HTA process and relevant variables of interest in four “buckets” where it is hypothesised that a combination of variables within “buckets” (A), (B) and (C), determine the observed outcome in “bucket” (D) as follows: (A) clinical and economic evidence appraised (e.g., trial characteristics, comparators, Incremental Cost Effectiveness Ratio (ICER) and economic model specifications), (B) interpretation/assessment of this evidence (i.e., clinical and economic evidence related uncertainties raised), (C) societal and system-specific context in which HTA-based decision-making operates (i.e., dimensions of value that a technology adds in the society/setting of interest, such as the unmet need it targets in terms of therapeutic treatment availability, the societal benefit it offers in terms of improved patient QoL, functional ability outcomes, all referred to as Social Value Judgements (SVJs)) and system-specific processes for decision-making (e.g., the use of a single or multiple technology appraisal in England), and (D) coverage decision outcome categorised as: (i) L = List (i.e., positive coverage decision), (ii) LWC = List with one or more conditions which are not classified as MEAs (e.g., dosing restrictions, clinical restrictions relating to treatment eligible sub-population, etc.), (iii) LWCMEA = List with one or more conditions including at least one restriction classified as MEA and iv) DNL = Do not list (i.e., negative coverage decision).
Data on the above “buckets”, per medicine-indication pair in all study countries were extracted from publicly available HTA appraisals published in the respective HTA bodies’ websites, namely PBAC (AUS), NICE (ENG), TLV (SE) and SMC (SCOT). A database stratified by HTA agency was built to describe and classify MEAs across the respective HTA bodies and facilitate data analysis.
Data analysis
Restricted HTA outcomes were coded as a binary variable (i.e., LWC vs. LWCMEA), while the type of MEA was coded as a multinomial variable (i.e., financial (“F”), outcomes (“O”) based or combination (“C”)), based on taxonomies that have been described in the literature [2, 6, 9], with discounts explicitly considered as financial MEAs in this analysis. Finally, assuming that all categories of uncertainties and SVJs were applicable to all drug-indication pairs studied, these were treated and coded as binary variables based on whether they have been raised and considered (or not), respectively, in the HTA-based decision-making process [11]. More specifically, the mention/raise of an uncertainty or SVJ—regardless of its weight/impact on the decision-making process—has been classified as “raised” or “considered”, while in cases where there is no mention of a specific uncertainty or SVJ this was classified as “not raised” or “not considered”, respectively, for each drug-indication pair.
For the purposes of this analysis, a panel data design was not feasible as the study sample comprised one decision per medicine-indication pair per country in a particular year as opposed to annual decisions; similarly, since the response variables are categorical, they could not be modelled as a linear combination of explanatory variables either [15]. Therefore, the associations studied were described as probabilities, estimated by means of a binary and a multinomial logit model. For the first part of the analysis, binary logistic regression was used to estimate the probability of a technology receiving restricted coverage with at least one restriction in the form of a MEA (as opposed to one or more restrictions without a MEA) based on a set of HTA explanatory variables, hypothesised to influence HTA-based decision-making [14, 16]. Additionally, as a robustness check, Pearson’s Chi-squared tests were performed to identify which HTA criteria determine statistically significant differences between LWC and LWCMEA coverage decisions for each study country. Finally, for the second part of the analysis, multinomial logistic regression was used to model the probability of an implemented MEA taking one of the three outcomes “F”, “O” or “C” given a set of HTA criteria/ explanatory variables associated with the medicine-indication pair in question.
Results
235 coverage decisions were studied, of which 88% (n = 207) were favourable (with or without restrictions) and 12% (n = 28) non-favourable across all countries. The majority of favourable coverage decisions were LWCMEA (78.7%, n = 163), 11.1% (n = 23) were LWC and 10.2% (n = 21) were L. In England, 93% (n = 54) of MEAs were financial, 96% (n = 49) in Scotland, 76.3% (n = 29) in Australia and 27% (n = 4) in Sweden. Outcome-based schemes were mostly implemented in Sweden (47%, n = 7) and combination schemes primarily used in Australia (21%, n = 8) (Table 1).
