Abstract
Application of biological agents targeting inflammatory cytokines such as tumor necrosis factor-α (TNF-α) dramatically caused a paradigm shift in the treatment of rheumatoid arthritis (RA). Infliximab, a chimeric anti-TNF-α monoclonal antibody, has initially been introduced to Japan in 2003 and shown to be dramatically effective in alleviating arthritis refractory to conventional treatment. However, serious adverse events such as bacterial pneumonia, tuberculosis, and Pneumocystis jiroveci pneumonia were reported to be in relatively high incidence; i.e., 2%, 0.3%, and 0.4%, respectively, in a strict postmarketing surveillance of an initial 4000 cases in Japan. Etancercept, a recombinant chimeric protein consisting of p75 TNF-α receptor and human IgG, was subsequently introduced to Japan in March of 2005. We therefore drew up treatment guidelines for the use of etanercept to avoid potential serous adverse events, since only approximately 150 cases have been included in the clinical study of etanercept in Japan. The guidelines were initially designed by the principal investigators (N.M, T.T., K.E.) of rheumatoid arthritis study groups of the Ministry of Health, Labor and Welfare (MHLW), Japan, and finally approved by the board of directors of the Japan College of Rheumatology. The MHLW assigned a duty to the pharmaceutical companies to perform a complete postmarketing surveillance of an initial 3000 cases to explore any adverse events, and this was performed according to the treatment guidelines shown in this article.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent years, there has been a paradigm shift in the treatment of rheumatoid arthritis (RA). It is mostly attributed to the introduction of biological agents targeting inflammatory cytokines. Biological agents have approved and marketed for the treatment of RA in Europe and the United States include anti-tumor necrosis factor-α (TNF-α) antibodies such as infliximab (Remicade) adalimumab (Humira), soluble TNF-α receptor etanercept (Enbrel), and interleukin (IL)-1 receptor antagonist anakinra (Kineret). Among these, etanercept has drawn particular attention as a highly effective and safe biological product in the treatment of RA; it was approved in January 2005 in Japan.
Efficacy and adverse events of etanercept
Etanercept is a recombinant chimeric protein consisting of two molecules of p75 and the Fc portion of human IgG1 and is produced by introducing the fusion gene into Chinese hamster ovary cells (molecular weight, approximately 150kDa; total amino acid residues, 934). As compared with the natural-occurring soluble TNF-α receptor, etanercept showed 50-fold greater binding to TNF-α, 100- to 1000-fold greater biological activity, and 5- to 8-fold longer plasma half-life; therefore, treatment of RA with etanercept has been conducted.1
In a phase III study in the United States involving 234 patients with active RA who were resistant to disease-modifying antirheumatic drugs (DMARDs) including methotrexate (MTX), treatment with etanercept 25mg showed significantly greater efficacy than etanercept 10mg or placebo.1 Analysis of adverse events revealed that the incidence of injection-site reactions was significantly higher in the 25-mg dose group than other dose groups and that the active treatment groups had a higher incidence of infections, i.e., upper respiratory tract infections, than the placebo group.
In a double-blind study of concomitant MTX, 89 patients with active RA who had been treated with MTX for at least 6 months received either etanercept 25 mg or placebo twice a week subcutaneously in addition to MTX, resulting in improvement in a 20% American College of Rheumatology (ACR 20) response in 71% of patients receiving etanercept and an ACR 50 improvement in 39% of patients receiving etanercept. Moreover, there were no significant differences in incidence of adverse events such as infections between the two groups.2
On the basis of these results, etanercept was approved as a treatment for RA by the Federal Drug Administration (FDA) in the United States in November 1998. More than 6 years after its approval in the United States, the drug was approved in January 2005 and has been marketed since the end of March 2005 in Japan.
