Abstract
In Zimbabwe, management of medical solid waste is emerging as a visible dilemma. This is attributed to population explosion as well as outbreak of diseases and spread of already existing diseases which accelerate volume of medical solid waste generated by medical facilities. Consequently, the overarching objective of this paper was to review medical solid waste management status in Zimbabwe utilising published documents. The literature demonstrated that medical solid waste generated in Zimbabwe encompasses pathological, pharmaceutical, chemical, infectious, cytotoxic, sharps and general waste. Management approaches used by medical facilities are marred with inappropriateness as shown by storage, collection, conveyance and disposal of non-segregated waste. Verdicts of the study depict that open pit dumping, landfills, incineration, burying, open burning, ottoway pits and open dumpsites are discarding strategies used. However, these strategies pose water, air and soil pollution, therefore, impacting the ecosystem and humanity. Findings indicated that infectious diseases, respiratory diseases, gastro-intestinal problems and injuries emanate due to poor management of medical waste. The roots of unsafe management of medical solid waste include inadequate finance, weak enforcement of legislation, ignorance among health workers and waste workers as well as non-participatory approach in decision making. Zimbabwe is recommended to direct funds to medical solid waste, increase awareness of health workers through trainings and education and reinforcing enforcement of legislation linked to medical solid waste among others.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Medical solid waste is viewed as disposed waste generated from activities such as health protection, diagnosis, treatment, dental and scientific research [1,2,3]. However, this type of waste is also generated at household level during utilisation of dialysis, insulin injections and animal treatment in rural areas [4, 5]. This implies that medical solid waste is confronting both rural and urban areas, hence demand attention. Medical solid waste generated in most continents like Africa consists of 85 percent non-hazardous and 15 percent hazardous waste [6,7,8]. In view of this, a large percentage of medical waste is similar to general municipal solid waste. Nevertheless, owing to insufficient separation medical solid waste turns into entirely hazardous waste [9, 10]. Therefore, medical solid waste requires proper separation from generation to disposal sites to minimise quantity of hazardous waste. A view upheld by Vasistha et al. [4] is that proper management of medical solid waste is essential to protect the environment and uphold human health. Medical solid waste comprises of sharps, pathological, toxic medical chemicals, cytotoxic, medical radioactive, pharmaceutical, infectious and general waste [6, 11, 12]. Considering these various characteristics medical solid waste, its increase has potential to cause injuries, pricks and infectious diseases to people.
Currently, the globe is subjected to growth of medical solid waste quantities due to epidemic diseases like Covid-19 [10, 13]. This was observed in India where medical solid waste volume raised from 0.5 kg to 4 kg per patient per day while in China it explode to 6 kg per bed per day [13]. Henceforth, besides increasing number of patients at medical facilities, diseases accelerate medical solid waste generation. Upsurge of medical solid waste is due to high hospitalisations and use of personal protective equipment such as masks, gloves and gowns [14, 15]. Proliferation of medical solid waste means sustainable management to curb dire environmental impacts is vital. Medical solid waste is regarded as the 2nd perilous waste after radiation waste [2, 3, 16]. This means improper monitoring of the waste have potential to hinder achievement of sustainable development. Medical solid waste can impact water, soil, biodiversity, air and environmental aesthetic value negatively globally if improper management strategies are applied [8, 17] and humanity is also affected [4, 18]. Globally, at least 5.2 million human beings lost their lives annually due to diseases emanating from poorly managed medical solid waste [19]. Medical solid waste mismanagement is linked to nosocomial diseases, gastro-intestinal diseases, skin disorder [8] infectious diseases hepatitis B, C, HIV and AIDS [4, 14, 20]. In order to quell these health risks, health institutions must implement eco-friendly management strategies. However, in Africa apt management of solid waste including medical solid waste is difficult due to social, political, economic challenges and waste increase [21]. Consequently, a myriad of challenges need to be suppressed in order to achieve sustainable medical solid waste management.
Approximately, 67,740 health institutions are in Africa [7] and generate about 282,447 tonnes of medical solid waste yearly [8]. Nevertheless, medical solid waste generation trends may have increased due to Covid-19. These quantities call for vast financial, skilled personnel, effective planning and implementation of rigorous approaches. However, these necessities are inadequate in African countries [22, 23]. Therefore, proper management is rare, presented by indiscriminate disposal of medical solid waste [1, 20]. Bulky volume of medical solid waste is discarded in open pits, poorly constructed landfills, dumpsites as well as low standard incinerators without treatment [23, 24]. This is indicated in Zimbabwe where solid waste including medical waste is monitored by incapacitated municipalities [25, 26]. This revealed that committed government which supports municipalities is necessary to achieve proper medical solid waste management in African countries including Zimbabwe. Zimbabwean government is constructing health facilities to safeguard wellbeing of its citizens who are around 16.53 million as stated by Zimbabwe Statistics and World Bank in 2017. Consequently, the population facilitate high generation of medical solid waste by seeking assistance from health facilities. This concurs with Torkashvard [27] that growth of population upsurge quantity of solid waste, mainly medical solid waste. Zimbabwe is under threat of diseases associated with poor sanitation such as typhoid, cholera, malaria [10, 12, 14]. In addition, United Nations Development Program [28] revealed that over spilling of Covid-19 into Zimbabwe accelerate generation of medical solid waste since it escalates utilisation of personal protective equipment. Therefore, population growth and high disease prevalence are among the drivers of medical solid waste increase in the Zimbabwe.
