Abstract
Background
In recent years, the type of surgical treatment for Achilles tendon rupture has been the subject of controversial debate. This biomechanical study evaluates for the first time in literature the ultimate failure load (UFL) of interlocking horizontal mattress (IHM) suture as compared with Kakiuchi suture in Achilles tendon rupture. The hypothesis is that IHM suture can be performed also for Achilles tendon rupture and ensures higher resistance compared with the traditional Kakiuchi suture.
Materials and methods
Twenty fresh bovine Achilles tendons were obtained. Ten preparations were randomly assigned to each of two different groups: group A (10 specimens) sutured by IHM technique, and group B (10 specimens) sutured by Kakiuchi technique. Each construct was mounted and fixed on a tensile testing machine. Static preconditioning of 50 N was applied for 5 min as initial tensioning to stabilize the mechanical properties of the graft, then a load to failure test was performed at crosshead speed of 500 mm/min.
Results
Ten specimens were tested for each group. The mean UFL was 228.6 ± 98.6 N in the IHM suture group and 96.57 ± 80.1 N in the Kakiuchi suture group. Statistical analysis showed a significant difference (p < 0.05) with better UFL in the IHM group. In both groups, the failure mode registered in each specimen was suture breakage (rupture of suture thread).
Conclusions
IHM suture achieved better UFL compared with Kakiuchi suture in an animal model of Achilles tendon repair. These results seem to support IHM as a valid option in Achilles tendon rupture.
Similar content being viewed by others
Introduction
Achilles tendon injury is a common musculoskeletal disorder that is increasing in frequency, affecting between 5.5 and 9.9 per 100,000 individuals each year in North America [14, 21]. To date, the type of surgical treatment for Achilles tendon rupture has been the subject of controversial debate, and the ideal form of treatment for Achilles tendon rupture remains controversial [23]. For many years, nonoperative treatment was the gold standard, but recent studies have shown that surgical treatment offers advantages over nonsurgical treatment in terms of clinical outcomes and recurrence rate [15]. One of the most important factors in modern surgery for Achilles tendon rupture is the strength of the suture, which is vital to reduce the number of re-ruptures and achieve early rehabilitation. The re-rupture rate is currently about 5 % among those treated with open surgical suture [3, 12, 24]. Early weight-bearing and strengthening exercises are increasingly being used to accelerate recovery [10, 13]. Therefore, strong repair should resist distraction, allowing early rehabilitation and promoting tendon healing [8, 17].
Early mobilization following Achilles tendon repair has been reported to be beneficial in terms of postoperative recovery and improved tendon vascularity [2, 11, 20, 25]. Clinically, patients with early mobilization after Achilles tendon repair have been shown to have shorter rehabilitation time and return-to-sport time [10, 28].
Determining the best suture in terms of strength is one of the most important challenges in this surgery. In this study, it was decided to compare interlocking horizontal mattress (IHM) versus Kakiuchi suture instead of standard techniques such as Kessler, Bunnell or Krackow suture because, nowadays, according to literature [9, 19, 22], Kakiuchi suture is one of the sutures offering greater guarantees in terms of stiffness and tightness in Achilles tendon rupture (Fig. 1).
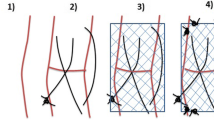
Interlocking horizontal mattress suture is the suture giving the best clinical results in literature for hand flexor repair [4]. The IHM suture technique is based on the standard surgical horizontal mattress suture design. With a regular forehand needle insertion, this technique commences on the far side of the repair and proceeds toward the surgeon. This method results in a suture pattern that has its strands running more longitudinally than the oblique patterns of both the cross-stitch and interlocking cross-stitch [5] (Fig. 2).
The aim of the authors is to perform IHM suture in Achilles tendon rupture, a technique never described before in literature.
The aim of this study is to evaluate the biomechanical properties in terms of the ultimate failure load (UFL) of the IHM suture versus the Kakiuchi suture for repair of Achilles tendon rupture. Among the techniques described over the years, there is no literature concerning IHM suture in Achilles tendon rupture. The presented biomechanical study evaluates for the first time in literature the UFL of IHM suture compared with Kakiuchi suture in Achilles tendon rupture. The hypothesis is that IHM could be performed also for Achilles tendon rupture and ensure higher resistance with respect to traditional Kakiuchi suture.
