Abstract
Background
The use of peripheral locked screws has reduced glenoid baseplate failure rates in reverse shoulder arthroplasty. However, situations may arise when one or more non-locked screws may be preferred. We aimed to determine if different combinations of locked and non-locked screws significantly alter acute glenoid baseplate fixation in a laboratory setting.
Materials and methods
Twenty-eight polyurethane trabecular bone surrogates were instrumented with a center screw-type glenoid baseplate and fixated with various combinations of peripheral locked and non-locked screws (1-, 2-, 3- and 4-locked con). Each construct was tested through a 55° arc of abduction motion generating compressive and shear forces across the glenosphere. Baseplate micromotion (μm) was recorded throughout 10,000 cycles for each model.
Results
All constructs survived 10,000 cycles of loading without catastrophic failure. One test construct in the 1-locked fixation group exhibited a measured micromotion >150 μm (177.6 μm). At baseline (p > 0.662) and following 10,000 cycles (p > 0.665), no differences were observed in baseplate micromotion for screw combinations that included one, two, three and four peripheral locked screws. The maximum difference in measured micromotion between the extremes of groups (1-locked and 4-locked) was 29 µm.
Conclusions
Hybrid peripheral screw fixation using combinations of locked and non-locked screws provides secure glenoid baseplate fixation using a polyurethane bone substitute model. Using a glenosphere with a 10-mm lateralized center of rotation, hybrid baseplate fixation maintains micromotion below the necessary threshold for bony ingrowth.
Level of Evidence
N/A/, basic science investigation.
Similar content being viewed by others
Introduction
Improvements in glenoid baseplate fixation have been critical to the success of the modern reverse shoulder replacement. Recognition of the importance of baseplate tilt [1,2,3], optimal screw placement [4,5,6,7,8,9], glenoid reaming techniques [10], peripheral screw fixation [11], baseplate shape and position [9, 12, 13], and introduction of bone ingrowth technologies [13] have contributed to avoiding the catastrophic baseplate failures described using first-generation reverse shoulder replacements [14,15,16,17,18,19,20,21]. In combination with improved surgical technique and implant enhancements, baseplate failures are less common [6].
One key modification which helped improve baseplate fixation was the introduction of peripheral locked screws. First tested by Harman et al. [11], locked screw use significantly enhanced baseplate fixation and minimized micromotion at the baseplate−glenoid bone interface. This was also observed in clinical practice. Frankle et al. initially reported an 11% baseplate failure rate using peripheral non-locked 3.5-mm screws [22]. However, in a 5-year follow-up series using the same implant with 5.0-mm peripheral locked screws, the baseplate failure rate was reduced to 0% [23]. This has led most surgeons to utilize locked screws for nearly all peripheral screw fixation opportunities when using a central screw-based baseplate.
There are, however, clinical scenarios when a surgeon may prefer to use non-locked peripheral screws. The concept of hybrid fixation, where combinations of locked and non-locked screws are used together, has been a longstanding feature used in locked plate osteosynthesis and has been shown to be biomechanically similar while also providing the potential benefits of compression or aiding with reduction [24,25,26,27,28]. Variations in hybrid peripheral screw combinations have not been tested for reverse shoulder glenoid baseplate fixation. The purpose of this study was to evaluate initial glenoid baseplate fixation using a variety of combinations of locked and non-locked peripheral screws. We hypothesized that glenoid baseplate micromotion would be sufficiently minimized using all combinations of locked and non-locked peripheral screws.
Materials and methods
Twenty-eight synthetic trabecular bone surrogate cylinders (Sawbones® Model #1522-12, Rigid Cellular Foam; Pacific Research Laboratories, Vashon, WA, USA) with a nominal density of 0.32 g/cm3 (ASTM F1839-08) were utilized in the current investigation. This nominal was chosen as an intermediary between poor quality (0.24 g/cm3) and good quality (0.48 g/cm3) cancellous bone used by others in studies of similar scope [33]. Upon receipt of the blocks (40 × 130 × 180 mm) each was machined into cylinders measuring 44.5 mm in diameter and 40 mm in height.