LWC vs. LWCMEA coverage decision
Of the restricted coverage decisions studied (n = 186), 88% (n = 163) were LWCMEA and 12% (n = 23) were LWC. A number of binary logit models were performed to ascertain the effects of different HTA criteria on the likelihood of receiving a LWCMEA as opposed to a LWC coverage decision. The statistically significant models with the best predictability rate are presented below (Table 2). Values highlighted in bold correspond to the effect size/ likelihood (i.e., OR) and the respective p-value of the HTA criteria that were found to be of statistical significance within the different models.
The first model (χ2 = 47.7, p < 0.0001) explained 43% (Nagelkerke R2) of the variance in restricted coverage decisions and correctly classified 92% of cases. Medicine-indication pairs with utility and cost-effectiveness related uncertainties were approximately 27 (OR=26.731, p<0.05) and 4 (OR=3.926, p<0.05) times, respectively, more likely to receive a LWCMEA instead of a LWC coverage decision. The SVJs of innovation and rarity were associated with an increased (OR=8.504, p<0.05) and decreased (OR=.147, p<0.05) likelihood of a LWCMEA (as opposed to LWC) coverage decision, respectively.
The second model (χ2 = 51.3, p < 0.0001) explained 46% (Nagelkerke R2) of the variance in restricted outcomes and correctly classified 91% of cases. Medicine-indication pairs with utility and cost-effectiveness related uncertainties were approximately 21 (OR=20.97, p<0.05) and 4.5 (OR=4.361, p< 0.05) times respectively, more likely to receive a LWCMEA instead of a LWC coverage decision. The SVJs of innovation and rarity were associated with an increased (OR=10.632, p<0.05) and decreased (OR=.165, p<0.05) likelihood of a LWCMEA (as opposed to LWC) coverage decision, respectively.
The third model (χ2 = 18.25 , p < 0.0001) explained 30% (Nagelkerke R2) of the variance in restricted coverage decisions and correctly classified 88% of cases. Medicine-indication pairs with utility and economic comparator related uncertainties were approximately 7 (OR=7.169, p<0.01) and 4 (OR=4.147, p<0.05) times, respectively, more likely to receive a LWCMEA instead of a LWC coverage decision. The SVJ of innovation was associated with an increased (OR=11.727, p<0.01) likelihood of a LWCMEA (as opposed to LWC) coverage decision.
Finally, the fourth model (χ2 = 19.45, p < 0.001) explained 19% (Nagelkerke R2) of the variance in restricted outcomes and correctly classified 87% of cases. Medicine-indication pairs with cost-effectiveness related uncertainties were approximately 3 (OR=3.24, p<0.05) times more likely to be classified as LWCMEA instead of LWC. The SVJs of special considerations and rarity were associated with an increased (OR=3.014, p<0.05) and decreased (OR=.254, p<0.05) likelihood of a LWCMEA (as opposed to LWC) coverage decision, respectively.
Country-specific outcomes
Pearson’s chi-squared tests were also performed to identify any HTA criteria that determine statistically significant differences between LWC and LWCMEA coverage decisions for each study country. Cost-effectiveness uncertainties determined statistically significant differences between the LWC and LWCMEA groups for England (χ2 = 8.98, p = 0.003), Scotland (χ2 = 3.97, p = 0.046) and Australia (χ2 = 5.02, p = 0.025). Additionally, uncertainties around the economic model used and the utilities included in the model highlighted statistically significant differences between LWC and LWCMEA coverage outcomes in England (χ2 = 5.65, p = 0.017) and Australia (χ2 = 3.10, p = 0.028), respectively. Finally, uncertainties around clinical evidence and clinical benefit, and the SVJ of innovation, underscored statistically significant differences between LWC and LWCMEA groups for Scotland (χ2 = 3.68, p = 0.04), England (χ2 = 4.98, p = 0.026) and Australia (χ2 = 3.10, p = 0.028), respectively (Online resource 1).