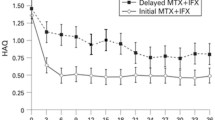
The most significant benefit of etanercept is to inhibit the progression of joint destruction. Its efficacy has been demonstrated to be far superior to that of MTX, which is known to have the potent effect of slowing the progression of joint destruction.3 The remarkable effectiveness of etanercept has been shown particularly in the recently reported TEMPO (Trial of Etanercept and Methotrexate with Radiographic Patient Outcomes).4 In this trial, 686 patients with RA who were resistant to one or more DMARDs other than MTX received one of the following three treatments for 2 years: MTX alone, etanercept alone, or etanercept plus MTX. The primary efficacy endpoint was the numeric index of the ACR response (ACR-N) area under the curve (ACR-AUC) over the first 24 weeks. The primary endpoint did not differ significantly between the MTX monotherapy group and etanercept monotherapy group; however, the etanercept plus MTX group had significantly higher ACR-AUC values than the two monotherapy groups. The proportion of patients achieving ACR 50, a clinically meaningful efficacy, at 2 years was 71% in the etanercept plus MTX group as compared with 42% in the MTX monotherapy group and 54% in the etanercept group, indicating greater efficacy of the combination of etanercept and MTX. Moreover, the change in total Sharp Score at 1 year of treatment was −0.54 in the etanercept plus MTX group as compared with +2.8 in the MTX monotherapy group and +0.52 in the etanercept group, suggesting the possibility that the combination may inhibit the progression of joint destruction and even heal the condition.
Frequently observed adverse events include injectionsite reactions, which are characterized by erythema with pruritus, swelling, or pain at the injection sites. Most reactions disappear with only topical treatments such as antihistamines.
The most careful attention should be given to monitoring for infections. Among the more than 1100 patients receiving long-term treatment for at least 6 months, 50 experienced serious infections such as pyelonephritis, bronchitis, septic arthritis, and abscess formation, which were caused by various types of organisms including bacteria, fungi, and Pneumocystis jiroveci. Etanercept may mask clinical symptoms characteristic of infections, such as fever and chills, and inhibit the production of acute inflammatory proteins, thereby causing the problem of difficulty in detecting infections at an early stage.
In addition, occurrence of tuberculosis has recently been of particular concern, although etanercept appears to be rarely associated with tuberculosis as compared with infliximab.5,6 However, caution should be exercised when etanercept is used in Japan, where tuberculosis frequently occurs,7 because BCG vaccinations in Japan preclude the use of the tuberculin skin test for screening at the start of drug treatment, and there are not a few patients with drugresistant Mycobacterium tuberculosis.8,9
Although the occurrence of malignancies was the most serious among possible complications, the incidence in the more than 1100 patients was not significantly different from the expected incidence in the general population. Also, patients with active RA have been shown to have a slightly higher incidence of malignant lymphoma. In March 2003, the FDA reported that the standardized incidence ratio (SIR) for malignant lymphoma ranged from 2.3 to 3.5 in patients receiving etanercept with no statistically significant difference.10
Because etanercept is known to exacerbate congestive heart failure, caution should be made when etanercept is administered to patients with heart failure. Initially, clinical trials were conducted with infliximab or etanercept as a therapeutic agent for congestive heart failure because TNF-α was believed to be involved in the pathophysiology of congestive heart failure. However, individual clinical trials showed treatment failures and even worsening cases of congestive heart failure, leading to termination of these trials.11
In addition, rare cases of pancytopenia have been reported. Although demyelinating diseases in the central nervous system have also been reported, a causal relationship to the treatment remains uncertain. In some patients with multiple sclerosis, an increase in disease activity has been found after the treatment.12 A recent report showed that etanercept treatment in early RA patients was well tolerated for up to 5 years.13
In Japan, 147 patients who were refractory to conventional DMARDs were enrolled in phase II clinical study. Patients were randomly divided into three groups, i.e., placebo group, 10mg twice-weekly group, and 25mg twice-weekly group, and treated for 12 weeks. Consequently, both the 10mg group and 25mg group yielded an almost identical ACR20 response, significantly better than the placebo group (64.0%, 65.3% vs. 6.3%, respectively). This trend was similar in both ACR50 and ACR70 response. There was no significant difference observed in severe adverse effects between the etanercept and placebo groups.