This study used the glenoid components of a single reverse shoulder arthroplasty system (RSP®; DJO Global, Austin, TX, USA). The baseplate consists of a single central 6.5-mm lag screw in combination with four peripheral screw holes, which can be used in locked or non-locked fashion. The underside of the baseplate is coated with hydroxyapatite to facilitate bony ingrowth in vivo. All baseplates were fixed perpendicular to the bone block substitutes. Briefly, a 2.5-mm drill was used to define the trajectory for the baseplate’s central screw. A 6.5-mm tap was used to create the threads for the central screw. With the tap still in place, a reamer was used to create the circumferential concavity required to accommodate the underside of the baseplate, which was then inserted and tightened to a maximum torque of 3.5 N-m (Model DID-04 Digital Torque Screwdriver; Imada, Inc. Northbrook, IL, USA). For this study, we evaluated baseplate fixation using four combinations of locked (5-mm diameter) and (3.5-mm diameter) non-locked peripheral screws in seven (n = 7) cylinders per fixation group—(1) 1 locked screw + 3 non-locked screws (1-locked), (2) 2 locked screws + 2 non-locked screws (2-locked), (3) 3 locked screws + 1 non-locked screw (3-locked), and (4) 4 locked screws (4-locked). All locked and non-locked screws were the same length as determined by a retrospective analysis of a consecutive series of 100 reverse shoulder arthroplasty surgeries using the same glenoid baseplate. This identified an average peripheral screw length of 21 mm. Thus, 22-mm screws were selected for all locked and non-locked screws.
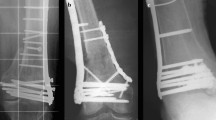
For peripheral screw placement, a 4-in-1 drill guide was used which allows for drilling and placement of screws (after the inner sleeve is removed) in a constant perpendicular orientation to the baseplate. For non-locked and locked peripheral screws, respectively, 2.5 and 4-mm drills were used to define the screw trajectory in the cylinder. On the circular surface of the baseplate-instrumented Sawbones® cylinder, one screw hole was arbitrarily defined as superior, with anterior, inferior and posterior orientations defined thereafter in clockwise fashion, thereby mimicking a shoulder’s right-sided glenoid orientation (Fig. 1). For the 1-locked screw configuration, the locked peripheral screw was placed in the superior screw hole. In the 2-locked group, locked screws were placed superiorly and inferiorly. Finally, for the 3-locked screw configuration, locked screws were placed superiorly, inferiorly, and posteriorly. Peripheral non-locked screws were advanced to a depth of 22 mm in the foam cylinder and tightened to 0.7 N-m using a torque limiting screw driver. This torque magnitude was determined in pilot experiments and represents the highest, consistently achievable torque in this particular Sawbones® block density without loss of non-locked screw purchase or applied torque. All locked screws were tightened to 2.5 N-m with care taken not to cross the threads. Thereafter, a differential variable reluctance transducer (DVRT) (Model MG-DVRT®; LORD MicroStrain® Sensing Systems, Williston, VT, USA) with 3 μm accuracy, was mounted to the instrumented surface of the Sawbones® in the inferior/superior direction with a custom-designed attachment rig such that the sensor was in contact with the periphery of the baseplate immediately adjacent to the superior screw hole (Fig. 2). Inferior/superior micromotion was of primary interest given the orientation of the applied loads in our test setup, which were applied to the baseplate in the scapular plane to simulate abduction and the primary function of reverse shoulders. Out-of-plane micromotion in the anterior/posterior direction was not measured because no shear loads were applied in the axial plane. After screw placement and DVRT attachment, a 32-mm neutral glenosphere (DJO Global, Austin, TX, USA) was impacted onto the baseplate. This glenosphere has a center of rotation 10 mm from the glenoid surface.
Position of locked and unlocked screws within the baseplate for each configuration. 1a Baseplate with four locked screws, 2a baseplate with three locked and one unlocked screw, 3a baseplate with two locked and two unlocked screws, 4a baseplate with one locked and three unlocked screws. L locked, U unlocked
We adopted a testing methodology identical to our previously published work [37]. Briefly, the instrumented Sawbones® cylinder was mounted in a swing arm attached to the torque motor of a servoelectric test frame (Model 800LE; Test Resources, Shakopee, MN, USA). Test specimens were cycled through a 55° arc of motion at 1 Hz, while the test frame’s actuator applied a constant 750 N compressive force via a glenosphere size-matched humeral component polyethylene neutral liner, in similar fashion to the methods adopted by previous authors (Fig. 3) [13, 29, 37]. The orientation of the test block was such that the arc of motion occurred in the scapular plane defined by the superior and inferior screw holes of the baseplate, thus serving to approximate a 25°−80° humeral abduction motion relative to a fixed scapula. This loading setup induces a maximum shear force of 346 N at the extremes of the motion arc from neutral (i.e., ±27.5°) and a 750 N compressive load at the neutral position (Fig. 4). The continuous analog voltage output from the DVRT was queried at the beginning of testing and every 500 cycles thereafter through 10,000 cycles of loading. The measured voltage was related to baseplate micromotion (μm) using the manufacturer’s provided linear calibration coefficient. Here, micromotion was defined as the average of the absolute values of micromotion measured by the DVRT at the arc of motion extremes (+27.5° and −27.5°) over 20 loading cycles for each data collection time point. Testing was stopped if catastrophic construct failure was grossly observed.