Materials and methods
Twenty fresh bovine Achilles tendons were obtained from the forefeet of 6-month-old animals. They were kept moist until testing by being wrapped in tissue paper soaked with Ringer’s solution and stored in sealed polyethylene bags. For this study, all applicable international, national, and/or institutional guidelines for the care and use of animals were followed. The same orthopedic surgeon performed tendon harvesting and preparation for testing of each specimen. All tendons were prepared with length of 120 mm, and a lesion was produced in each tendon by using a scalpel to create a clean division in the middle (60 mm). The width and thickness of all tendons were measured and are presented in Table 1. The specimens were not statistically different in terms of width or thickness (p < 0.05). Two different suture configurations were tested, using absorbable Ethicon PDS II® (polydioxanone) #2 suture (Fig. 2).
Ten preparations were randomly assigned to each of two different groups: group A (10 specimens) sutured with IHM technique, and group B (10 specimens) sutured with Kakiuchi technique. Kakiuchi technique is performed by passing transversely through the intact tendon a long straight needle threaded with an absorbable suture, with the same procedure being performed at two different levels on both the proximal and distal stumps of the tendon. Proximally, the suture wire is passed at 0.5 and 1 cm from the cut tendon edge; distally, the suture wire is passed at 0.5 and 1 cm from the rupture site (Fig. 1). In vivo the ankle is held at 30° plantar flexion and the knee flexed to 90° while the sutures are tied. Direct observation confirms that the space between the two stumps is eliminated [9]. The IHM repair technique is performed by running an interlocking horizontal mattress suture, starting at the far end. The suture needle passes underneath the prior crossing suture to lock each throw. When the suture is finished, it is tied at the near end as shown in Fig. 2. In this technique, suture is performed at 0.5 cm from the tendon edge. For IHM, there are six loops for each suture.
Each construct was mounted and fixed on a tensile testing machine (model Z010, Zwick-Ruell, Ulm, Germany) using two metal clamps connected to the load cell. The load was applied parallel to the longitudinal axis of the specimen to obtain the worst load scenario. The specifically designed clamps were frozen to avoid graft slippage from the clamp. Static preconditioning of 50 N was applied for 5 min as initial tensioning to stabilize the mechanical properties of the graft, then a load to failure test was performed at crosshead speed of 500 mm/min. Data regarding the ultimate failure load (UFL) of each specimen were recorded using Textexpert 8.1 software (Zwick-Ruell) and evaluated using a load–displacement curve. We also recorded the failure mode for each construct (Figs. 3, 4, 5, 6).
A total sample size of 18 was considered adequate for overall comparison of the two techniques with respect to construct measurements, assuming an effect size of 0.25, alpha-value of 0.05, and beta-value of 0.20 (study power 80 %).
For all variables, normality of data was ascertained by Kolmogorov–Smirnov test. Differences in construct tensile properties (UFL) between the two groups were compared by Mann–Whitney test. All data were analyzed by a single blinded researcher. The Statistical Package for the Social Sciences (SPSS) version 22 was used for calculations.
Results
Ten specimens were tested in each group, resulting in a total of 20 specimens. The results are summarized in Table 2. The mean UFL was 228.6 ± 98.6 N in the IHM suture group and 96.5 ± 80.1 N in the Kakiuchi suture group. Statistical analysis showed a significant difference (p < 0.05) with better UFL for the IHM group. In both groups, the failure mode registered in each specimen was suture breakage (rupture of suture thread).
Discussion
The most important finding of this study is that IHM suture exhibited better UFL compared with Kakiuchi suture.
During the early rehabilitation phase, when passive range-of-movement exercises are started, the forces in the Achilles tendon of a healthy limb with the ankle at neutral dorsiflexion range from 70.6 N with the knee in full extension to 17.8 N with the knee flexed to 50° [17] .
Achilles tendon forces at 10° and 20° of ankle dorsiflexion range from 183.2 to 83.4 N and from 401.8 to 215.5 N, respectively, with the knee in full extension and with the knee flexed to 50° [22]. Forces of 190 N are produced when walking in a cam walker with a 1-inch heel raise [1]. When walking, these forces are 2.1 times higher than those exerted by the body weight [6]. The forces on the Achilles tendon during walking and running exceed the strength of all repairs; thus, careful postoperative treatment is imperative [27].
The results presented herein indicate that the IHM technique applied in our study resulted in sufficient primary UFL (228.60 N) to withstand the forces experienced during the early rehabilitation phase, except for passive exercises with 20° of ankle dorsiflexion and knee in full extension (401.8 N).
