Abstract
Background
This study was performed to evaluate the treatment of complex regional pain syndrome (CRPS) type I with stellate ganglion blockade.
Materials and methods
We performed three blockades at weekly intervals in 22 patients with CRPS type I in one hand. The patients were divided into two groups depending on the time between symptom onset and treatment initiation. Group 1and 2 patients had short and long symptom-onset-to-treatment intervals, respectively. Pain intensity, using a visual analog score (VAS), and range of motion (ROM) for the wrist joint were assessed before and 2 weeks after treatment and were compared using nonparametric statistical analysis.
Results
Treatment produced a statistically significant difference in wrist ROM for all patients (P < 0.001). VAS values showed an overall decrease from 8 ± 1 to 1 ± 1 following treatment, and there was a significant difference in VAS value between groups 1 and 2 (P < 0.05).
Conclusions
We concluded that stellate ganglion blockade successfully decreased VAS and increased ROM of wrist joints in patients with CRPS type I. Further, the duration between symptom onset and therapy initiation was a major factor affecting blockade success.
Similar content being viewed by others
Introduction
Complex regional pain syndrome (CRPS) was once known as reflex sympathetic dystrophy (RSD) and causalgia [1]. The International Association for the Study of Pain (IASP) suggested a new nomenclature, CRPS, with two subtypes, which deliberately avoid suggesting etiology or site [2]. CRPS type I (RSD) is defined as a syndrome that usually starts after a noxious event, is not limited to the distribution of a single peripheral nerve, and is disproportionate to the inciting event [3]. CRPS type II (causalgia) is defined as a syndrome that starts after a nerve injury and is not necessarily limited to the distribution of the injured nerve [3]. Despite these changes, CRPS has generated significant research interest [4]. One issue that continues to evolve is the role of interventional therapy in managing CRPS type I [5]. The sympathetic nervous system has been implicated in the pathophysiology of CRPS type I, and consequently, sympathetic nervous system blockade is widely used to treat CRPS type I [6]. The current view is that, when necessary, interventions administered in a timely manner may help relieve pain and facilitate the primary goal—functional rehabilitation of the affected limb [7].
Although treatment of CRPS type I with stellate ganglion block is well established, there is a limited number of prospective studies in the literature on its effectiveness. A review published by Cepeda et al. [6] revealed the scarcity of published evidence to support the use of local anesthetic sympathetic blockade as the gold standard treatment for CRPS.
The purpose of this prospective study was to evaluate the effectiveness of stellate ganglion blockade in CRPS type I in improving functional use of the affected limb and thus increase the patient’s independence at work, at leisure, and in the performance of daily activities.
Materials and methods
The study consisted of 22 patients admitted to the Orthopaedics and Traumatology Department of our hospital between 2003 and 2006 with the diagnosis of CRPS type I in one hand (Table 1). The diagnosis was based on the IASP diagnostic criteria [2, 8]. The inclusion criteria were the presence of regional pain and sensory changes following a noxious event; pain associated with findings such as abnormal skin color, temperature change, abnormal sudomotor activity or edema; no distribution of the pain of a single nerve in the extremity; the combination of these findings exceeding their expected magnitude in response to known physical damage during and following the inciting event [8]. Prior treatment with conservative therapies, such as medication, physical therapy, and rehabilitation programs, was not successful in these patients. Exclusion criteria were use of tobacco products or any medication that could affect sympathetic function, active infection at the injection site, known allergies to medications, previous neck surgeries, Raynaud’s disease or Raynaud’s phenomena, and coagulopathy. The study was approved by our Institutional Review Board, and the study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in a prior approval by our Institutional Review Board. Written informed consent was obtained from each patient.
