Abstract
Objective
To estimate the impact of glycaemic control and time since diabetes diagnosis on care costs incurred by people with type 2 diabetes mellitus (T2DM).
Research design and methods
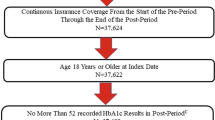
Random-effects linear regression models were run to test the impact of average glucose control (HbA1c) and time since diabetes diagnosis on total care spending in people with T2DM, adjusting for year of onset and other covariates. Two datasets were linked, Vektis (healthcare costs reimbursed by the Dutch mandatory health insurance) and Zodiac (clinical and sociodemographic data). The sample includes 22,612 observations, grouped in 5653 individuals from the Northern part of the Netherlands, covering 4 years (2008–2011).
Results
A 1% point increase in HbA1c is associated with a 2.2% higher total care costs. However, when treatment modality is included, the results are modified. A 1% point increase (11 mol/mol) in HbA1c is significantly associated with 3.4% higher total care costs for individuals without glucose-lowering treatment. Being treated with insulin is significantly associated with an increase in costs of 30–38% for every additional percentage point of HbA1c, depending on the covariates included. Without controlling for year of onset, an additional year of diabetes duration relates to 2.6% higher care costs, while this is 4.9% controlling for year of onset. The effect of HbA1c and diabetes duration differs between types of costs.
Conclusion
HbA1c, insulin treatment and diabetes duration are the main drivers of increasing care costs. The results signal the relevance of controlling for HbA1c together with treatment modality, diabetes duration and year of diagnosis effects.



Similar content being viewed by others
Notes
Individuals were classified as having an excellent glucose control if HbA1c level was below or equal to 7% in, at least, 80% of the available measurements during the follow-up period.
The privacy of all patients was assured using a trusted third party (ZorgTTP) to combine the data, while encrypting the personal identity numbers, thus creating a database with detailed information, which could not be traced to a known individual. The researchers performed all analyses at VEKTIS, on a fully anonymous dataset.
Costs that were not included were uninsured care (i.e. informal care), as well as care from any additional insurance (treatments not or only partly covered by the mandatory package; for instance, dental care for people aged 18 years old and above, alternative medical treatments (homoeopathy), or hearing aids).
Diabetes non-related conditions refer to cancer, alcohol abuse, paralysis, chronic pulmonary disease, hypothyroidism, liver disease, peptic ulcer, rheumatoid arthritis, anaemia, psychosis and depression.
Congestive heart failure, acute myocardial infarction, peripheral vascular disease, uncomplicated hypertension, complicated hypertension, stroke, any other cerebrovascular accident, dementia, retinopathy, neuropathy, renal failure, weight loss, obesity were considered the diabetes-related comorbidities.
We also performed the same regressions including Mundlak terms [28] to relax the assumption that observed time-varying variables are uncorrelated with the unobserved variables by adding individual-means of independent variables that do vary over time within individuals. However, the Mundlak terms included were not significant, and the coefficients were quite similar to the ones obtained in the Random-effects linear regression models. Hence, results with Mundlak terms can be found in Table A2 in Online Appendix.
Table A3, Online Appendix, reports the summary statistics for the original sample, before applying the sample selection criteria. There are no big differences when compared to the final sample.
According to the American Diabetes Association guidelines [23], HbA1c levels are at target level if they are equal or below 6.5%. Hence, three categories of HbA1c levels are set according to HbA1c levels: (1) HbA1c ≤ 6.5%; (2) 6.5% < HbA1c ≤ 7.5%; and (3) HbA1c > 7.5%, which indicates uncontrolled diabetes.
A coefficient will be considered statistically significant if it is significant, at least, at 95% confidence level (p value = 0.05).
The average marginal effect and p value of age (and diabetes duration) were calculated using the command lincom from Stata 14.0, using the regression coefficients for age and age squared (diabetes duration and its square) as well as the mean age (diabetes duration) for the overall sample. For example, the average marginal effect of an additional year of age is calculated as follows: coefficient of age + 2 × coefficient of age2 × (mean age) = 0.0174262 + 2 × 0.0000266 × 68.38 = 0.0210593 (z value = 21.68, p value = 0.000).
The coefficient and p value of variables part of interactions in the regression model were obtained using the command lincom from Stata 14.0. For example, the coefficient of insulin is calculated as follows: coefficient of insulin alone + coefficient of the interaction HbA1c # insulin × mean HbA1c = 0.658 − 0.0498 × 6.77. Once we obtained this coefficient and given the logarithmic form of our regression model, we calculated the insulin coefficient as follows: \((e^{\text{coef}} - 1) \times 100 = (e^{0.3208} - 1) \times 100 = 37.83.\). The second part of the calculation was followed for every dummy variable included in the main analysis (treatment modalities and diabetes onset cohorts) and in the sensitivity analysis (Elixhauser comorbidities).