Another important finding is that we registered a homogeneous mode of failure consisting in suture breakage. No suture slippage across tendon was found, thus we can speculate that both sutures distribute tension across the tendon, avoiding excessive stress that could damage the tendon itself, which has typically undergone degenerative changes in Achilles tendon rupture.
Surgical repair of Achilles tendon rupture is commonly performed, mostly in young active patients, and multiple techniques for treatment of Achilles tendon rupture have been described [7, 26, 28].
The aim of surgical treatment of acute Achilles tendon rupture is to obtain the maximum primary mechanical stability of the sutured tendon, which is crucial to ensure a low rate of postoperative re-rupture and to allow early rehabilitation. For this reason, the type of suture used can affect the clinical outcome and change the postoperative protocol. We tried to determine the load to failure by simulating clinical failure, in which tendon re-rupture occurs in the first 3 months after surgery as a result of increased load. However, this study has several limitations.
First, this was an ex vivo animal study, so we could not reproduce the tendon properties in vivo in humans [16, 18]. We used an apparently healthy tendon, which is different from that usually found in the surgical scenario, where rupture typically appears as a result of degenerative changes involving tissue of the tendon. Moreover, the lesion in the tendon was produced by using a scalpel to create a clean division, in contrast to the frayed ends associated with clinical injury [18]. For all these reasons, only clinical studies might clarify whether IHM suture is truly superior to Kakiuchi suture in the chronic tendinitis scenario. Bovine tendon was tested because it is readily available and has already been used in similar biomechanical studies [18]. Another limitation is that we only recorded data for the UFL, because we aimed only to determine whether IHM could offer better biomechanical performance, considering that graft slippage is more correlated to the characteristics of the tendon itself, which has viscoelastic properties. Finally, the load axis was applied parallel to the graft, which is different from the complex forces that the repaired tendon has to resist during the early rehabilitation phase.
In conclusion, IHM suture exhibited better UFL compared with Kakiuchi suture in an animal model of Achilles tendon repair. These results seem to support IHM as a valid option in Achilles tendon rupture, though the clinical implications of the various repairs were not studied. Many minimally invasive approaches, including for the Kakiuchi technique, have been described in literature for Achilles tendon repair. IHM suture in vivo can also be performed minimally invasively.
More clinical studies are needed to confirm the functional and biomechanical effectiveness of this suture technique.
References
Akizuki KH, Gartman EJ, Nisonson B, Ben-Avi S, McHugh MP (2001) The relative stress on the Achilles tendon during ambulation in an ankle immobiliser: implications for rehabilitation after Achilles tendon repair. Br J Sports Med 35:329–334
Aspenberg P (2007) Stimulation of tendon repair: mechanical loading, GDFs and platelets: a mini-review. Int Orthop 31:783–789
Cetti R, Christensen SE, Ejsted R et al (1993) Operative versus nonoperative treatment of Achilles tendon rupture. A prospective randomized study and review of the literature. Am J Sports Med 21:791–799
Dona E, Gianoutsos MP, Walsh WR (2004) Optimizing biomechanical performance of the 4-strand cruciate flexor tendon repair. J Hand Surg Am 29(4):571–580
Dona E, Turner AWL, Gianoutsos MP, Walsh WR (2003) Biomechanical properties of four circumferential flexor tendon suture techniques. J Hand Surg 28A:824–831
Fröberg A, Komi P, Ishikawa M, Movin T, Arndt A (2009) Force in the Achilles tendon during walking with ankle foot orthosis. Am J Sports Med 37:1200–1207
Ismail M, Karim A, Shulman R, Amis A, Calder J (2008) The Achillon achilles tendon repair: is it strong enough? Foot Ankle Int 29:808–813
Schneppendahl J, Thelen S, Schek A et al (2012) Initial stability of two different adhesives compared to suture repair for acute Achilles tendon rupture—a biomechanical evaluation. Int Orthop (SICOT) 36:627–632. doi:10.1007/s00264-011-1357-9