Type of MEA
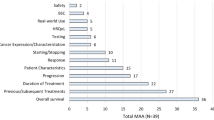
163 MEAs were identified, of which 83.4% (n = 136) were “F”, 6.2% (n = 10) were “O” and 10.4% (n = 17) were “C”. A number of multinomial logit models were performed to identify the sets of HTA criteria, including clinical/economic uncertainties and SVJs, that best predicted the likelihood of a MEA in place for the study medicine-indication pairs being “F”, “O” or “C” (Table 3, Fig. 1). Values highlighted in bold correspond to the effect size/likelihood (i.e., OR) and the respective p-value of the HTA criteria that were found to be of statistical significance within the different models.
Analytical framework on the HTA criteria driving restricted coverage decisions with a MEA (LWCMEA) and the respective type of MEA. HTA: Health Technology Assessment, LWC: List with conditions, LWCMEA: List with conditions, including a MEA, MEA: Managed Entry Agreement, SVJs: Social Value Judgements. The categories of the HTA criteria included in this analysis and subsequently used in the above framework are based on previously published relevant research and all respective definitions are described in detail therein [11]. Source: The author; the framework is fully conceptualised by the author, based on background from relevant literature [2, 11, 14]
The first model (χ2 = 38.61, p < 0.0001) explained 42% (Nagelkerke R2) of the variance in MEA types. Medicine-indication pairs with uncertainties raised around relevance to clinical practice (OR=.072, p< 0.05 and OR=.056, p<0.05) and social value considerations around rarity (OR=.073, p<0.05 and OR=.04, p<0.05) were more likely to be funded with an “O”, as opposed to a “F” and a “C” agreement respectively. On the contrary, the social value consideration of innovation was as associated with an approximately 9.5 (OR=9.346, p<0.05) times higher likelihood of a “F” as opposed to an “O” agreement.
The second model (χ2 = 41.79, p < 0.0001) explained 45% (Nagelkerke R2) of the variance in MEA types. Medicine-indication pairs with uncertainties raised around clinical evidence (OR=.066, p<0.05) and relevance to clinical practice (OR=.084, p<0.05), and social value considerations around rarity (OR=.061, p<.05) were more likely to be funded under an “O” as opposed to a “F” agreement. Similarly, medicine-indication pairs with social value considerations around rarity were more likely (OR=.034, p<0.05) to lead to an “O” as opposed to a “C” agreement. On the contrary, medicine-indication pairs with social value considerations around innovation and impact on society were associated with an approximately 9 (OR=8.999, p<0.05) and 18 (OR=17.732, p<0.0001) times higher likelihood of coverage with a “F” as opposed to an “O” agreement.
The third model (χ2 = 47.94, p < 0.0001) explained 50% (Nagelkerke R2) of the variance in MEA types. Medicine-indication pairs with uncertainties raised around clinical evidence (OR=69.221, p<0.05) and relevance to clinical practice (OR=26.4, p< 0.05), and social value considerations around rarity (OR=46.207, p<0.05) and severity (OR=23.349, p<0.05), had a higher likelihood of coverage with an “O” instead of a “F” agreement. Additionally, medicine-indication pairs with social value considerations around innovation (OR=.038, p<0.05) and special considerations (OR=.148, p<0.05) were associated with a higher likelihood of coverage with a “F” instead of a “C” agreement.
Discussion and policy implications
This paper explored the sets of HTA criteria, including clinical/economic uncertainties and SVJs, that might contribute to a higher likelihood of restricted HTA recommendations including a MEA as part of the restriction or not, and subsequently identified the HTA-relevant criteria that determine the respective type of a MEA in place (Fig. 1). This is the first study to date to model the HTA criteria that determine both the utilisation and the typology of MEAs in oncology therapies across countries.
Coverage with a MEA was predominantly driven by uncertainties around the utilities of the economic model, and the SVJ of innovation. Outcome-based contracts were primarily influenced by uncertainties on the clinical evidence and relevance to clinical practice, followed by the rarity and severity of the condition. Financial MEAs were influenced by the SVJs of innovation and societal impact of the technology in question. Similar findings arise from the limited and largely descriptive evidence available in the relevant literature. A recent review of outcome-based MEAs in the OECD countries concluded that these may indeed be more common for products with orphan indications, while a case study presented therein concluded that outcome-based schemes in England mostly tried to address uncertainty around the magnitude of long-term clinical benefit, and concerns around the duration of therapy in routine clinical practice [17]. It has also been suggested that outcome-based contracts typically aim to address uncertainties around efficacy or effectiveness in the general population, long-term clinical evidence on clinically significant endpoints (i.e., clinical rather than surrogate markers), as well as safety, and numbers likely to be treated in real-world practice [6]. Finally, using a theoretical model, Antonanzas et al. (2011) analysed situations in which payers will prefer a MEA over non-MEA and concluded that payers’ decisions will depend on monitoring costs, marginal production costs, and the utility patients will derive from treatment [18].