Treatment guidelines for the use of etanercept (Table 1)14
For the safe use of etanercept in Japan, which produces such high efficacy and potential adverse events, the internal medicine rheumatology study group of the Ministry of Health, Labor and Welfare, Japan (led by N.M., T.T., and K.E.) has developed the guidelines for treatment with etanercept, which provide indications, contraindications, and tuberculosis risk assessment, which was based on the guidelines for the use of infliximab for RA patients in Japan9 (Fig. 1). The guidelines were approved by the board of directors of Japan College of Rheumatology.
Etanercept is indicated in patients with active RA at or above a certain level. Specifically, etanercept may be used in patients who have inadequately been controlled despite treatment of at least 3 months with the usual doses of one of the DMARDs (methotrexate, bucillamine, or sulfasalazine), which are rated as “recommendation A level” in the Diagnostic Manual and Evidence-based Treatment Guidelines15 developed by the study group of the Ministry of Health, Labor and Welfare. Leflunomide, another DMARD rated as recommendation A, is not included in the present guidelines because of the adverse event of serious interstitial pneumonia observed in Japan.16 Inadequate response to previous treatment is defined by the presence of at least six tender joints and swollen joints and either C-reactive protein levels of at least 2.0 mg/dl or erythrocyte sedimentation rate (ESR) of at least 28mm/h.
To avoid potential opportunistic infections, patients should have a peripheral leukocyte count of 4000/mm3 or more, peripheral lymphocyte count of 1000/mm3 or more, and a negative test for blood β-d-glucan. These criteria are based on the findings that cellular immunity plays an important role in opportunistic infections caused by Mycobacterium tuberculosis or fungi such as Pneumocystis jiroveci, and that these infections are likely to occur in patients with decreased peripheral lymphocyte counts.17 A test for blood β-d-glucan has been included because β-d-glucan, a component of fungi, may be diagnostic of fungal infections, especially infections with Pneumocystis jiroveci.
The recommended dosage and administration of etanercept in Japan is 10–25 mg given once daily and twice weekly as a subcutaneous injection. In this aspect, onceweekly administration of 50mg etanercept in patients with active RA patients has been approved in the United States, and this dosing regimen was shown to be equivalent to 25 mg etanercept twice weekly in terms of safety, efficacy, and pharmacokinetics.18 Patients will switch to self-injection after they are assessed as capable of conducting self-injections and receive adequate instructions. Etanercept may be used as monotherapy as the drug was administered so in clinical trials in Japan. In Europe and the United States, however, etanercept in combination with MTX has been demonstrated to provide greater efficacy in TEMPO.4 Thus, the combination of etanercept with MTX should be considered in patients with highly active disease in Japan.
Etanercept is contraindicated in patients with active infections or a history of serious infections within the previous 6 months. In addition, careful assessment of the risk of tuberculosis should be made. Specifically, the following three examinations should be performed before treatment initiation: interview with respect to family and past history of tuberculosis, chest radiography, and purified protein derivative (PPD) skin test (Fig. 1). Chest radiographs should preferably be interpreted by a specialist in pulmonology, tuberculosis, or radiology. When abnormalities are suspected on chest radiography, computed tomography of the chest should be performed. Etanercept is contraindicated in patients with abnormalities in chest radiographs such as linear opacities, calcification ≥5mm, and pleural thickening suggesting old pulmonary tuberculosis, and individuals infected with pulmonary or extrapulmonary tuberculosis. However, treatment with etanercept may be considered with antituberculous agents only if the potential benefits outweigh the potential risks. In patients with a positive PPD skin test (as evidenced by erythema of at least 20mm in diameter or the presence of induration) or opacities suggesting old pulmonary tuberculosis on chest radiographs, treatment with isoniazid 0.3 g/day should be initiated at least 1 month prior to administration of etanercept and continued for the subsequent 9 months. However, no definite guidelines are available that address how to deal with isoniazid-induced hepatic impairment and isoniazid-resistant Mycobacterium tuberculosis, as well as how long isoniazid treatment should be given. Etanercept is also contraindicated in patients with previous Pneumocystis jiroveci pneumonia, congestive heart failure, malignancies, or demyelinating disease.
