Abstract
Purpose
The aim of this study is to investigate the reliability and validity of the Japanese version of the modified American College of Rheumatology (ACR) Preliminary Diagnostic Criteria for Fibromyalgia (mACR 2010-J) and the Fibromyalgia Symptom Scale (mFS-J).
Methods
According to the ACR 1990 classification criteria, patients with chronic pain were divided into the fibromyalgia group and nonfibromyalgia group (rheumatoid arthritis and osteoarthritis). Patients in both groups were assessed using mACR 2010-J and mFS-J.
Results
294 of 462 (64 %) patients in the fibromyalgia group met mACR 2010-J, whereas 4 % (9/231) of the nonfibromyalgia group did, with sensitivity of 64 %, specificity of 96 %, positive predictive value of 97 %, negative predictive value of 56 %, and positive likelihood ratio of 16.3. Mean total scores on mFS-J significantly differentiated the fibromyalgia from the nonfibromyalgia group. According to the value of the Youden index, the best cutoff score for the mFS-J was 9/10.
Conclusion
Our findings indicate that mACR 2010-J as a positive test and mFS-J as a quantification scale might be suitable for assessing fibromyalgia among Japanese chronic pain populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
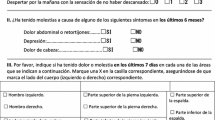
Fibromyalgia (FM) is characterized by widespread musculoskeletal chronic pain, fatigue, poor sleep, frequent psychological difficulties, and multiple tender points on physical examination [1, 2]. In 1990, the American College of Rheumatology (ACR) presented FM criteria (ACR 1990) that required tenderness on pressure (tender points) in at least 11 of 18 specified sites and the presence of widespread pain for diagnosis [1]. Widespread pain was defined as axial pain, both left- and right-sided and with upper and lower segment pain. However, ACR 1990 had the serious problem of little variation in symptoms. To improve this shortcoming, new clinical criteria, which integrate variations in symptoms with severity scale (2010 ACR Preliminary Diagnostic Criteria for FM, ACR 2010) [3], have been presented. The diagnostic criteria for FM are satisfied if the following three conditions are met: (1) Widespread Pain Index (WPI) ≥7 and Symptom Severity Score (SS) ≥5, or WPI of 3–6 and SS ≥9; (2) symptoms have been present at a similar level for at least 3 months; and (3) the patient does not have a disorder that would otherwise explain the pain. The publication of ACR 2010 eliminated the tender point examination, thus making it possible to study FM in survey and clinical research.
Accordingly, we have validated the Japanese version of ACR 2010 [4]. In addition, we have originally validated the Japanese version of the Fibromyalgia Symptom Scale with the sum of WPI and the original SS, i.e., fatigue, waking unrefreshed, cognitive symptoms, and somatic symptoms in general consisting of 41 symptoms of the FS-J [4]. Both ACR 2010-J and FS-J have high reliability and validity, and are useful for assessing fibromyalgia among Japanese chronic pain populations.
Recently, Wolfe et al. [5] proposed a modification of the ACR 2010 (mACR 2010), deleting 38 out of 41 somatic symptoms in general from the original SS. Consequently, complete self-administration has become possible. Furthermore, they created the Fibromyalgia Symptom Scale with the sum of WPI and the new SS (FS). They reported that the criteria properly identified diagnostic groups, and that FS score ≥13 best separated criteria+ and criteria− patients.
The aim of this study is to investigate the reliability and validity of the Japanese version of the mACR 2010 (mACR 2010-J) and the Japanese version of the FS (mFS-J). Furthermore, our questions are whether mACR 2010-J would be more useful than ACR 2010-J for assessing fibromyalgia among Japanese chronic pain populations, and whether mFS-J is more suitable than FS-J as a positive test.
Subjects and methods
An experienced rheumatologist and an experienced psychiatrist had translated the mACR 2010 into Japanese with the author’s permission and produced forward- and back-translations to create the mACR 2010-J.
We recruited FM patients who met the previous criteria of the ACR 1990 and were without psychiatric disorders according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) [6] in a clinic specialized for FM, the Kasumigaseki Urban Clinic, in Tokyo, Japan, between August 1, 2010 and July 31, 2011. During the study period, other patients with diseases associated with chronic pain such as rheumatoid arthritis (RA) and osteoarthritis (OA) who had not been diagnosed previously with FM were recruited as control patients. To adjust the imbalance of number of patients, control patients were additionally recruited from May 30 to July 2, 2012. The diagnoses of RA and OA were made according to the 2010 rheumatoid arthritis classification criteria [7] and the American College of Rheumatology criteria for classification and reporting of osteoarthritis of the hand, hip, and knee [8–10]. The experienced rheumatologist and the experienced psychiatrist familiar with FM assessed these patients. This study was approved by the Institutional Review Board of Kasumigaseki Urban Clinic.
After obtaining informed consent from study participants, the rheumatologist rated patients with the mACR 2010-J. In order to assess interrater reliability, another rater independently rated a subset of the same subjects (N = 19) while blind to the diagnoses and scores of the other rater. The raters in this study were already fully trained in use of the scale and quite experienced in use of it. We therefore decided that only a small subsample was needed to reevaluate consistency across raters.