Beyond its empirical study design, another strength of this analysis is the holistic approach considered in the HTA criteria driving MEAs, accounting for the interconnected impact of both uncertainties and SVJs on the final HTA/MEA outcomes, as opposed to the existing literature that has primarily studied the impact of uncertainties. This is important because the emphasis placed on HTA criteria differs between HTA stakeholders across or even within countries; some countries focus on disease severity and drug efficacy, others concentrate on cost-effectiveness, whereas in some countries, payers and HTA stakeholder experts have different preferences on the HTA process and hence, divergent views on which criteria are the most significant within their systems [12]. Specifically, for MEAs, it arises that the requirement for an agreement and the type of agreement preferred by payers, is subject to the disease area and other setting and medicine specific, value considerations [19]. Furthermore, despite significant efforts to create good practice guidelines on the design, implementation, and evaluation of MEAs [6, 20,21,22,23,24], there are still gaps in understanding the conditions that lead to acceptance of proposed MEAs from the payers’ perspective. For example, in England, rejections of manufacturer proposed agreements (i.e., Patient Access Schemes (PAS)) are still observed, highlighting that despite existing guidelines on the submission of PAS, we still lack an understanding of the considerations that render a MEA successful from the point that a company submits a PAS proposal and until this is accepted by NICE [24, 25]. On that front, the findings presented here can enhance transparency in existing guidelines by promoting a shared understanding on the aspects that determine value in MEA negotiations from the payer’s’ perspective. This can guide both manufacturers—to tailor agreement proposals such that they align with the value perceptions of different payers, and payers—to establish more streamlined processes in decision-making under uncertainty.
Limitations
Despite the empirical contribution of this study in the field of MEA research, the results presented herein should be interpreted with caution due to certain methodological discrepancies that possibly undermine the robustness of the study.
First, country-specific policies, purchasing framework and context in which pricing and reimbursement decision-making operates have not been incorporated in the analysis per se. It is believed that their potential confounding effect has been captured through criteria around HTA system-specific considerations such as SVJs. Of course, even though the SVJ classification used in this analysis is largely applicable to all important SVJs considered across countries [11, 14], SVJs still remain highly subjective and dependent on the setting-specific context in which they are considered. Therefore, the SVJ variables included in this analysis might not be entirely representative of all the system-specific considerations that are of “weight” in HTA-based decision-making across the study countries. In addition, reference in the literature has been made on the impact of the overall country-specific healthcare and welfare characteristics on HTA-based decision-making, such as healthcare spending per capita, societal willingness-to-pay and the structure of the healthcare system [26]. As such, to enhance accuracy of the results, these factors should be explicitly included in future studies modelling the uptake of MEAs.
Second, based on the methodology followed in this analysis, whether an uncertainty has been resolved or not reflects the impact of the implemented MEA, while the mention/raise of an uncertainty during the appraisal (whether resolved or not following the proposed MEA) reflects a potential determinant/reason behind the implementation of a MEA as a funding modality. On that front, this specific analysis does not differentiate between resolved/unresolved uncertainties; it aims to capture all the uncertainties raised (as per the HTA reports/public summary documents) to understand which of these had a greater impact in determining LWCMEA coverage decisions. However, it is of critical importance to conduct further analyses to capture the uncertainties that remain following the proposed MEA, as an evaluation of its impact.
Finally, the limited sample size studied hinders the overall power, sensitivity and specificity of the models. Future replication of these models would benefit from a larger study sample, possibly by including coverage decisions of medicines in other therapeutic areas too, although caution should be exercised to account for potential comparability issues arising from differences in the value that different SVJs reflect for payers in different disease areas. Overall, due to setting-specific nuances in HTA-based and reimbursement decision-making, the criteria and their relative weight in the decision-making process, as identified in this analysis, are not necessarily generalisable across settings and should be interpreted on an individual basis and adapted to the respective setting-specific context in question.