It has already been found in the literature that the incremental costs in the first years after diabetes diagnosis decrease [31] and then start increasing again. In our data, GP costs start to rise after 37 years since diabetes diagnosis.
References
OECD/EU: Health at a Glance: Europe 2016—State of Health in the EU cycle. OECD Publishing, Paris (2016)
NCD Risk Factor Collaboration: Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet 387, 1513–1530 (2016)
Zhang, P., Zhang, X., Brown, J., Vistisen, D., Sicree, R., Shaw, J., Nichols, G.: Global healthcare expenditure on diabetes for 2010 and 2030. Diabetes Res. Clin. Pract. 87, 293–301 (2010)
Liebl, A., Khunti, K., Orozco-Beltran, D., Yale, J.F.: Health economic evaluation of type 2 diabetes mellitus: a clinical practice focused review. Clin. Med. Insights Endocrinol. Diabetes 8, 13–19 (2015)
Li, R., Zhang, P., Barker, L.E., Chowdhury, F.M., Zhang, X.: Cost-effectiveness of interventions to prevent and control diabetes mellitus; a systematic review. Diabetes Care 33, 1872–1894 (2010)
Herman, W.H., Hoerger, T.J., Brandle, M., Hicks, K., Sorensen, S., Zhang, P., Hamman, R.F., Ackermann, R.T., Engelgau, M.M., Ratner, R.E., For the Diabetes Prevention Program Research Group: The cost-effectiveness of lifestyle modification or metformin in preventing type 2 diabetes in adults with impaired glucose tolerance. Ann. Intern. Med. 142, 323–332 (2005)
Clarke, P., Gray, A., Adler, A., Stevens, R., Raikou, M., Cull, C., Stratton, I., Holman, R., On behalf of the UKPDS Group: Cost-effectiveness analysis of intensive blood-glucose control with metformin in overweight patients with type II diabetes (UKPDS No. 51). Diabetologia 44, 298–304 (2001)
Zhuo, X., Zhang, P., Hoerger, T.J.: Lifetime direct medical costs of treating type 2 diabetes and diabetic complications. Am. J. Prev. Med. 45(3), 253–261 (2013)
Menzin, J., Korn, J., Cohen, J., Lobo, F.: Relationship between glycaemic control and diabetes-related hospital costs in patients with type 1 or type 2 diabetes mellitus. J. Manag. Care Pharm. 16, 264–275 (2010)
Banerji, M.A., Dunn, J.D.: Impact of glycemic control on healthcare utilisation and costs of type 2 diabetes: current and future pharmacologic approaches to improving outcomes. Am. Health Drug Benefits 6(7), 382–392 (2013)
Degli Esposti, L., Saragoni, S., Buda, S., Sturani, A., Degli Esposti, E.: Glycaemic control and diabetes-related health care costs in type 2 diabetes; retrospective analysis based on clinical and administrative databases. ClinicoEconomics Outcomes Res. 5, 193–201 (2013)
McBrien, K.A., Manns, B.J., Chui, B., Klarenbach, S.W., Rabi, D., Ravani, P., Hemmelgarn, B., Wiebe, N., Au, F., Clement, F.: Health care costs in people with diabetes and their association with glycaemic control and kidney function. Diabetes Care (2012). https://doi.org/10.2337/dc12-0862
Shetty, S., Secnik, K., Oglesby, A.K.: Relationship of glycaemic control to total diabetes-related costs for managed care health plan members with type 2 diabetes. J. Manag. Care Pharm. 11(7), 559–564 (2005)
Skyler, J.S.: The economic burden of diabetes and the benefits of improved glycaemic control: the potential role of a continuous glucose monitoring system. Diabetes Technol. Ther. 2(1), S7–S12 (2000)
Trogdon, J.G., Hylands, T.: Nationally representative medical costs of diabetes by time since diagnosis. Diabetes Care 31(12), 2307–2311 (2008)
Nichols, G.A., Brown, J.B.: The impact of cardiovascular disease on medical care costs in subjects with and without type 2 diabetes. Diabetes Care 25(3), 482–486 (2002)
Turner, R.C., Cull, C.A., Frighi, V., Holman, R.R.: Glycemic control with diet, sulfonylurea, metformin, or insulin in patients with type 2 diabetes mellitus. JAMA 281, 2005–2012 (1999)
Booz & Co.: Diabetes Care in the Netherlands. Improving Health and Wealth. Novo Nordisk, Bagsværd (2011)
Hendriks, S.H.; Bilo, H.J.G.: Healthcare costs for men and women with type 2 diabetes in the Netherlands (2017) (work in progress)
Mohnen, S., Baan, C., Struijs, J.: Bundled payments for diabetes care and healthcare costs growth: a 2-year follow-up study. Am. J. Acc. Care 3(4), 63–70 (2015)