However, solid waste explosion in Zimbabwe fails to correspond with the prevailing waste management systems [29, 30]. Hence, medical solid waste is affecting the already overburdened solid waste management systems in Zimbabwe. This is because medical facilities in Zimbabwe generate a mixture of both hazardous and non-hazardous solid waste [31, 32]. In the Zimbabwean context, improper management of medical solid waste is ascribed to fragmented weakly enforced solid waste policies and legislations [5, 26, 33]. Nonetheless, regardless of medical solid waste growth and existence of various management challenges in Zimbabwe its literature is limited compared to the quantity generated. This prospect drives the review to focus on medical solid waste management status in Zimbabwe as a general objective, although it will be guided by the following specific objectives: analyse the characteristics of medical solid waste generated, examine medical solid waste management approaches and assess potential environmental risks associated with the management approaches. Attention will also be given to proffering of an integrated sustainable model for medical solid waste management in Zimbabwe.
Study area
Zimbabwe is a landlocked nation occupying about 390,757 square kilometre area in Africa [33] between latitudes 15–230 S and longitudes 25–340 E [34]. Zimbabwe shares frontiers with Zambia, Mozambique, South Africa and Botswana [34]. Koppen–Geiger climate classification denotes that Zimbabwe experiences subtropical climate with hot wet summers and cool dry winters [33, 35]. The country is divided into 5 regions basing on precipitation and temperature experienced in the area [36, 37]. Zimbabwe received an average of about 670 mm of precipitation per annum whilst temperature is around 15 ℃ to 25 ℃ [38]. Zimbabwe Statistics and World Bank (2017) postulated that Zimbabwe’s population is approximately 16.53 million. Like any other country in Africa, people in Zimbabwe are affected by numerous types of diseases such as HIV and AIDS, tuberculosis and poor sanitation diseases such as cholera [39, 40] and Covid-19 [28]. Consequently, they resort to medical facilities for assistance. The entire population is served by 214 medical facilities excluding smaller clinics [41], thus accelerating medical solid waste generation at the facilities. Medical solid waste increase adds burden to a country which is struggling with municipal solid waste [42,43,44]. This initiates the review to merely concentrate on medical solid waste management status in Zimbabwe.
Methodology
The study was grounded on already published literature on medical solid waste management. Similarly, general solid waste literature with aspects of medical solid waste was involved, since medical solid waste literature is limited in Zimbabwe. Articles published in English were reviewed to reach the goal of the review paper. In Zimbabwe, all types of solid waste management is regulated by the Environmental Management Act [Chapter 20:27], effluents and solid waste disposal regulations, 2007. Therefore, the literature published from 2007 to current date was reviewed during the study. However, Taru and Kuvarega [31]’s research was included since the research pave way for other researches linked to medical solid waste in Zimbabwe. The search was carried out utilising a combination of related key terms such as medical solid waste, clinical solid waste, healthcare solid waste and solid waste among others. However, medical solid waste management approaches and environmental health risks associated with the strategies were part of the keywords. Published articles, journals, abstracts, thesis, book chapters and books were retrieved from Google Scholar, Sage Publications, Springer, Science Direct, African Journals Online, Scopus, Web of Science Publications and Pubmed. Development of an integrated sustainable management model for medical solid waste management was based on the literature contextualised in Zimbabwe. Although it was guided by the Deming circle, a systematic review of published literature offers an understanding of medical solid waste management status and opportunity to proffer recommendations.
Types and characteristics of medical solid waste
In Zimbabwe, medical solid waste is produced by households, hospitals, clinics during patient treatment, diagnosis, caring and immunisation [31], in form of pathological, pharmaceuticals, sharps, radioactive, toxic chemical waste, infectious waste, cytotoxic waste and general waste [20, 46]. Hence, medical solid waste generated by health institutions, households and elderly care facilities in Zimbabwe consists of hazardous and non-hazardous solid waste. This coincide with Ali et al. [9], Rahman et al. [45], and WHO [54] that medical solid waste consist of 85 percent non-hazardous and 15 percent hazardous waste. This means Zimbabwe produces medical solid waste similar to other countries as demonstrated in Table 1, hence need enhanced management approach.
Pathological waste produced consists of body parts, human tissues detached during surgery, operations and autopsy, placentas, and foetuses from stillbirths [46, 54]. World Health Organisation [15] opines that pathological waste is infectious due to existence of virus and bacteria in human tissue samples. Therefore, proper handling of pathological waste should be mandatory among health workers in Zimbabwe to curb spread of infectious diseases. In Zimbabwe, expired drugs, contaminated drugs and their containers disposed in Zimbabwe are considered as pharmaceutical waste [47, 48]. Nevertheless, pharmaceutical waste quantity is always low in Zimbabwe due to financial crisis which facilitates proper planning when purchasing and utilising drugs. Sharp waste includes needles, syringes, blades, broken glasses, knives, scalpels, infusion sets and pipettes [20, 31]. Considering these categories of medical waste in Zimbabwe proper management is the only way forward to minimise health risks such as sharp injuries, cuts and pricks. Sharp waste may cause injuries, thus facilitating spread of diseases such as HIV and AIDS, and hepatitis B and C; hence, special care is recommended when dealing with medical sharp waste [49, 50].