Conclusions
The growing interest in MEAs and their increased implementation across countries globally, necessitates an enhanced transparency on the aspects that determine value in MEA negotiations. On that front, the findings of this study provide a better understanding on the decision-making criteria that shape payers’ preferences in coverage with a MEA or not. Empirical research on the HTA criteria driving MEAs is key to encourage a transparent, cross-country learning on how MEAs can be tailored to align with payers’ perceptions on “value” and ultimately, promote more efficient MEA negotiations and increased opportunities for coverage through MEAs. There are still barriers to overcome for MEAs to be implemented more widely and efficiently, such as their increased administrative burden, the absence of standardised processes to evaluate their outcomes and the confidentiality around the final prices and discounts negotiated under these agreements.
Data availability
The dataset generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
European Commission (EC) (2018). Innovative payment models for high-cost innovative medicines report of the expert panel on effective ways of investing in health (EXPH). https://ec.europa.eu/health/expert_panel/sites/expertpanel/files/docsdir/opinion_innovative_medicines_en.pdf (Accessed March 15, 2018) (2018)
Ferrario A, Kanavos P. Managed entry agreements for pharmaceuticals: the E uropean experience. EMiNet, Brussels, Belgium (2013). http://eprints.lse.ac.uk/50513/1/_Libfile_repository_Content_Ferrario%2C%20A_Ferrario_Managed_%20entry_%20agreements_2013_Ferrario_Managed_%20entry_%20agreements_2013.pdf
Husereau D, Cameron C. December 2011. Value-based pricing of pharmaceuticals in Canada: opportunities to expand the role of health technology assessment? CHSRF series of reports on cost drivers and health system efficiency: paper 5. http://www.cfhi-fcass.ca/Libraries/Commissioned_Research_Reports/Husereau-Dec2011-EN.sflb.ashx
WHO (2015). ‘Access to new medicines in Europe: technical review of policy initiatives and opportunities for research’. 2015, WHO: Copenhagen. http://www.euro.who.int/en/health-topics/Health-systems/medicines/publications2/2015/access-to-new-medicines-in-europe-technical-review-of-policy-initiatives-and-opportunities-for-collaboration-and-research
KCE. Gerkens S, Neyt M, San Miguel L, Vinck I, Thiry N, Cleemput I. How to improve the Belgian process for Managed Entry Agreements? An analysis of the Belgian and international experience. Health Services Research (HSR) Brussels: Belgian Health Care Knowledge Centre (KCE). KCE Reports 288. D/2017/10.273/41. (2017) https://kce.fgov.be/sites/default/files/atoms/files/KCE_288_Improve_Belgian_process_managed_entry_agreements_Report.pdf
Garrison, L.P., Jr., Towse, A., Briggs, A., De, P.G., Grueger, J., Mohr, P.E., et al.: Performance-based risk-sharing arrangements-good practices for design, implementation, and evaluation: report of the ISPOR good practices for performance-based risk-sharing arrangements task force. Value Health 16, 703–719 (2013)
Pauwels, K., Huys, I., Vogler, S., Casteels, M., Simoens, S.: Managed entry agreements for oncology drugs: lessons from the European experience to inform the future. Front. Pharmacol. 8, 171 (2017)
Ferrario, A., Kanavos, P.: Dealing with uncertainty and high prices of new medicines: a comparative analysis of the use of managed entry agreements in Belgium, England, the Netherlands and Sweden. Soc Sci Med. 124, 39–47 (2015)
Carlson, J.J., Sullivan, S.D., Garrison, L.P., Neumann, P.J., Veenstra, D.L.: Linking payment to health outcomes: a taxonomy and examination of performance-based reimbursement schemes between healthcare payers and manufacturers. Health Policy 96(3), 179–190 (2010)
Morel, T., Arickx, F., Befrits, G., Siviero, P., van der Meijden, C., Xoxi, E., Simoens, S.: Reconciling uncertainty of costs and outcomes with the need for access to orphan medicinal products: a comparative study of managed entry agreements across seven European countries. Orphanet J. Rare Dis. 8, 198 (2013)