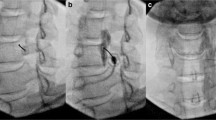
Twenty-two patients with diagnosis of CRPS type I [12 right (54.5%) and ten left (45.5%)] were included. Thirteen patients were women (59.1%) and nine (41.9%) were men. Mean patient age was 50.7 ± 15.0 (range 18–70) years, 59.3 ± 22.3 (range 27–85) years, and 54.6 ± 18.7 (range 18–85) years for men, women, and all patients, respectively. Plain radiographic changes were cortical thinning, cortical bone loss, and patchy osteopenia. The conditions associated with development of CRPS type I included eight distal radius fractures (four were surgically treated), four soft tissue tumor excisions, and four carpal tunnel syndrome surgery. Three patients had soft tissue hand trauma due, respectively, to fifth metacarpal fracture, crush injury to the hand, and surgery for Dupuytren’s disease.
Patients were assessed by clinical examination and radiography prior to treatment initiation and at the posttreatment follow-up, which was 2 weeks after the final stellate ganglion blockade. They were divided into two groups according to the latency from symptom onset and stellate ganglion block initiation (28 weeks as the threshold). Group 1 (14 patients) and group 2 (eight patients) had a short and a long mean duration between symptom onset and treatment, respectively. The mean times from symptom onset to treatment initiation were 17.0 ± 6.3 (range 6–28) weeks, 49.8 ± 17.6 (range 29–77) weeks, and 28.9 ± 19.7 (range 6–77) weeks for group 1, group 2, and all patients, respectively. Patients were not allowed to take any medication. Patients’ mean ages were 54.9 ± 20.6 (range 18–85) years and 54.0 ± 16.2 (range 29–75) years for groups 1 and 2, respectively.
Stellate ganglion blockade was performed three times with an interval of 1 week between treatments. The procedure used the anterior paratracheal approach on the cervical sympathetic chain without fluoroscopic guidance [9, 10]. A 22-gauge, 5-cm needle was inserted perpendicular to the skin until bone contact was made and then withdrawn to rest anteriorly to the precervical fascia. A volume of 15 ml of equal parts 0.5% bupivacaine (5 mg/ml) and 1% prilocaine–hydrochloride (HCl) (20 mg/ml) was used. After injection of a 0.5-ml test dose to exclude intravascular positioning, the remainder of the appropriate dose was administered. The patient was encouraged to lie flat for 3 min after the injection and then to sit up.
Pain intensity was evaluated before and 2 weeks after the last of three stellate ganglion blockades using a 10-cm visual analog scale (VAS) in which 0 represented no pain and 10 represented the most severe pain. The range of flexion, extension, supination, and pronation of each patient’s wrist joint was also recorded. Patients were asked to perform simple range of motion (ROM) exercises during the blockades. These consisted mainly of active and active-assisted passive exercises on the wrist joint. After the follow-up examination performed 2 weeks after the last stellate ganglion blockade, passive exercises along with a rehabilitation program were started.
Statistical analysis
Statistical analysis was performed with Statistical Package for Social Sciences 11.0 (SPSS 11.0, SPSS Inc., Chicago IL, USA). The Wilcoxon signed-rank test was used to compare wrist-joint ROM values before and 2 weeks after the last blockade and to compare VAS values before and 2 weeks after the last blockade for all patients and for each group. The Mann–Whitney U test was used for between-group comparisons of mean VAS values. P < 0.05 was taken to indicate statistical significance.
Results
Values pretreatment and 2 weeks postblockade ROM are shown in Table 2. The blockade produced significant changes in ROM values for wrist flexion, extension, supination, and pronation in all patients (P < 0.001). Wrist flexion and extension improved from 50° ± 14° to 69° ± 8° and from 39° ± 13° to 59° ± 8°, respectively. Supination and pronation improved from 41° ± 12° to 63° ± 8° and from 50° ± 13° to 69° ± 8°, respectively.
Pretreatment and 2 weeks postblockade VAS results for both groups are presented in Table 3. Overall VAS decreased from 8 ± 1 to 1 ± 1 following stellate ganglion blockade.