To sum up, in this article we focused on the guidelines for the use of etanercept that have been introduced in Japan since spring 2005. In Japan, because only about 100 patients received etanercept in clinical trials, it remains uncertain whether etanercept yields clinical benefit and adverse events with a similar frequency as observed in Europe and the United States. Nonetheless, we will conduct an all-cases postmarketing surveillance using the above-mentioned treatment guidelines, review the results, and revise the guidelines as needed.
References
KW Moreland MH Shiff SW Baumgartner EA Tindall RM Fleischmann KJ Bulpitt et al. (1999) ArticleTitleEtanercept therapy in rheumatoid arthritis. A randomised, controlled trial Ann Intern Med 130 478 Occurrence Handle1:CAS:528:DyaK1MXitFChs7Y%3D Occurrence Handle10075615
ME Weinblatt JM Kremer AD Bankhurst KJ Bulpitt RM Fleischmann RI Fox et al. (1999) ArticleTitleA trial of etanercept, a recombinant human tumor necrosis factor: Fc fusion protein in patients with rheumatoid arthritis receiving methotrexate N Engl J Med 340 253 10.1056/NEJM199901283400401 Occurrence Handle10.1056/NEJM199901283400401 Occurrence Handle1:CAS:528:DyaK1MXht1Wqsbk%3D Occurrence Handle9920948
JM Bathon RW Martin RM Fleishmann JR Tesser MH Schiff EC Keystone et al. (2000) ArticleTitleA comparison of etanercept and methotrexate in patients with early rheumatoid arthritis N Engl J Med 343 1586–93 10.1056/NEJM200011303432201 Occurrence Handle10.1056/NEJM200011303432201 Occurrence Handle1:CAS:528:DC%2BD3cXovVeltLg%3D Occurrence Handle11096165
L Klareskog D van der Heijde JP De Jager A Gough J Kalden M Malaise et al. (2004) ArticleTitleTherapeutic effect of the combination of etanercept and methotrexate compared with each treatment alone in patients with rheumatoid arthritis: double-blind randomized controlled trial Lancet 363 675–81 Occurrence Handle10.1016/S0140-6736(04)15640-7 Occurrence Handle1:CAS:528:DC%2BD2cXhs12jur4%3D Occurrence Handle15001324
J Keane S Gershon RP Wise E Mirabile-Levens J Kasznica WD Schwieterman et al. (2001) ArticleTitleTuberculosis associated with infliximab, a tumor necrosis factor α-neutralizing agents N Engl J Med 345 1098–104 10.1056/NEJMoa011110 Occurrence Handle10.1056/NEJMoa011110 Occurrence Handle1:CAS:528:DC%2BD3MXnsFShsr0%3D Occurrence Handle11596589
MA Gardam EC Keystone R Menzies S Manners E Skamene R Long et al. (2003) ArticleTitleAnti-tumour necrosis factor agents and tuberculosis risk: mechanisms of action and clinical management Lancet Infect Dis 3 148–55 Occurrence Handle10.1016/S1473-3099(03)00545-0 Occurrence Handle1:CAS:528:DC%2BD3sXislKmsLo%3D Occurrence Handle12614731
WHO report Global tuberculosis control-surveillance, planning, financing. http://www.who.int/tb/publications/global_report/en/
Report from the Ministry of Health, Labor and Welfare Japan (in Japanese). http://www.jata.or.jp/rit/rj/data_tp.html
N Miyasaka T Takeuchi K Eguchi (2005) ArticleTitleProposed Japanese guidelines for the use of infliximab for rheumatoid arthritis Mod Rheumatol 15 4–8 Occurrence Handle10.1007/s10165-004-0357-7 Occurrence Handle1:CAS:528:DC%2BD2MXhsV2is7k%3D Occurrence Handle17028815
American College of Rheumatology-Hotline: 1. http://www.rheumatology.org/publications/hotline/0303tnfl.asp