In the Zimbabwean context, infectious waste comprise of soiled dressings, surgical gloves, bandages, sponges as well as swabs contaminated by excreta, blood and fluids from patients with communicable and contagious diseases in isolation, surgical wards and theatre [20, 31]. Currently, infectious waste explodes due to high use of personal protective equipment (gloves, gowns, masks, goggles, and boots) in Zimbabwean hospitals owing to Covid-19 outbreak [28]. As a result, stakeholders like Environmentalist and Health and Safety officers should co-ordinate to craft measures to protect both the environment and health workers from infectious waste. Utilisation of nuclear medicines, unsealed radionuclides and therapeutic procedures in Zimbabwe facilitate generation of radioactive waste [20]. Yves-Chartier [12] indicated that equipment (glassware, packages, absorbent paper) contaminated by radioactive substances during the diagnosis process are included as medical radioactive waste. This type has potential to cause genetic mutation and cancer to health workers in Zimbabwe, therefore, require close attention. Pressurised containers which include oxygen cylinders, aerosol and air fresheners containers are among medical solid waste. This simply means different methods are required to manage various types of solid waste from medical sector in Zimbabwe.
Jerie [51] revealed that medical toxic chemical waste consists of containers with remains of clinical chemicals, sterilant, disinfectants, reagents, solvents as well as heavy metals like mercury from batteries. Hence, medical facilities in Zimbabwe produce medical toxic chemical waste since chemical containers, broken clinical thermometers and blood pressure gauges with mercury are part of the waste. General medical solid waste is generated from administration offices such as papers, plastic containers, as well as food waste from the kitchen and visitors who brought food, flowers to their admitted relatives [20, 31]. This suggests that medical facilities in Zimbabwe produce certain quantity of solid waste with similar characteristics to household waste, therefore, can be reused or recycled. Solid waste is considered non-hazardous if it is not mixed or get in contact with hazardous waste [49, 50]. Therefore, improper segregation of medical waste in Zimbabwe hinders application of reuse and recycle strategies, since the waste became wholly hazardous. Zimbabwean hospitals generate cytotoxic drugs and their metabolites as part of cytotoxic waste. This clearly denotes that medical solid waste requires attention owing to existence of various categories of waste.
Medical solid waste management in Zimbabwe
Storage and segregation of medical solid waste
Studies by Tsiko and Togarepi [46] indicated that solid waste generated in hospital wards is put in small containers or boxes and they are emptied in large containers placed in the corridors. When the containers in the corridors are full with mixed medical solid waste, they are conveyed for storage site [31]. This suggests that medical solid waste storage in Zimbabwe is marred with confusion, since the storage process may expose humanity to health risks. As a result of continuous emptying of medical solid waste into containers placed in the corridors, their capacity will be exceeded resulting in spilling of waste to the floor [20]. Thus, exposing various groups of people to pricks, injuries, piercing and infections from poorly stored waste. Hence, there is need for medical facilities in Zimbabwe to have separate areas (rooms) for solid waste storage before conveyed from onsite to waste site.
Taru and Kuvarega [31] opined that in the Zimbabwean context, medical solid waste is stored indiscriminately since infectious waste and sharps are mixed with pathological waste. However, medical solid waste should be segregated in different colour-coded stiff containers with bin liners and lids during storage in a secured place [7, 15]. Sharps are always stored in any container which is available and mixed up with other types of waste for instance pharmaceutical and infectious waste [20]. This goes against the view of World Health Organisation [54] and Zimbabwe Ministry of Health [55] that sharp waste should be stored in puncture proof containers which can be sealed when it is full. Taking into account the above, medical solid waste segregation is full of chaos since despite that medical solid waste is different it is indiscriminately stored and disposed. This coincide with Mangizvo and Chinamasa [20] that in Zimbabwe general solid waste generated is collected and disposed together with medical hazardous waste haphazardly. This suggests that segregation of medical solid waste should be done at initial stages of waste management chain like storage, to enable collection and disposal of segregated waste.
Collection and conveyance of medical solid waste
Tsiko and Togarepi [46] observed that collection and transportation is done utilising wheeled trolleys from points of generation (hospital departments and wards) to onsite areas of temporary storage. Medical solid waste is conveyed from areas of generation to final discarding areas, namely landfills, dumpsites and point of incineration by municipalities waste trucks [20, 46]. Consequently, participation of medical solid waste generators in management of medical solid waste from cradle to grave is lagging behind in urban hospitals, since the burden shifted from medical sector to incapacitated municipalities. Municipalities collect medical solid waste to ensure that areas under their jurisdiction are not contaminated by solid waste as stipulated by the Urban Council Act (Chapter 15:09) [56, 57]. However, the situation begs to differ in rural areas since medical waste generators manage medical solid waste from collection to disposal because they are not beneficiaries of the Act. This implies that legislations and Acts that cater for medical solid waste management in rural areas are prerequisite in the Zimbabwe.