There was no significant difference in baseline VAS value between groups (P > 0.05). Blockade significantly improved VAS values in all patients and in both treatment groups (P < 0.05); however, there was a significant difference in postblockade VAS value between groups 1and 2 (P < 0.05). No adverse effects to medications administered or the procedure itself were documented during the procedure or follow-up.
Discussion
Invasive procedures, including nerve blocks, spinal cord and peripheral nerve stimulation, chemical and surgical sympathectomies, and deep brain stimulation have been used to manage CRPS type I for some time [4]. Sympathetic nervous system dysfunction is presumed to be an essential component of the syndrome [11], and sympathetic blockade has been recommended as early as possible to interrupt and reverse the process [12]. The primary goal of this study was to evaluate the effects of stellate ganglion blockade treatment on CRPS type I. Treatment produced a statistically significant difference in wrist ROM for all patients (P < 0.001). VAS values showed an overall decrease from 8 ± 1 to 1 ± 1 following treatment, and there was a significant difference in VAS value between groups 1 and 2 (P < 0.05), showing that there is a direct relationship between symptom onset and treatment initiation. Mean VAS reduction was 7 ± 1 (range 5–9), 6 ± 2 (range 3–9), and 7 ± 2 (range 3–9) in groups 1 and 2 and overall, respectively.
This study was limited by a relatively small sample size and a wide range of conditions causing CRPS type I. However, as demonstrated in previous studies [13–15], large sample sizes and even distribution of etiologies are difficult to achieve. Another weakness of the study was the lack of long-term results of the blockades.
There is limited number of studies of stellate ganglion blockade in the literature. Cepeda et al. [6, 14] published two reviews. In 2002, they concluded that there are questions as to the efficacy of local anesthetic sympathetic blockade in treating CRPS because its efficacy is based mainly on case series [14]. Later in 2005, Cepeda et al. [6] published a review that attempted to determine the likelihood of pain alleviation after sympathetic blockade with local anesthetics in the patient with CRPS, to assess how long any benefit persists, and to evaluate the incidence of adverse effects. They searched the Cochrane Pain, Palliative and Supportive Care Register, the Cochrane Central Register of Controlled Trials, Medline, EMBASE, LILACS, conference abstracts of the World Congresses of the International Association for the Study of Pain, and bibliographies from retrieved articles for randomized controlled trials that evaluated the effect of sympathetic blockade with local anesthetics in children or adults to treat RSD, causalgia, or CRPS. They found only two small randomized double-blind studies that evaluated 23 patients across both studies. The combined effect of the two trials produced a relative risk (RR) to achieve at least 50% of pain relief 30 min to 2 h after the sympathetic blockade of 1.17 [95% confidence interval (CI) 0.80–1.72]. They stated that it was not possible to determine the effect of sympathetic blockade on long-term pain relief because the authors of the two studies evaluated different outcomes. They concluded that the study revealed a scarcity of published evidence to support the use of local anesthetic sympathetic blockade as the gold standard treatment for CRPS. Also, the two randomized studies that met inclusion criteria had very small sample sizes. Therefore, no conclusion concerning the effectiveness of this procedure could be drawn, and there is a need to conduct randomized controlled trials to address the value of sympathetic blockade with local anesthetic for the treatment of CRPS.
Another review was published recently by Albazaz et al. [18] in 2008. They stated that the review gives a synopsis of CRPS and discusses the principles of management based on the limited available literature on the subject. They performed a literature search using electronic bibliographic databases (Medline, EMBASE, PubMed Central) from 1970 to 2006 with the keywords: complex regional pain syndrome, reflex sympathetic dystrophy, neuropathic pain, and causalgia. Relevant articles from the reference lists in retrieved articles were also studied. There were 3,771 articles. Of the 76 randomized controlled trials that were identified, most were on the role of sympathetic blockade in the treatment of CRPS (n = 13). In other studies, nine were on bisphosphonates or calcitonin; four were on cognitive behavioral therapy, physiotherapy, or occupational therapy; three were on spinal cord stimulation; and two each on acupuncture, vitamin C, and steroids. The remaining studies were on miscellaneous therapy or combination therapy, making it difficult to draw any conclusions on treatment effect. There was very little good evidence in the literature to guide treatment of CRPS. The authors concluded that early recognition and a multidisciplinary approach to management seems important in obtaining a good outcome.