Micromotion data were analyzed using a 2-way ANOVA for intra-group (time) and inter-group (fixation) comparisons and post hoc comparisons were performed with Bonferroni correction at a significance level of 0.05. The number of test constructs in which micromotion was measured >150 μm threshold commonly accepted for osseous integration was reported.
Results
All 28 instrumented cylinders survived 10,000 cycles of loading without catastrophic failure. No gross evidence of baseplate subsidence into the test blocks was noted in any specimen. One test construct in the 1-locked fixation group exhibited a measured micromotion >150 μm (177.6 μm) (Table 1). This was observed after 9500 cycles. No constructs in the 2-locked, 3-locked or 4-locked fixation groups exhibited micromotion >150 μm.
There was no difference in baseplate micromotion at baseline between any of the fixation groups (p > 0.662) (Fig. 5a). After 10,000 cycles of loading, the 4-locked fixation group exhibited the lowest measured baseplate micromotion, on average (68.1 ± 15.3 μm; range 45.2–91.0 μm), although this was not significantly different (p > 0.665) from the 1-locked (97.1 ± 47.2 μm; range 40.1–177.6 μm), 2-locked (76.7 ± 34.5 μm; range 43.1–143.1 μm), or 3-locked fixation groups (72.4 ± 15.3 μm; range 39.5–121.6 μm) (Figs. 5b, 6).
Discussion
Critical to glenoid component survivability of the reverse shoulder replacement is obtaining sufficient initial fixation on the glenoid bone to facilitate osseous integration [4, 6, 11]. Minimization of micromotion <150 µm between an implant and bone has been shown to be optimal in achieving a biologic environment for bone growth onto metal arthroplasty surfaces [30,31,32]. Extrapolating these findings and applying them to the reverse shoulder glenoid component, numerous attempts have been made at enhancing baseplate fixation with the common goal of limiting micromotion between the glenoid component and the prepared glenoid surface. Over the past 15 years, advancements in surgical technique, implant design modifications, and understanding of scapular anatomy have helped surgeons improve baseplate failure rates. Of these enhancements, screw fixation has been noted as the most important feature of enhanced fixation [4, 9, 12].
Use of a glenosphere implant with a more lateral center of rotation was met with controversy based on historical implant failures seen with earlier generation implants [14,15,16,17,18,19,20,21]. The first modern reverse shoulder replacement to revisit a more lateralized center of rotation utilized a central screw baseplate and four peripheral non-locked 3.5-mm screws. Using all peripheral non-locked screws, the glenoid baseplate failure rate was 11% [22]. With continued understanding of surgical technique and replacement of the 3.5-mm peripheral non-locked screws with 5.0-mm locked screws, the incidence of glenoid baseplate failures was reduced to 0% in a 5-year minimum follow-up study [33]. This clinical experience validated the mechanical study reported by Harman et al. [11] which showed how peripheral locked screws were superior to non-locked screws at maximizing baseplate fixation <150 µm micromotion threshold. Surgeons have thus gained comfort using a glenoid baseplate with four peripheral locked screws. There are certainly cases where four peripheral locked screws are either not possible or may not be of optimal surgical preference. Included in these scenarios are cases where there is limited bone remaining, such that a screw would capture minimal bone or result in a prominent screw; or cases where a larger locked screw might not be optimal, creating a potential stress riser for an acromion spine fracture [34]. Additionally, there are situations when further glenoid component compression is desirable, which can only be achieved by using a non-locked screw. In these cases, the surgeon may elect to utilize a non-locked screw rather than a locked screw. This concept of hybrid fixation is now commonplace in fracture management using locked plates, but prior to this study had not been tested for applicability in the reverse shoulder replacement glenoid component.