In the Zimbabwean context, medical solid waste collection is inefficient owing to delays, due to shortage of capacity as a result of lack of dump trucks, finance and fuel. Collection rate of solid waste encompassing medical waste in Zimbabwe is approximately 60 percent [53, 58]. This coincide with Haregu et al. [59] who revealed that collection of solid waste by municipalities in less industrialised countries is always less than 70 percent. Efficient collection of municipal solid waste in including medical solid waste in Zimbabwe is hindered by fuel, financial and transport deficit [53, 60]. This shows that economic challenges in Zimbabwe crippled efficient collection and conveyance of medical solid waste, therefore, averting the ability to reach sustainable development goals. Solid waste in Zimbabwe should be collected at least twice per week due to climatic conditions in the country [26, 61]. This means frequent collection of medical solid should be carried out in Zimbabwe, to avert odours from decomposing waste. However, in Zimbabwe, solid waste including medical solid waste is collected to areas of final disposal once a week or once a month due to fuels’ shortages [29, 31, 42]. This means collection of medical solid waste in Zimbabwe fail to conform to World Health Organisation guidelines. Postponement of medical solid waste collection gives pathological waste opportunity to decompose, hence exposing the environment and human health at risk. Heaping of uncollected waste is witnessed at medical facilities and households in Zimbabwe. As a result, scavenging domestic, wild and stray animals tear and open waste containers, hence exposing themselves to health problems. During deployment of waste trucks, no specific routes are followed; therefore, collection is done haphazardly [26, 62]. Consequently, sometimes other suburbs and institutions are skipped; therefore, medical solid generated in those areas’ facilities will suffer since waste is not collected. Continuous accumulation of uncollected solid waste at onsite area creates conducive environment for breeding of cockroaches, rats and flies which speeds the spread of waste-related diseases [25, 51]. This depicts that uncollected medical solid waste facilitates the occurrence of waste-related diseases; therefore, efficient collection rate is a mandatory. Nevertheless, municipalities argued that inadequate collection of solid waste including medical solid waste in Zimbabwe is ascribed to underfunding and limited co-operation of rate payers [26], although Zimbabwean residents conclude that funds misuse and misallocation by municipalities that exacerbate inefficiency collection of waste [53] and medical solid waste is not spared. This suggest that inappropriate collection of medical solid is a result of blame game between the city fathers and residents, hence they must work together to achieve efficient waste collection.
Disposal of medical solid waste
In Zimbabwe, about 90 percent of solid waste, including medical waste is disposed in indiscriminate state [26, 58]. This revealed that sustainable alternatives such as recycle, reuse and prevention need to be applied in medical waste management in Zimbabwe, to minimise quantity of waste disposed. Approximately, 40 percent of solid waste encompassing medical solid waste is disposed in an illegally manner along road edges, in drains and open spaces [53, 58]. This implies that a certain proportion of medical solid waste is also destined in undesignated disposal sites, thus exacerbating occurrence of environmental health problems. Taru and Kuvarega [31] revealed that medical solid waste disposal approaches utilised in Zimbabwe include open dumping, burying, open pits, and burning. This is pathetic since most the approaches used to dispose medical solid waste forms the base of solid waste management hierarchy. Makarichi et al. [57] pointed out that 37.6 percent of solid waste from different sources is burned through uncontrolled open burning at generation point in Zimbabwe. This point out that medical solid waste is also disposed through open burning which can be controlled or uncontrolled burning since it is capable to reduce quantity of waste as well as destroying pathogens, virus and bacteria.
In addition, Jerie and Musasa [46] asserted that incineration is highly utilised to dispose medical solid waste. Considering the mentioned approaches, it is clear that Zimbabwe is still utilising the least desired strategies to dispose medical solid waste; therefore, a road map to reach upper part of the waste management hierarchy is required. Strategies namely plasma, gasification as well as electro-thermal deactivation of medical waste can be used to treat and dispose medical solid waste in Zimbabwe, than solely relying on incineration. Ferreira and Veiga [63]; Rana and Ganguly [64] and Vasistha et al. [4] concur that medical facilities resort to incineration because it is capable to reduce the quantity of medical solid waste by about 80 percent, detoxification and destroy pathogens. In less developed nations, incineration is viewed as a golden approach, although utilisation of low standard incinerators result in spike of emissions in the atmosphere [9, 17]. This is exemplified by Mangizvo and Chinamasa [20]’s studies in Kwekwe which demonstrate that the incinerator used for medical solid waste disposal was operating inadequately owing to collapse of furnace lining. In addition, overloaded non-segregated solid waste limits the efficiency of incinerators since non-combustible and wet waste is resistant to incineration [20, 31, 52]. Therefore, none ash residues of medical solid waste such as glasses, sharp waste and containers finds their way to disposal sites, exposing informal waste collectors to injuries.
Nyakatswau et al. [48] argued that solid waste in Zimbabwe is collected by municipality dump trucks to be discarded in official dumpsites despite difference of their origin, type or potential environmental effects. Hence, medical solid waste with its hazardous characteristics is also transported to dumpsites together with other general solid waste. This generally means policies and legislations which support segregation of medical solid waste at initial stages is required to achieve proper disposal. Approximately, 90 percent of solid waste generated in cities is conveyed to dumpsites for instance Pomona in Harare [52, 58], this means medical solid waste is not spared. As evidenced by this a large volume of medical solid waste is disposed, therefore, recycling and reuse is rarely practised in Zimbabwe. This goes with Taru and Kuvarega [31] who postulated that medical solid waste generated by Parerenyatwa medical facilities is transported and discarded on dumpsites. Nevertheless, besides increasing environmental health risks, medical solid waste is partly speeding exhaustion of dumpsites which are already dying a slow death. This is demonstrated by the Pomona dumpsite which was projected to be closed in 2020, since solid waste was exceeding its capacity [52]. Consequently, Zimbabwe must not focus on collect and dispose approach when dealing with medical solid waste.