Safety Update TNF-α blocking agents: 1. http://www.fda.gov/ohrms/dockets/ac/03/transcripts/3930T1.htm
BW Van Oosten F Barkhof L Truyen JB Boringa FN Bertelsmann BM von Blomberg et al. (1996) ArticleTitleIncreased MRI activity and immune activation in two multiple sclerosis patients treated with the monoclonal anti-tumor necrosis factor antibody cA2 Neurology 47 1531 Occurrence Handle1:STN:280:DyaK2s7itVSluw%3D%3D Occurrence Handle8960740
MC Genovese JM Bathon RM Fleischmann LW Moreland RW Martin JB Whitmore et al. (2005) ArticleTitleLongterm safety, efficacy, and radiographic outcome with etanercept treatment in patients with early rheumatoid arthritis J Rheumatol 32 1232–42 Occurrence Handle1:CAS:528:DC%2BD2MXnsl2nsrY%3D Occurrence Handle15996057
Miyasaka N. Research report of “Development of Guidelines for the Treatment of Rheumatoid Arthritis with New Biological Products and Research on Their Validation” supported by a Grant-in-Aid for Scientific Research (Prevention and Research of Immunologic and Allergic Diseases) from the Ministry of Health, Labour and Welfare, Japan in 2004; in press
Study Group of the Ministry of Health, Labour and Welfare. Therapeutic manual of rheumatoid arthritis (revised). Diagnostic manual and evidence-based treatment guidelines. Japan Rheumatism Foundation; 2004
F Sakai S Noma Y Kurihara H Yamada A Azuma S Kudoh et al. (2005) ArticleTitleLeflunomide-related lung injury in patients with rheumatoid arthritis: imaging features Mod Rheumatol 15 73–9 Occurrence Handle10.1007/s10165-004-0364-8
J Ogawa M Harigai N Nagasaka T Nakamura N Miyasaka et al. (2005) ArticleTitlePrediction of and prophylaxis against pneumocystic pneumonia in patients with connective tissue diseases undergoing medium- or high-dose corticosteroid therapy Mod Rheumatol 15 91–6 10.1007/s10156-004-0368-5 Occurrence Handle10.1007/s10156-004-0368-5 Occurrence Handle1:CAS:528:DC%2BD2MXjvVCntbw%3D Occurrence Handle17029042
EC Keystone MH Schiff JM Kremer S Kafka M Lovy T De Vries et al. (2004) ArticleTitleOne-weekly administration of 50 mg etanercept in patients with active rheumatoid arthritis. Results of a multicenter, randomized, double-blind, placebo-controlled trial Arthritis Rheum 50 353–63 Occurrence Handle10.1002/art.20019 Occurrence Handle1:CAS:528:DC%2BD2cXhvFeitLc%3D Occurrence Handle14872476
Acknowledgment
This study was supported by a grant from the Ministry of Health, Labor and Welfare, Japan. The authors also express sincere appreciation to the members of the internal medicine rheumatology study group of the Ministry of Health, Labor and Welfare, Japan, i.e., Shigeto Toma, Hisashi Yamanaka, Tetsuji Sawada, Hiroaki Ida, Takao Koike, Hideto Kameda, Yoshiaki Ishigatsubo, Takayuki Sumida, Masayoshi Harigai, Kazunori Tomono, Yoshiya Tanaka, Atsuo Nakajima, Norihiro Nishimoto, Kiichiro Tsutani, Hiroyuki Aburaya, Kazuhiko Yamamoto, Atsuo Taniguchi, Shigeto Kobayashi, Satoshi Itoh, Toshihiro Nanki, Atsushi Kawakami, Tsuneyo Mimori, Takashi Okamoto, Naoyuki Tsuchiya, Shunichi Shiozawa, Masaaki Nakano, Masataka Uetani, and Kiyoshi Migita.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Miyasaka, N., Takeuchi, T. & Eguchi, K. Guidelines for the proper use of etanercept in Japan. Mod Rheumatol 16, 63–67 (2006). https://doi.org/10.1007/s10165-006-0457-7
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s10165-006-0457-7