We found that the duration between the symptom onset and therapy initiation played a major role in blockade success. Similar to this study, in a prospective study of 25 patients who had carpal tunnel release, Ackerman and Zhang [19] found that stellate ganglion blockade was significantly more effective in relieving pain associated with CRPS type I when administered shortly after symptom onset. They concluded that the treatment was less effective when administered >16 weeks after symptom onset.
Seventy-one patients with reflex sympathetic dystrophy of the lower extremities were studied over a 3-year period. Of the 27 patients managed by conservative means, 11 (41%) showed signs of improvement, whereas of the 43 patients treated by sympathetic nerve blocks, 28 (65%) experienced progress. The authors concluded that early treatment with repeated sympathetic nerve blocks appears to improve the long-term outcome [17]. Yokono et al. [20] correlated the changes in three phase bone scintigraphy (TPBS) with prognosis after sympathetic blockade in RSD of the hand in 12 patients. They compared scintigraphy obtained just before and after this series of sympathetic blocks and evaluated the eventual recovery of hand function. In eight patients, blood flow (phase 1) image of TPBS decreased after the blockade. But others with normalized blood flow remained with mild hand contracture. These results suggest that normalization of blood pool and delayed image on scintigraphy is a predictor of subsequent recovery after sympathetic blockade in RSD. Schürmann et al. [16] evaluated the results of stellate ganglion blockade in 33 patients in CRPS type I. They report that mean pain reduction was 2.3 points on the VAS. Seventeen patients (51.5) experienced a reduction ≤50% of initial pain, no significant pain relief was observed in 13 patients (39.4%), and three patients (9.1%) had no pain before the blockade. These findings are contrary to our study, in which we found a mean VAS reduction of 7 ± 2 (range 3–9) overall. The reason for this maybe the injection technique or patient characteristics.
We report that stellate ganglion blockade successfully relieved pain in patients with CRPS type I as indicated by a significant reduction in VAS values for all patients following the block (P < 0.05). Price et al. [21] analyzed the results of sympathetic ganglion block in seven patients. They reported that local injection of an anesthetic produced large reductions in pain intensity in six patients and concluded that both magnitude and duration of pain reduction should be closely monitored to provide optimal efficacy in procedures that use local anesthetics to treat CRPS. Bonelli et al. [13], in a randomized trial of reflex sympathetic dystrophy, found that the performance of intravenous guanethidine block is of longer duration, and superior to stellate ganglion block as regards some early pharmacological effects. However, their patients exhibited severe reflex sympathetic dystrophy following peripheral nerve lesions, and thus all belonged to CRPS type II.
Sympathetic block treatment may be particularly helpful in cases in which, despite adequate doses of oral medication, pain limits a patient’s participation in physical and occupational therapy [7]. Treatments aimed at pain reduction and rehabilitation of limb function form the mainstay of therapy [18]. In this study, stellate ganglion blockade significantly improved ROM values for wrist flexion, extension, supination, and pronation in all patients (P < 0.001). The treatment effectively cut the vicious cycle of pain, immobilization, decreased joint motion, and pain.
We concluded that treating CRPS type I with stellate ganglion blockade successfully decreased VAS values and increased wrist-joint ROM. We are of the opinion that our study focuses on a district anatomical region and gives evidence to guide treatment of CRPS type I, especially in the hand and wrist. The duration between symptom onset and therapy initiation was a major factor affecting the success of the blockade. If other treatment modalities fail, stellate ganglion blockade should be performed as early as possible.