Moreover, medical solid waste generated by rural areas is discarded in open pits in Zimbabwe owing to its low costs. However, this approach can be a potential source of infection to public health and exacerbate cropping of different environmental problems if poorly managed [51, 65]. In addition, openly discarded medical solid waste is exposed to blowing wind, thus accelerating rate of cross infection to the nearest residential areas. A view upheld by Jerie and Zulu [66] is that residential areas located less than 500 m from the dumpsites are vulnerable to problems associated with solid waste. Infectious medical solid waste is supposed to be treated utilising autoclaving system and chlorine to disinfect it before being disposal in Zimbabwe [20]. Nevertheless, these strategies cannot be applied frequently due to financial constraints; therefore, despite being a major emission generator, incineration remains the only option. This congruent with Tanyanyiwa [60] and Chapungu et al. [67] failure to adopt or utilise sustainable waste treatment or disposal in Zimbabwe that is attributed to limited finance.
Zimbabwe like other least industrialised nations, utilises landfilling as an alternative to dispose medical solid waste; however, the dilemma is they are operated like open dumpsites. In developing nations, approximately 50 percent of collected solid waste is discarded through poorly controlled landfills [59, 68]. Landfills in Zimbabwe are like dumpsites since solid waste is non-compacted, not covered by soil and landfills lack leachate and gas control systems owing to limited funds and lack of experts [56, 57]. This implies that pollutants from decomposed medical solid waste can potentially cause deleterious impacts to the environment. Municipality solid waste on dumpsites is always exposed to open burning [42, 62]; therefore, medical solid waste is also burned at rural and urban health facilities. Therefore, medical solid waste is also destroyed through open combustion in Zimbabwe [20, 31].
In rural hospitals, ottoway pits are also utilised to dispose pathological waste, but the problem is sharps and infectious waste mixed with pathological waste [20], hence finds their way into ottoway pits. This minimise effectiveness of ottoway pits as an alternative to dispose pathological waste. In addition, most of the times the ottoway pits are not lined, this gives the leachates from ottoway pits opportunity to pollute groundwater as well as soil. Unlined solid waste disposal sites produce leachates, acids and ions which contaminate soil and ground water [50, 56]. In Zimbabwe rural medical facilities, burying of waste is usually practised [65]. From the above, it is not an exaggeration if one argues that most of the approaches utilised to dispose medical solid waste in Zimbabwe are far from the recommended standards to reach sustainability. Currently, disposal of solid waste including medical waste is problematic in Zimbabwe due to waste increase, sub-optimal infrastructure and absence adequate waste data [57, 58]. However, Tanyanyiwa [60] and Nhubu and Muzenda [52] noted that disposal solid waste including medical waste is emerging as a problem due to Not In My Backyard syndrome. This principle increase difficulties to locate medical solid waste dumpsites since people are aware of environmental health risks associated with improperly monitored dumpsites.
Environmental health risks associated with medical solid waste management
Medical solid waste generated by health institutions may pose dire impacts to the environment, especially if the least desired discarding approaches are used [6, 9, 46]. This means flora and fauna as well as water sources, soil and air in Zimbabwe are at risk owing to improper medical solid waste management. According to Ali et al. [9], Askarian et al. [6] and Ansari et al. [49], non-treated medical solid waste release toxic pollutants and pathogens such as bacteria and viruses in the natural environment. Thus, exposing different fauna species with access to the dumpsites to viral and bacterial diseases. This is inevitable in Zimbabwe where most of the dumpsites are unsecured [46]. Inadequate incineration of medical solid waste with polyvinyl chloride results in air contamination by dispersing carbon monoxide, dioxide, nitrous oxide, furans and dioxins in the atmosphere [31, 41, 50]. This illustrates that improper management of medical solid waste is increasing human carbon footprint in Zimbabwe. This is the reason why medical facilities are regarded as the 5th emitter of greenhouses gases at global level, generating approximately 4.4 percent [7, 9, 49]. As a result, improper solid waste management including medical waste management in Zimbabwe accelerates climate change [52, 58]; therefore, medical solid waste management cannot be neglected in Zimbabwe. Moreover, humans who inhale toxic gases from medical solid waste may suffer from chronic and acute respiratory diseases such as tuberculosis, coughing alongside cancer [6, 49, 51]. In Zimbabwe, less effective incinerators are utilised to dispose medical solid waste [20, 31]. This implies that partially burnt solid waste such as sharps and bottles always finds their way to the dumpsites and speedy exhaustion of dumpsites. Therefore, in the Zimbabwean context methods such as granulation, shredding, crushing, pulverisation, grinding and crushing with potential to reduce volume of waste which is not suitable for incineration.
Medical facilities incinerate clinical thermometers, fluorescent tubes, blood pressure gauges and electrical gadgets which contain carcinogenic heavy metals such as mercury, cadmium, lead, copper and zinc [2, 9, 49]. Hence, human beings are vulnerable to neurological disorders, genetic mutation and blood pressure due to exposure to heavy metals. Disposed medical solid waste was found to generate copper, zinc, mercury, lead, cadmium and chromium [1, 9, 23]. However, the non-biodegradable characteristics of heavy metal increase its accumulation in the environment causing health problems to human beings [51]. This suggest that people who reside in proximity to medical solid waste incineration sites can be affected by various types of cancer such as colon cancer, since medical waste is a source of heavy metals. In addition, leachates containing heavy metals and pollutants from decomposed result in water pollution which later cause ulcers to people [27, 51]. This implies that cost-effective as well as environmentally friendly strategies must be used to dispose medical waste to reduce quantity of heavy metals in the environment. Pollutants from medical waste and excessive radiation from incineration affect birth weight of unborn babies (foetuses) and catalyse occurrence of down syndromes [11, 31, 51]. This means medical solid waste incineration affects pregnant mothers, yet in rural areas of Zimbabwe, incineration is done at hospitals. Inefficiency solid waste collection in Zimbabwe is increasing ability of medical solid waste to cause dire impacts. This is because inadequate collection forces residents to turn to open burning [26, 56] and this also infiltrate to medical facilities since they will be trying to reduce volume of uncollected waste. However, uncontrolled burning of medical solid waste produce smoke which act as nuisance to people and contaminates the air. Contaminated air causes eye irritation, bronchitis, dry cough, tuberculosis and asthma [51, 68]. Hence, burning of medical solid waste has potential to diminish humanity’s wellbeing.