Our study results demonstrate that a variety of hybrid peripheral screw combinations can provide sufficient glenoid component fixation using a glenosphere with a more lateral center of rotation. No statistical differences were observed in baseplate micromotion for peripheral screw combinations that included one, two, three and four peripheral locked screws. This was true at initial fixation (p > 0.662) and following 10,000 cycles (p > 0.665) using a bone substrate model that simulates poor glenoid bone quality often seen in reverse shoulder arthroplasty patients [13]. In fact, the maximum difference in measured micromotion between the extremes of groups (1-locked and 4-locked) was 29 µm (97 µm and 68 µm, respectively).
With increased cyclic loading of the glenosphere, there was increased micromotion seen at the baseplate−bone model interface. However, only one of the 28 tested constructs exhibited micromotion >150 µm threshold within the 10,000 cycles. This specimen utilized a single locked and three non-locked peripheral screws and did not reach this threshold until after 9500 cycles. While we noted no statistically significant differences between fixation groups, the variability in measured micromotion after 10,000 cycles of loading was decreased with an increasing number of locked peripheral screws. Thus, these study findings suggest that (1) hybrid fixation is a reasonable option for surgeons to consider when placing peripheral screws around a central screw baseplate and that (2) maximizing the number of peripheral locked screws, when clinically feasible, may more consistently maintain baseplate fixation through the postoperative rehabilitation course. Furthermore, use of a glenosphere with a center of rotation 10 mm lateral to the glenoid can be utilized with a glenoid baseplate secured with a combination of locked and non-locked screws without compromising the fixation necessary for ingrowth.
Several steps were taken to help maintain uniformity of the tested constructs and strengthen the validity of the data. Non-locked screws have the potential to lose fixation during implantation by stripping out. A pilot study was thus performed to evaluate the torque at which peripheral non-locked screws stripped (documented as a sharp drop in measured torque) within the bone model and lost fixation. All of the peripheral non-locked screws were then implanted within the torque limits observed, ensuring that each screw placed provided similar fixation. Additionally, the orientation of the baseplate was controlled such that the screw orientation remained constant, preventing variability in rigidity based on the orientation of the locked and non-locked screws. Finally, the central screw baseplates were implanted with an identical maximum torque to ensure that uniform compression was achieved with each tested model.
The cyclic loading protocol in this study mimics the stresses that might be observed in vivo and was similar to the technique utilized in our previous work [37] and by Roche et al. [29]. This consisted of a 750 N axial load applied through the humeral component while the glenosphere was rotated about the humeral component in a 55° arc of motion. This loading profile induces a maximum calculated shear force of 346 N and a maximum compressive load of 750 N. The applied compressive load magnitude of 750 N is in good agreement with data published by Bergmann et al. [35] who measured in vivo glenohumeral joint loads during abduction in patients with load/moment measuring total shoulder arthroplasty prostheses. However, the loading approach used here may be considered worst case, as muscle forces in reverse shoulder arthroplasty patients have been reported to vary between 30 and 50% less than in anatomical arthroplasty patients due to a compromised rotator cuff [36]. It was felt that this method of testing would better simulate what would be observed clinically rather than the methodologies noted by Harman et al. [11]. Nonetheless, the findings observed in the 4-locked screw group were similar to the findings reported by Harman et al. [11] using the identical 4-peripheral screw baseplate.
Limitations of this study relate to the use of polyurethane foam. While efforts were made to simulate the clinical environment, including placement of screws within torque limits, variations in patient bone quality may have different effects on hybrid peripheral screw baseplate fixation strength. Additionally, the screws placed were all within the foam model and did not obtain bi-cortical purchase that may occur in vivo. However, even without bi-cortical purchase, all but one non-locked baseplate configurations were able to limit micromotion <150 µm through 10,000 cycles. Finally, this study represents the initial fixation obtained by the glenoid baseplate. With the limitations of postoperative rehabilitation protocols, osseous integration of the glenoid baseplate may occur well before the 10,000 cycles tested in this study. Further investigation of the clinical outcomes using hybrid peripheral screw fixation of a central screw baseplate are warranted to validate the findings of this study.
In summary, hybrid peripheral screw fixation using combinations of locked and non-locked screws provides secure glenoid baseplate fixation using a polyurethane bone substitute model. Glenospheres with a more lateral center of rotation can be utilized together with a hybrid combination of peripheral glenoid baseplate screws without compromising fixation necessary for ingrowth of bone into the implant.