References
Rowbotham MC (2006) Pharmacologic management of complex regional pain syndrome. Clin J Pain 22:425–429
Merskey H, Bogduk N (1994) Classification of chronic pain. Seattle, IASP, pp 40–43
Kingery WS (1997) A critical review of controlled clinical trials for peripheral neuropathic pain and complex regional pain syndromes. Pain 73:123–139
Wilson PR, Stanton-Hicks M, Harden RN (eds) (2005) CRPS: current diagnosis and therapy. IASP, Seattle, pp 45–58
Nelson DV, Stacey BR (2006) Interventional therapies in the management of complex regional pain syndrome. Clin J Pain 22:438–442
Cepeda MS, Carr DB, Lau J (2005) Local anesthetic sympathetic blockade for complex regional pain syndrome. Cochrane Database Syst Rev 19:CD004598
Stanton-Hicks MD, Burton AW, Bruehl SP, Carr DB, Harden RN, Hassenbusch SJ et al (2002) An updated interdisciplinary clinical pathway for CRPS: report of an expert panel. Pain Pract 2:1–16
Stanton-Hicks M, Jänig W, Hassenbusch S, Haddox JD, Boas R, Wilson P (1995) Reflex sympathetic dystrophy: changing concepts and taxonomy. Pain 63:127–133
Dunningham TH (1980) The treatment of Sudeck’s atrophy in the upper limb by sympathetic blockade. Injury 12:139–144
Hempel V (1993) The stellate ganglion blockade. Anaesthesist 42:119–128
Schwartzman RJ, McLellan TL (1987) Reflex sympathetic dystrophy. A review. Arch Neurol 44:555–561
Bonica JJ (1990) Causalgia and other reflex sympathetic dystrophies. In: Bonica JJ, Loeser JD, Chapman CR, Fordyce WE (eds) The management of pain, vol 1, 2nd edn. Lea & Febiger London, Philadelphia, pp 220–243
Bonelli S, Conoscente F, Movilia PG, Restelli L, Francucci B, Grossi E (1983) Regional intravenous guanethidine vs. stellate ganglion block in reflex sympathetic dystrophies: a randomized. Pain 16:297–307
Cepeda MS, Lau J, Carr DB (2002) Defining the therapeutic role of local anesthetic sympathetic blockade in complex regional pain syndrome: a narrative and systematic review. Clin J Pain 18:216–233
Malmqvist EL, Bengtsson M, Sörensen J (1992) Efficacy of stellate ganglion block: a clinical study with bupivacaine. Reg Anesth 17:340–347
Schürmann M, Gradl G, Wizgal I, Tutic M, Moser C, Azad S et al (2001) Clinical and physiologic evaluation of stellate ganglion blockade for complex regional pain syndrome type I. Clin J Pain 17:94–100
Wang JK, Johnson KA, Ilstrup DM (1985) Sympathetic blocks for reflex sympathetic dystrophy. Pain 23:13–17
Albazaz R, Wong YT, Homer-Vanniasinkam S (2008) Complex regional pain syndrome: a review. Ann Vasc Surg 22:297–306
Ackerman WE, Zhang JM (2006) Efficacy of stellate ganglion blockade for the management of type 1 complex regional pain syndrome. South Med J 99:1084–1088
Yokono A, Yokono S, Ogli K (1990) Relationship between three phase bone scintigram and prognosis after sympathetic blockade in reflex sympathetic dystrophy of the hand. Masui 39:1496–1502
Price DD, Long S, Wilsey B, Rafii A (1998) Analysis of peak magnitude and duration of analgesia produced by local anesthetics injected into sympathetic ganglia of complex regional pain syndrome patients. Clin J Pain 14:216–226
Conflict of interest statement
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Yucel, I., Demiraran, Y., Ozturan, K. et al. Complex regional pain syndrome type I: efficacy of stellate ganglion blockade. J Orthopaed Traumatol 10, 179–183 (2009). https://doi.org/10.1007/s10195-009-0071-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10195-009-0071-5