In Zimbabwe, medical solid waste is dumped in open pits which are improperly managed, thus increasing breading of diseases vectors and environmental pollution. Open pits and open dumping creates favourable breeding sites for mosquitoes, rats which cause malaria and rat-bite fever, respectively, alongside flies which transmit dysentery, typhoid and cholera [51, 67]. Therefore, medical facilities, which are considered safe places, are now fuelling outbreak of diseases relating to poor solid waste management in Zimbabwe. Improper management of solid waste including medical solid waste also contributed to 2008–2009 outbreak which lead to death of approximately 3.500 people [39, 69]. Furthermore, medical solid waste disposed in open pits are easily accessible by domestic dogs, goats, birds and cats, and this exacerbate cross infection to residential areas. Domestic animals like dogs always collect anything they pick to residential areas [20], thus increasing vulnerability of people to risks associated with medical solid waste namely infectious diseases. Decomposition of solid waste including medical waste on landfills and dumpsites generates leachates, acids and heavy metals which contaminate water and soil [52, 57]. This advocates that decay of medical solid waste on landfills that pose dire impacts to water and soil quality; therefore, flora is not spared. Dissolved minerals from landfills and dumpsites cause water-borne diseases such as typhoid, cholera, and dysentery [70], as well as propelling growth of water hyacinth in water sources [26, 58]. As a result of disposal of medical solid waste on poorly engineered landfills and dumpsites, water contamination is inevitable in Zimbabwe. Pomona, Chitungwiza and Golden Quarry dumpsites in Zimbabwe lack mechanisms that reduce infiltration of leachates to groundwater [57]; hence, ground water pollution is inevitable. Therefore, Zimbabwe as a country should put emphasis on constructing waste sites which impede free leachate movement.
Incineration of solid waste specifically medical solid waste produce ashes with high toxic heavy metals and organic contaminants with potential to pollute ground and surface water [53, 71, 72]. This revealed that it is vital for Zimbabwe medical sector to eliminate or reduce toxicity of incineration residues and ashes before disposing into landfills. Pollutants and heavy metals are absorbed by plant roots and trans-located to edible fruits and roots [73]. Given this, pollutants from medical solid waste find their way into the food chain since browsers and humans always survive from green plants and fruits. However, ingestion of fruits or roots containing pollutants increase occurrence of ulcers, cancer and diarrhoeal diseases [73]. A view upheld by Ansari et al. [49] is that impurities of medical solid waste in soil can pose various abdominal pains. Therefore, soil contaminated by medical solid waste pollutants can accelerate abdominal pains in Zimbabwe since geophagy is rampant. Landfills are known generators of irritating odours and methane gas, a greenhouse gas which accelerate global warming [70]. Henceforth, besides causing health problems, decomposed medical solid waste speeds up global warming, thus facilitating climate change. Mobile refuse trucks pollute the air since they utilise petrol or diesel which produce greenhouse gases [53], similarly medical solid waste refuse trucks produce toxic gases such as nitrous oxide, sulphur dioxide and hydrocarbon particles. Thus, increasing global warming and respiratory problems to people in the vicinity. Studies in Kwekwe show that open trucks which enable medical solid waste to fall were used to convey waste to incineration site [20]. Falling solid waste including medical solid waste result in land pollution [26, 74], if it remain unpicked, visual pollution increases. Therefore, strict handling of medical solid waste and monitoring of dumpsites is required in Zimbabwe to avert appearance of medical waste as nuisance. Visual pollution diminishes aesthetic value of the environment [26], thus impacting tourism which a source of income in Zimbabwe. Therefore, apart from being an eyesore, medical solid waste hinders economic growth in Zimbabwe since it minimises inflow of tourist since they shun waste. This means utilisation of proper well-serviced vehicles is required when ferrying medical solid waste to minimise air pollution and land pollution.
Cuts, puncture, and injuries caused by disposed sharps such as needles and broken glasses cause easy penetration of fungi, virus and bacteria into human system [20, 51]. Therefore, medical sharp waste has potential to increase spread of Hepatitis B, C, HIV and AIDS, Ebola and Covid-19 since they contain viruses from infected people. A view upheld by Ramteke and Sahu [13] and World Health Organisation [15] is that medical sharp results in injuries and cuts which increase transmission of Hepatitis B and C, HIV/AIDS and Covid-19. In 2018, HIV, hepatitis B and hepatitis C new infections caused by infected sharp waste like syringes was approximately 260,000, 21 million and 2 million, respectively [75]. In addition, medical solid waste contaminated by infectious saliva, blood and body fluids increase spread of infectious diseases [2, 10]. This means in Zimbabwe, health workers, waste collectors, patients and public are under threat since they are always in contact with medical solid waste with various types of infectious waste such as sharp waste. In Zimbabwe, people are exposed to anthrax due to contact with medical waste generated during treatment of domestic animals. Children and scavengers who access dumpsites with medical waste without safety gear are also vulnerable to infectious diseases. Health workers and waste collectors in Zimbabwe took safety gear for granted and became more vulnerable to injuries and infections caused by medical sharp waste. This is supported by [76, 77] that solid waste workers specifically informal workers (scavengers) are exposed to various waste-related injuries or diseases since they work without required personal protective equipment. In addition, sharp waste also contain biological pathogens which cause diseases like tetanus [50, 51]. This means scavengers who look for valuable materials from dumpsites and children who use medical solid waste dumpsites as playgrounds are at risk of being infected by infectious diseases since they are always not vaccinated.