Kakiuchi M (1995) A combined open and percutaneous technique for repair of tendo Achillis. Comparison with open repair. J Bone Jt Surg Br 77(1):60–63
Kearney RS, Costa ML (2012) Current concepts in the rehabilitation of an acute rupture of the tendo Achillis. J Bone Jt Surg [Br] 94-B:28–31
Kjaer M, Langberg H, Miller BF (2005) Metabolic activity and collagen turnover in human tendon in response to physical activity. J Musculoskelet Neuronal Interact 5:41–52
Lo IK, Kirkley A, Nonweiler B (1997) Operative versus nonoperative treatment of acute Achilles tendon ruptures: a quantitative review. Clin Sports Med 7:207–211
Lovric V, Kanazawa T, Nakamura Y et al (2011) Effects of gaps induced into the ACL tendon graft on tendon-bone healing in a rodent ACL reconstruction model. Muscle Ligament Tendon J 3:91–99
Maffulli N, Waterston SW, Squair J, Reaper J, Douglas AS (1999) Changing incidence of Achilles tendon rupture in Scotland: a 15-year study. Clin J Sport Med 9:157–160
Möller M, Movin T, Granhed H, Lind K, Faxén E, Karlsson J (2001) Acute rupture of tendo Achilles. A prospective randomised study of comparison between surgical and non-surgical treatment. J Bone Jt Surg (Br) 83(6):843–848
Mortensen HM, Skov O, Jensen PE (1999) Early motion of the ankle after operative treatment of a rupture of the Achilles tendon: a prospective, randomized clinical and radiographic study. J Bone Jt Surg [Am] 81-A:983–990
Orishimo KF, Burstein G, Mullaney MJ et al (2008) Effect of knee flexion angle on Achilles tendon force and ankle joint plantarflexion moment during passive dorsiflexion. J Foot Ankle Surg 47:34–39
Ortiz C, Wagner E, Mocoçain P, Labarca G, Keller A, Del Buono A, Maffulli N (2012) Biomechanical comparison of four methods of repair of the Achilles tendon: a laboratory study with bovine tendons. J Bone Jt Surg Br 94(5):663–667. doi:10.1302/0301-620X.94B5.27642
Rebeccato A, Santini S, Salmaso G, Nogarin L (2001) Repair of the achilles tendon rupture: a functional comparison of three surgical techniques. J Foot Ankle Surg 40(4):188–194
Schepull T, Aspenberg P (2013) Early controlled tension improves the material properties of healing human Achilles tendons after ruptures: a randomized trial. Am J Sports Med 41:2550–2557
Suchak AA, Bostick G, Reid D, Blitz S, Jomha N (2005) The incidence of Achilles tendon ruptures in Edmonton, Canada. Foot Ankle Int 26:932–936
Vadalà A, De Carli A, Vulpiani MC, Iorio R, Vetrano M, Scapellato S, Suarez T, Di Salvo F, Ferretti A (2012) Clinical, functional and radiological results of Achilles tenorraphy surgically treated with mini-open technique. J Sports Med Phys Fitness 52(6):616–621
Wallace RG, Heyes GJ, Michael AL (2011) The non-operative functional management of patients with a rupture of the tendo Achillis leads to low rates of re-rupture. J Bone Jt Surg [Br] 93-B:1362–1366
Winter E, Ambacher T, Maurer F et al (1995) Surgical therapy of Achilles tendon rupture. Unfallchirurg 98:468–473
Wong J, Barrass V, Maffulli N (2002) Quantitative review of operative and nonoperative management of Achilles tendon ruptures. Am J Sport Med 30:565–575
Worth N, Ghosh S, Maffulli N (2007) Management of acute Achilles tendon ruptures in the United Kingdom. J Orthop Surg (Hong Kong) 15:311–314
Zandbergen RA, de Boer SF, Swierstra BA, Dayi J, Kleinrensink GJ, Beumer A (2005) Surgical treatment of Achilles tendon rupture: examination of strength of 3 types of suture techniques in a cadaver model. Acta Orthop 76(3):408–411
Wu Z, Hua Y, Li H, Chen S, Li Y (2015) Biomechanical comparison of three methods for distal Achilles tendon reconstruction. Knee Surg Sports Traumatol Arthrosc 23(12):3756–3760
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Patient consent
Obtaining the informed consent form involved patients was waived by the Research Ethics Committee.
Ethical approval
For this study all applicable international, national and/or institutional guidelines for the care and use of animals were followed.
Funding
No funding was delivered for this study.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Guzzini, M., Lanzetti, R.M., Proietti, L. et al. Interlocking horizontal mattress suture versus Kakiuchi technique in repair of Achilles tendon rupture: a biomechanical study. J Orthop Traumatol 18, 251–257 (2017). https://doi.org/10.1007/s10195-017-0455-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10195-017-0455-x