Efthymiadou, O., Kanavos, P.: Determinants of managed entry agreements in the context of health technology assessment: a comparative analysis of oncology therapies in four countries. Int J Technol Assess Health Care. 29(37), e31 (2021)
Akehurst, R.L., Abadie, E., Renaudin, N., Sarkozy, F.: Variation in health technology assessment and reimbursement processes in Europe. Value Health. 20(1), 67–76 (2017)
Antonanzas, F., Juárez-Castelló, C., Lorente, R., et al.: The use of risk-sharing contracts in healthcare: theoretical and empirical assessments. Pharmacoeconomics 37, 1469–1483 (2019)
Nicod, E., Kanavos, P.: Developing an evidence-based methodological framework to systematically compare HTA coverage decisions a mixed methods study. Health Policy 120(1), 35–45 (2016)
Maynou-Pujolras, L., Cairns, J.: Why do some countries approve a cancer drug and others don’t? J. Cancer Policy 4, 21–25 (2015)
Dakin, H., Devlin, N., Feng, Y., Rice, N., O’Neill, P., Parkin, D.: The influence of cost-effectiveness and other factors on nice decisions. Health Econ. 24(10), 1256–1271 (2015). https://doi.org/10.1002/hec.3086. (Epub 2014 Sep 23 PMID: 25251336)
Wenzl, M and Chapman S. (2019), "Performance-based managed entry agreements for new medicines in OECD countries and EU member states: How they work and possible improvements going forward", OECD Health Working Papers, No. 115, OECD Publishing, Paris. https://www.oecd.org/health/health-systems/HWP-115-MEAs.pdf
Antonanzas, F., Juarez-Castello, C., Rodriguez-Ibeas, R.: Should health authorities offer risk-sharing contracts to pharmaceutical firms? A theoretical approach. Health Econ. Policy Law 6(3), 391–403 (2011)
Dunlop, W.C.N., Staufer, A., Levy, P., Edwards, G.J.: Innovative pharmaceutical pricing agreements in five European markets: a survey of stakeholder attitudes and experience. Health Policy 122(5), 528–532 (2018)
WHO (2018). New report from TLV highlights importance of managed entry agreements. 8 January, 2018. WHO Regional Office for Europe. http://www.euro.who.int/en/countries/sweden/news/news/2018/01/new-report-from-tlv-highlights-importance-of-managed-entry-agreements
NICE. (2018). Process and methods. Patient access schemes, commercial access agreements and flexible pricing. https://www.nice.org.uk/process/pmg19/chapter/patient-access-schemes-commercial-access-agreements-and-flexible-pricing
SMC (2019). NHSScotland Patient Access Scheme (PAS) Guidance V8. https://www.scottishmedicines.org.uk/media/4434/nhsscotland-patient-access-scheme-pas-guidance-v80-final.pdf
PBS (2017). Guidelines for deeds of agreement for the pharmaceutical benefits Scheme (Version 1.4). http://www.pbs.gov.au/info/industry/listing/elements/deeds-agreement
DoH. Hints and tips for companies considering a patient access scheme (PAS) proposal in England. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/217037/PAS-Good-Practice-Guidance.pdf
Pharmaforum Patient Access Schemes: a look behind the scenes. https://pharmaphorum.com/views-and-analysis/patient-access-schemes-a-look-behind-the-scenes/ (2015).
Cerri, K.H., Knapp, M., Fernández, J.L.: Decision making by nice: examining the influences of evidence, process and context. Health Econ Policy Law. 9(2), 119–141 (2014)
Acknowledgements
The author is grateful to the following experts for their invaluable collaboration in the data collection and validation process: Anna-Maria Fontrier, Mackenzie Mills and Erica Visintin. I am also thankful to Prof. Panos Kanavos for his support and supervision in conducting this study.
Funding
The author received no specific funding for this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author received no specific funding for this work and declares no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Efthymiadou, O. Health technology assessment criteria as drivers of coverage with managed entry agreements: a case study of cancer medicines in four countries. Eur J Health Econ 24, 1023–1031 (2023). https://doi.org/10.1007/s10198-022-01526-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-022-01526-x