Competition of informal waste collectors and dogs to reach consumable, reusable and recyclable medical solid waste at the dumpsites expose human beings to injuries and being bitten. Jerie [51] postulated that human beings may be bitten by stray dogs during scavenging activities, hence became infected by rabies. Occupational risks like musculoskeletal disorders affect people who deal with lifting of objects such as loading and offloading of materials [43, 51]. This implies that medical solid waste workers in Zimbabwe are affected by hands, wrist and shoulder injuries as well as upper, lower back pain alongside chest pain due to loading and offloading. Therefore, dealing with medical solid waste speeds lives of the waste workers to the grave unknowingly, hence strict legislation should be implemented to protect waste workers. In Kwekwe, Zimbabwe, medical solid waste collectors are always transported in the same truck with solid waste [20]. Consequently, the workers are exposed to infectious diseases which they also ferry to their families since they went home with their infected clothes. Open dumpsites are known as sources of spiders, scorpions, odours, houseflies, rats and cockroaches which can affect nearest residential areas [67, 70]. Henceforth, attention in form of proper Environmental Impact Assessment is required when siting medical waste dumpsite. This is because households located less than 500 m from waste sites are under threat of problems that emanate from the sites [66]. This denotes that medical solid waste sites in rural areas pose numerous problems to people since they are located within the health premises. Njaya [78] observed that solid waste which rots quickly attract disease-transmitting organisms and vectors, thus impacting human health. Therefore, medical solid which consist of wet cotton wools, swabs, soiled bandages, pathological waste quickly decompose especially under high temperatures, hence generating odours, disease vectors.
Informal waste collectors inhale, ingest and absorb residues of chemicals such as fluorine, chlorine, deinking and cleaning detergents into their systems resulting in liver and kidney damage [51, 79]. As a result, medical solid waste collectors’ health is affected since medical facilities are major homes of chemicals in Zimbabwe. Solid waste workers are exposed to health problems since they always contact medical toxic chemical and medical radioactive waste [19, 43, 46]. Therefore, activities involved in medical solid waste management in Zimbabwe from cradle to grave expose humanity to numerous health risks; however, the likelihood and severity differ. A view which correspond with Ghafuri [80] results obtained through Preliminary Hazard and Risk Analysis and Risk Assessment Matrix is that segregation of medical waste is a high risk activity, while collection, treatment alongside discarding are medium risk events. This is presented in Table 2. Analysis goes on to demonstrate that pathological, infectious and sharp medical solid waste are considered as source of high risk [80] as shown in Table 2. Considering findings in Table 2, Zimbabwe’s health workers, waste collectors, community as well as the environment cannot escape risks associated with medical solid waste easily. Therefore, crafting of an integrated medical solid waste management model which capacitate co-ordination among different stakeholders pave way for Zimbabwe to reach sustainability.
Medical solid waste legislation and policies in Zimbabwe
Management of solid waste is a burning issue which was discussed at the Agenda 21 and the current Sustainable Development Goals. Consequently, Zimbabwe is giving attention to medical solid waste to achieve sustainability by 2030 [81]. In year 2012, Zimbabwe Ministry of Health and Child Care guided by the World Health Organisation protocols implemented guidelines for discarding pharmaceutical waste. However, the guidelines’ loophole is lack of waste reduction approaches and penalties imposed to those who fail to conform to the guidelines. Hence, medical waste in form of pharmaceutical waste remains a challenge in Zimbabwe. Zimbabwe’s Ministry of Health and Child Care informed medical facilities that they must acquire consent from the appropriate authority or manufacturer before discarding expired drugs [47, 55]. The Ministry of Health and Child Care indicate the roadmap of monitoring medical solid waste generation to disposal, in the handbook entitled “Infection Prevention and Control Handbook, Written by Doctor Gwinji in 2013. In view of this, Ministry of Health and Child Care is eager to contain risks associated with medical solid waste, but due various challenges, their efforts remain in vain. In addition, Ministry of Health and Child Care handbook does not show how waste minimisation strategies can be applied.
Reviewing of worldwide conventions directed to medical solid waste management denote that Zimbabwe signed the Basel Convention, Stockholm Convention and Rotterdam Convention [28]. The country is a signatory of Bamako Convention as well as Minamata Convention. In addition, Basel convention which focus on trans-boundary movement and management of hazardous waste was ratified in 2012 by Zimbabwe. The Basel convention is centred on minimising dire impacts associated with hazardous waste including medical solid waste. Therefore, by being a signatory of this convention, Zimbabwe is willing to conform to sustainable management of medical solid waste. Moreover, in trying to deal with hazardous radioactive and chemical waste, Zimbabwe is part of countries who signed Bamako convention. Considering characteristics of medical solid waste, it is not excluded in the convention; therefore, Zimbabwe is following goals of Bamako convention to monitor the waste properly. However, despite being member of the conventions, failure of Zimbabwe to conform is ascribed to inadequate finance. There are also no clear objectives on how hazardous waste such as medical waste can be recycled or how resource recovery can be applied.