Statistics
Data were analyzed using SPSS 17.0-J software. Differences among groups in demographic and clinical characteristics were calculated with the unpaired t test. If data were not sampled from Gaussian distributions, a nonparametric test (Mann–Whitney U test) was used. To compare categorical data, we used Fisher’s exact test.
In the present study, the control group was not healthy volunteer but consisted of chronic pain patients with RA and OA. It has been reported that the age-specific incidence of RA peaked in the 60–64 and 70–74 year age groups for females and males, respectively, in Taiwan [11]. Similarly, it has been reported that the peak prevalence of knee OA in women and men was ≥80 years in Japan [12]. In contrast, we have reported that the frequent age of onset of FM in women was 35–55 years based on our FM database including 3,500 Japanese patients with FM [13]. Among Asians, thus, patients with FM are much younger than those with RA and OA. Therefore, matching age of control patients with age of FM patients seems to be rather arbitrary. Accordingly, to control for the effect of age on the rate of patients meeting the mACR 2010-J, patients were divided into three age categories, i.e., 20–39, 40–59, and ≥60 years. There were only eight FM patients and one non-FM patients less than 20 years of age, and there were only two FM patients and three non-FM patients 80 years or older. Then, the Mantel–Haenszel method was used to test the difference in the percentage of patients meeting the mACR 2010-J between the two groups. Also, to control for the effect of age on the score on the mFM-J, one-way analysis of covariance was used. The internal consistency for the mFM-J was calculated with Cronbach’s α. Interrater reliability was measured with the intraclass correlation coefficient (ICC) for pairs of independent raters. Cutoff scores for the mFS-J were determined using receiver-operator characteristic (ROC) analyses to determine the Youden index when comparing the FM group with all non-FM subjects. Positive predictive value (PPV), negative predictive value (NPV), and positive likelihood ratio (sensitivity/1 − specificity) were also calculated. All statistical tests were two-tailed. Statistical significance was set at p < 0.05.
Results
A total of 462 patients meeting the ACR 1990 (the FM group) and a total of 231 non-FM patients (RA patients, 196; OA patients, 35; the non-FM group) were enrolled. Demographic and clinical characteristics of the groups are presented in Table 1, showing that 294 of 462 (64 %) patients in the FM group met the mACR 2010-J, whereas 4 % (9/231) of the non-FM group did, including 4 % (8/196) of RA patients and 3 % (1/35) of OA patients. The percentage of patients meeting the mACR 2010-J criteria in the FM group was significantly higher than that of the non-FM group after adjusting for age (estimated odds ratio, 35.7, p < 0.0001; Table 1). The sensitivity, specificity, PPV, NPV, and positive likelihood ratio for comparison of the FM group with all non-FM subjects were 64, 96, 97, 56, and 16.3 %, respectively. The ICC between the two independent raters was very high for the mACR 2010-J, at 0.877.
The mean score (standard deviation, SD) of mFS-J in the FM group was 16.7 (6.5), while that in the non-FM group was 3.7 (4.1). The mean score of mFS-J in the FM group was significantly higher than that of the non-FM group after adjusting for age (F = 605.1, p < 0.0001; Table 1). Internal consistency was not high, with a Cronbach’s α coefficient for the mFS-J (WPI + the modified SS) of 0.603. ROC analyses were performed for the mFS-J, comparing the FM group with the non-FM group. Table 2 shows the sensitivity, specificity, positive likelihood ratio, and Youden index for ROC analysis at various cutoff scores for the mFS-J. According to the value of the Youden index, the best cutoff score for the mFS-J was 9/10.
Discussion
This is the first study to validate the mACR 2010-J and mFS-J, which is the quantification scale of the mACR 2010-J. The positive likelihood ratio of 16.3 for the mACR 2010-J is sufficiently high as a positive test. We cannot directly compare the likelihood ratios for the mACR 2010-J and the ACR 2010-J, as the present study group is quite different from that used in the study of the ACR 2010-J [4]. However, the value of mACR 2010-J is sufficiently high compared with that of ACR 2010-J, for which the positive likelihood ratio was 8.8. Therefore, the modification of ACR 2010-J may be superior to the original ACR 2010-J as a positive test.
The best cutoff score for the mFS-J was 10, which is just the same as the FS-J [4]. Furthermore, the positive likelihood ratio for the mFS-J (Table 2) is as high as that for the FS-J at the cutoff score [4]. As the mFS-J is simpler than the FS-J, mFS-J may be superior to FS-J based on the original ACR 2010-J as a quantification scale. Meanwhile, the best cutoff score of 10 in the present study is smaller than that of the original study on the FS performed in the USA (cutoff score 13) [5]. One explanation for this difference is in patient characteristics. In the present study, comorbid psychiatric disorders were excluded, while in the previous study they were not. Patients with major depressive disorder, panic disorder, or anxiety disorder usually have somatic symptoms similar to those of ACR 2010, and comorbidity of major depressive disorder, panic disorder, or anxiety disorder is not rare [1]. Therefore, the population in the previous study may have been modified by comorbid psychiatric disorders. Thus, the cutoff score of 10 in the present study might reflect fibromyalgia itself more than that of 13 in the previous study. Another possible explanation is cross-cultural differences in expression or rating of symptoms.