Hendriks, S.H., van Hateren, K.J.J., Groenier, K.H., Houweling, S.T., Maas, A.H.E.M., Kleefstra, N., Bilo, H.J.G.: Sex differences in the quality of diabetes care in the Netherlands (ZODIAC-45). PLoS One 10(12), e0145907 (2015)
Heij, C., de Boer, P., Franses, P., et al.: Econometric methods with applications in business and economics. Oxford University Press, New York (2004)
American Diabetes Association: Classification and diagnosis of diabetes. Diabetes Care 40(Suppl. 1), S11–S24 (2017)
Menendez, M.E., Neuhaus, V., van Dijk, N., Ring, D.: The Elixhauser comorbidity method outperforms the Charlson Index in predicting inpatient death after orthopaedic surgery. Clin. Orthop. Relat. Res. 472(9), 2878–2886 (2014)
Shaw, A., Bagshaw, S., Goldstein, S., Scherer, L., Duan, M., Schermer, C., Kellum, J.: Major complications, mortality, and resource utilization after open abdominal surgery: 0.9% saline compared to plasma-style. Ann. Surg. 255(5), 821–829 (2012)
Elixhauser, A., Steiner, C., Harris, D.R., Coffey, R.M.: Comorbidity measures for use with administrative data. Med. Care 36, 8–27 (1998)
Jae-Yong, S., Jeong-Hoon, A., Hee-Taik, K., Shinhye, K., Jin-Seub, H., Ji-Min, K., Jang-Mi, Y.: Comparison between ICPC (International Classification of Primary Care) classification and ICD (International Classification of Diseases) classification at primary care in Korea. National Evidence-based Healthcare Collaborating Agency (NECA), NECA-C-15-008 (2016)
Mundlak, Y.: On the polling of time series and cross section data. Econometrica 46(6), 9–85 (1978)
Farewell, F.T., Long, D.L., Tom, B.D.M., Yiu, S., Su, L.: Two-part and related regression models for longitudinal data. Annu. Rev. Stat. Appl. 4, 283–315 (2017)
Frondel. M., Vance C.: Interpreting the outcomes of two-part models. Discussion paper SFB 823 Nr. 11/2011 (2011)
Nichols, G.A., Glauber, H.S., Brown, J.B.: Type 2 diabetes: incremental medical care costs during the 8 years preceding diagnosis. Diabetes Care 23, 1654–1659 (2000)
Bron, M., Marynchenko, M., Yang, H., Yu, A.P., Wu, E.Q.: Hypoglycemia, treatment discontinuation, and costs in patients with type 2 diabetes mellitus on oral antidiabetic drugs. Postgrad. Med. 124(1), 124–132 (2015)
Booz & Co.: Diabetes Care in the Netherlands. Improving Health and Wealth. Novo Nordisk, Bagsværd (2011)
Brandle, M., Zhou, H., Smith, B.R.K., Marriott, D., Burke, R., Tabaei, B.P., Brown, M.B., Herman, W.H.: The direct medical cost of type 2 diabetes. Diabetes Care 26, 2300–2304 (2003)
Borah, B.J., Pharm, T.D., Bouchard, J., Aagren, M., Forma, F., Alemayehu, B.: A comparison of insulin use, glycemic control, and health care costs with insulin detemir and insulin glargine in insulin-naive patients with type 2 diabetes. Clin. Ther. 31(3), 623–631 (2009)
Van den Berghe, G., Wouters, P., Kesteloot, K., Hilleman, D.E.: Analysis of healthcare resource utilization with intensive insulin therapy in critically ill patients. Crit. Care Med. 34(3), 612–616 (2006)
WHO Global Health Observatory Data Repository [online database]. Geneva, World Health Organization. http://apps.who.int/gho/data/view.main (2013). Accessed 15 Nov 2017
Khan, L., Mincemoyer, S., Gabbay, R.A.: Diabetes registries: where we are and where are we headed? Diabetes Technol. Ther. 11, 255–262 (2009)
Brown, J.B., Nichols, G.A., Glauber, H.S.: Case control study of 10 years of comprehensive diabetes care. West. J. Med. 172, 85–90 (2000)
Acknowledgements
The authors would like to thank Chantal van Tilburg and Mirte van Galen for their help with the data, as well as Viola Angelini for her contribution and advice when revising the manuscript. We would also like to thank the anonymous reviewers for their useful comments, which have substantially improved the manuscript.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rodríguez-Sánchez, B., Feenstra, T.L., Bilo, H.J.G. et al. Costs of people with diabetes in relation to average glucose control: an empirical approach controlling for year of onset cohorts. Eur J Health Econ 20, 989–1000 (2019). https://doi.org/10.1007/s10198-019-01072-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-019-01072-z
Keywords
- Care costs
- Type 2 diabetes mellitus
- Average glucose control
- Diabetes treatment
- Diabetes duration
- Year of onset cohorts