References
Gutierrez S, Greiwe RM, Frankle MA, Siegal S, Lee WE 3rd (2007) Biomechanical comparison of component position and hardware failure in the reverse shoulder prosthesis. J Shoulder Elbow Surg 16:S9–S12
Gutierrez S, Walker M, Willis M, Pupello DR, Frankle MA (2011) Effects of tilt and glenosphere eccentricity on baseplate/bone interface forces in a computational model, validated by a mechanical model, of reverse shoulder arthroplasty. J Shoulder Elbow Surg 20:732–739
Kwon YW, Forman RE, Walker PS, Zuckerman JD (2010) Analysis of reverse total shoulder joint forces and glenoid fixation. Bull NYU Hosp Jt Dis 68:273–280
Chebli C, Huber P, Watling J, Bertelsen A, Bicknell RT, Matsen F 3rd (2008) Factors affecting fixation of the glenoid component of a reverse total shoulder prothesis. J Shoulder Elbow Surg 17:323–327
Frankle MA, Teramoto A, Luo ZP, Levy JC, Pupello D (2009) Glenoid morphology in reverse shoulder arthroplasty: classification and surgical implications. J Shoulder Elbow Surg 18:874–885
Hoenig MP, Loeffler B, Brown S et al (2010) Reverse glenoid component fixation: is a posterior screw necessary? J Shoulder Elbow Surg 19:544–549
Hopkins AR, Hansen UN, Bull AM, Emery R, Amis AA (2008) Fixation of the reversed shoulder prosthesis. J Shoulder Elbow Surg 17:974–980
Humphrey CS, Kelly JD 2nd, Norris TR (2008) Optimizing glenosphere position and fixation in reverse shoulder arthroplasty, part two: the three-column concept. J Shoulder Elbow Surg 17:595–601
Parsons BO, Gruson KI, Accousti KJ, Klug RA, Flatow EL (2009) Optimal rotation and screw positioning for initial glenosphere baseplate fixation in reverse shoulder arthroplasty. J Shoulder Elbow Surg 18:886–891
Sutton LG, Werner FW, Jones AK, Close CA, Nanavati VN (2010) Optimization of glenoid fixation in reverse shoulder arthroplasty using 3-dimensional modeling. J Shoulder Elbow Surg 19:664–669
Harman M, Frankle M, Vasey M, Banks S (2005) Initial glenoid component fixation in “reverse” total shoulder arthroplasty: a biomechanical evaluation. J Shoulder Elbow Surg 14:162S–167S
James J, Huffman KR, Werner FW, Sutton LG, Nanavati VN (2012) Does glenoid baseplate geometry affect its fixation in reverse shoulder arthroplasty? J Shoulder Elbow Surg 21:917–924
Stroud NJ, DiPaola MJ, Martin BL et al (2013) Initial glenoid fixation using two different reverse shoulder designs with an equivalent center of rotation in a low-density and high-density bone substitute. J Shoulder Elbow Surg 22:1573–1579
Bodey WN, Yeoman PM (1983) Prosthetic arthroplasty of the shoulder. Acta Orthop Scand 54:900–903
Coughlin MJ, Morris JM, West WF (1979) The semiconstrained total shoulder arthroplasty. J Bone Joint Surg Am 61:574–581
Fenlin JM Jr (1975) Total glenohumeral joint replacement. Orthop Clin North Am 6:565–583
Franklin JL, Barrett WP, Jackins SE, Matsen FA 3rd (1988) Glenoid loosening in total shoulder arthroplasty. Association with rotator cuff deficiency. J Arthroplasty 3:39–46
Gerard Y, Leblanc JP, Rousseau B (1973) [A complete shoulder prosthesis]. Chirurgie 99:655–663
Kolbel R, Friedebold G (1973) [Shoulder joint replacement]. Arch Orthop Unfallchir 76:31–39
Neer CS 2nd, Craig EV, Fukuda H (1983) Cuff-tear arthropathy. J Bone Joint Surg Am 65:1232–1244
Reeves B, Jobbins B, Flowers F, Dowson D, Wright V (1972) Some problems in the development of a total shoulder endo-prosthesis. Ann Rheum Dis 31:425–426
Frankle M, Siegal S, Pupello D, Saleem A, Mighell M, Vasey M (2005) The reverse shoulder prosthesis for glenohumeral arthritis associated with severe rotator cuff deficiency. A minimum two-year follow-up study of sixty patients. J Bone Joint Surg Am 87:1697–1705
Cuff D, Pupello D, Virani N, Levy J, Frankle M (2008) Reverse shoulder arthroplasty for the treatment of rotator cuff deficiency. J Bone Joint Surg Am 90:1244–1251
Doornink J, Fitzpatrick DC, Boldhaus S, Madey SM, Bottlang M (2010) Effects of hybrid plating with locked and nonlocked screws on the strength of locked plating constructs in the osteoporotic diaphysis. J Trauma 69:411–417