The internal consistency with a Cronbach’s α coefficient for the mFS-J (WPI + the modified SS) of 0.603 is lower than that for the FS-J (WPI + the original SS) of 0.747 [4]. The modified SS consists of fatigue, waking unrefreshed, cognitive symptoms, plus having pain/cramps in the abdomen, depression, and headache, resulting from 38 somatic symptoms in general having been deleted from the original SS. Therefore, the modified SS values neuropsychiatric symptoms more than the original SS. In contrast, WPI is the number of pain areas, which is simply somatic. Accordingly, the internal consistency for the mFS-J (WPI + the modified SS) might have been lower than that for the FS-J (WPI + the original SS). As FM shows a variety of symptoms and is suspected of involving not only musculoskeletal but also central nervous system [14], the not so high value of internal consistency for the mFS-J may not necessarily be a shortcoming.
Thus, mACR 2010-J as a positive test and mFS-J as a quantification scale might be suitable for assessing fibromyalgia among Japanese chronic pain populations. A strength of the present study is that the findings represent real clinical practice in Japan, since the study was performed in a clinic specialized in FM which is visited by the largest number of FM patients in Japan. A limitation of this study is that the findings may not be applicable to all patients, since FM patients with other musculoskeletal diseases, such as spondylitis, were not included in it. Further studies with patients of other countries or ethnicities will be needed to determine cross-cultural or ethnic differences in expression or rating of symptoms.
References
Wolfe F, Smythe HA, Yunus MB, Bennett RM, Bombardier C, Goldenberg DL, et al. The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Report of the Multicenter Criteria Committee. Arthr Rheum. 1990;33(2):160–72.
Wolfe F, Ross K, Anderson J, Russell IJ, Hebert L. The prevalence and characteristics of fibromyalgia in the general population. Arthr Rheum. 1995;38(1):19–28.
Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Katz RS, Mease P, et al. The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res (Hoboken). 2010;62(5):600–10.
Usui C, Hatta K, Aratani S, Yagishita N, Nishioka K, Kanazawa T, et al. The Japanese version of the 2010 American College of Rheumatology Preliminary Diagnostic Criteria for Fibromyalgia and the Fibromyalgia Symptom Scale: reliability and validity. Mod Rheumatol. 2012;22(1):40–4.
Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Hauser W, Katz RS, et al. Fibromyalgia criteria and severity scales for clinical and epidemiological studies: a modification of the ACR Preliminary Diagnostic Criteria for Fibromyalgia. J Rheumatol. 2011;38(6):1113–22.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, D.C.: American Psychiatric Association; 1996.
Aletaha D, Neogi T, Silman AJ, Funovits J, Felson DT, Bingham CO 3rd, et al. Rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Ann Rheum Dis. 2010;69(9):1580–8.
Altman R, Asch E, Bloch D, Bole G, Borenstein D, Brandt K, et al. Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthr Rheum. 1986;29(8):1039–49.
Altman R, Alarcon G, Appelrouth D, Bloch D, Borenstein D, Brandt K, et al. The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hip. Arthr Rheum. 1991;34(5):505–14.
Altman R, Alarcon G, Appelrouth D, Bloch D, Borenstein D, Brandt K, et al. The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hand. Arthr Rheum. 1990;33(11):1601–10.
Lai CH, Lai MS, Lai KL, Chen HH, Chiu YM. Nationwide population-based epidemiologic study of rheumatoid arthritis in Taiwan. Clin Exp Rheumatol. 2012;30(3):358–63.
Yoshimura N, Muraki S, Oka H, Mabuchi A, En-Yo Y, Yoshida M, et al. Prevalence of knee osteoarthritis, lumbar spondylosis, and osteoporosis in Japanese men and women: the research on osteoarthritis/osteoporosis against disability study. J Bone Miner Metab. 2009;27(5):620–8.
Nishioka K. Present condition and problems in fibromyalgia. Nihon Naika Gakkai Zasshi. 2007;96(10):2235–40.
Usui C, Hatta K, Doi N, Nakanishi A, Nakamura H, Nishioka K, et al. Brain perfusion in fibromyalgia patients and its differences between responders and poor responders to gabapentin. Arthr Res Ther. 2010;12(2):R64.
Acknowledgments
This work was supported in part by grants from the Ministry of Health, Welfare, and Labor of Japan and the Japan Rheumatology Foundation and by a Grant-in-Aid for Young Scientists B (22791142) from the Japan Society for the Promotion of Science.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Usui, C., Hatta, K., Aratani, S. et al. The Japanese version of the modified ACR Preliminary Diagnostic Criteria for Fibromyalgia and the Fibromyalgia Symptom Scale: reliability and validity. Mod Rheumatol 23, 846–850 (2013). https://doi.org/10.1007/s10165-012-0759-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10165-012-0759-x