Estes C, Rhee P, Shrader MW, Csavina K, Jacofsky MC, Jacofsky DJ (2008) Biomechanical strength of the Peri-Loc proximal tibial plate: a comparison of all-locked versus hybrid locked/nonlocked screw configurations. J Orthop Trauma 22:312–316
Gardner MJ, Griffith MH, Demetrakopoulos D et al (2006) Hybrid locked plating of osteoporotic fractures of the humerus. J Bone Joint Surg Am 88:1962–1967
Stoffel K, Lorenz KU, Kuster MS (2007) Biomechanical considerations in plate osteosynthesis: the effect of plate-to-bone compression with and without angular screw stability. J Orthop Trauma 21:362–368
Sutherland GB, Creekmore T, Mukherjee DP, Ogden AL, Anissian L, Marymont JV (2010) Biomechanics of humerus fracture fixation by locking, cortical, and hybrid plating systems in a cadaver model. Orthopedics 33(8). doi:10.3928/01477447-20100625-02
Roche CP, Stroud NJ, Flurin PH, Wright TW, Zuckerman JD, DiPaola MJ (2014) Reverse shoulder glenoid baseplate fixation: a comparison of flat-back versus curved-back designs and oval versus circular designs with 2 different offset glenospheres. J Shoulder Elbow Surg 23:1388–1394
Cameron HU, Pilliar RM, MacNab I (1973) The effect of movement on the bonding of porous metal to bone. J Biomed Mater Res 7:301–311
Jasty M, Bragdon C, Burke D, O’Connor D, Lowenstein J, Harris WH (1997) In vivo skeletal responses to porous-surfaced implants subjected to small induced motions. J Bone Joint Surg Am 79:707–714
Pilliar RM, Lee JM, Maniatopoulos C (1986) Observations on the effect of movement on bone ingrowth into porous-surfaced implants. Clin Orthop Relat Res. 208:108–113
Cuff D, Clark R, Pupello D, Frankle M (2012) Reverse shoulder arthroplasty for the treatment of rotator cuff deficiency: a concise follow-up, at a minimum of five years, of a previous report. J Bone Joint Surg Am 94:1996–2000
Crosby LA, Hamilton A, Twiss T (2011) Scapula fractures after reverse total shoulder arthroplasty: classification and treatment. Clin Orthop Relat Res 469:2544–2549
Bergmann G, Graichen F, Bender A et al (2011) In vivo gleno-humeral joint loads during forward flexion and abduction. J Biomech 44:1543–1552
Terrier A, Reist A, Merlini F, Farron A (2008) Simulated joint and muscle forces in reversed and anatomic shoulder prostheses. J Bone Joint Surg Br 90:751–756
Formaini NT, Everding NG, Levy JC, Santoni BG, Nayak AN, Wilson C, Cabezas AF (2015) The effect of glenoid bone loss on reverse shoulder arthroplasty baseplate fixation. J Shoulder Elbow Surg 24(11):e312–e319
Acknowledgements
We would like to acknowledge Kaitlyn Christmas, BS and Andres F. Cabezas, ME for assistance with data collection. This study was funded by a grant from DJO Global.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This research was supported by a grant from DJO Global (DJO, LLC, Vista, CA, USA). The author, JCL, is a paid consultant for DJO Global and Globus Medical, and receives royalties from DJO Global and Innomed. The author, BGS, is affiliated with a research foundation that received support for this study from DJO Global and also receives additional research support from Stryker Orthopaedics, DJO Global, Arthrex, AO-North America and NIH/NIBIB. The authors NTF, NGE, ANN, and CW certify that they have no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article. No IRB was required as no human subjects were used.
Ethical standards
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
No patient data or information was used in this study.
Funding
This study was funded by a grant from DJO Global.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Formaini, N.T., Everding, N.G., Levy, J.C. et al. Glenoid baseplate fixation using hybrid configurations of locked and unlocked peripheral screws. J Orthop Traumatol 18, 221–228 (2017). https://doi.org/10.1007/s10195-016-0438-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10195-016-0438-3