Zimbabwe signed and ratified the 2012 Stockholm convention. The convention encourages eradication or reduction of persistent organic pollutants through apt management of waste piles. Hence, medical solid waste is not spared since incineration and open burning is used to dispose waste in Zimbabwe. Under Article 5 and Annex C, members of the convention are required to avoid disposal methods that produce persistent organic pollutants mostly dibenzofurans and polychlorinated dibenzo-p-dioxins. Hence, Zimbabwe must fit in medical solid waste disposal strategies and structures that meet the demands of Stockholm convention. Moreover, Zimbabwe is guided by Minamata convention when dealing with materials that contain mercury. This implies that medical solid waste such as batteries, fluorescent lamps, dental amalgams and clinical thermometers are managed through requirements of the convention. This will enable the country to move towards sustainable development goals. Medical facilities produce containers with residues of chemicals such as detergents, reagents and other materials contaminated by chemicals [20, 51]. Therefore, by being a member of Rotterdam convention, Zimbabwe is expected to deal with medical solid waste in a way that reduce detrimental impacts of chemical waste.
In the Zimbabwean context, specific Acts and Statutory Instruments related to medical solid waste does not exist. However, the legal framework for medical solid waste monitoring is grounded on the Environmental Management Act Chapter 20:27. The Act urges and encourages proper management of solid waste in Zimbabwe, and medical solid waste is not spared. However, the Act neglect aspects such as solid waste reduction, segregation as well as recovery approaches. Statutory Instrument 6 of 2007 on waste and solid waste and Statutory Instrument 268 of 2018 on hazardous waste offer regulations which encourage proper management of solid waste, including medical solid waste [82]. Although, statutory instrument fail to indicate clearly how various solid waste generators will be enforced to practise proper management of waste. The acts offers room for formulation of environmental quality standards and issues linked to environmental sustainability notably management of all types of solid waste. Nevertheless, it fails to consider vital issues like how integrated solid waste management can be achieved.
Environmental Management Act 20:27 criminalise pollution of the environment by individuals, formal and informal industries and medical facilities are not spared. Therefore, for medical facilities in Zimbabwe to be free from polluter paying principle, they must act according to requirements of Environmental Management Agency. Nevertheless, the fines imposed on medical facilities are very low; therefore, improper management of medical waste perpetuate. Zimbabwean Government [83] and De Gobbi [84] Environmental Management Agency Act 20:27 and 2013 Constitution of Zimbabwe Section 73 stipulates that every person has the right to a non-hazardous environment. Hence, if medical facilities fail to discard solid waste in an appropriate manner, they will contravene to the law. However, the problem is that environmental rights are centred on human beings while ignoring other environmental attributes affected by poorly disposed waste. Under Sections 55–56 of the Act institutions who produce polluting materials must conform to environmental quality standards. This suggests that health institutions are not spared since they generate solid waste which deform quality of the environment.
Zimbabwe also utilises Hazardous Substances Act Chapter 15:05, Statutory Instrument 10, of 2007 to monitor hospital solid waste [32]. The Act indicates that generators of hazardous waste are responsible for sustainable management of the waste. With this in mind, medical facilities in Zimbabwe are accountable for proper management of medical solid waste. Transportation of medical solid waste in Zimbabwe is guided by Hazardous Substances Act which stipulate that hazardous waste should be conveyed in specific vehicles. However, in Zimbabwe, multipurpose vehicles are used [20]. This is attributed to inadequate waste trucks as well as fuel. The major loophole of Hazardous Substances Act is that it is silent about the three Rs of solid waste management which are recycle, reuse and reduce. Hence, medical solid waste is mostly destined in disposal facilities. Urban Councils Act, Chapter 29:15 Statutory Instrument 68 of 2021 subsection 1 of section 4 shows that municipalities are responsible for offering waste collection services in urban areas [52, 85]. This means medical facilities in urban areas benefit while rural health institutions deal with their own solid waste, although rural medical facilities produce medical solid waste with characteristics to waste from urban hospitals. In this view of this, an act directed to marginal areas must be crafted. In addition, Urban Council’s Act provides generators of medical waste in urban areas opportunity to be mere participants in management of their waste. Therefore, adding burden to already ill equipped municipalities, thus exacerbating mismanagement of medical waste. Nevertheless, the major weakness of the Act is failure to highlight the consequences a council will face if it failed provide waste services to areas in its jurisdiction. Moreover, it does not include solid waste management approaches a council should apply after collection; therefore, councils mostly relied on collection and disposal approach.
Zimbabwe also applies the Public Health Act Chapter 15:09, this act deals with the control of emission and disposal of waste to reduce outbreak of diseases. The Public Health Act Chapter 15:09 forms the basis for healthcare and environmental health service. The Act shows that individuals and organisations must utilise waste management approaches that reduce negative health impacts to the public for instance infectious diseases. This suggests that medical facilities have to conform to the requirements of Public Health Act, when disposing medical solid waste. Ineffectiveness of Public Health Act is ascribed to its failure to indicate clear standards and procedures in solid waste management. Consequently, adoption of proper management of medical solid waste remains at miniature stage. Environmental Management Act Chapter 20:27, Statutory Instrument 72 of 2009 is also vital for air pollution control. According to subsection 4, Section 63 of the Act, individuals, industries and institutions involved in activities which emit pollutants into the atmosphere are included. Hence, medical facilities who incinerate or burnt medical solid waste is not spared.
According to Statutory instrument 72, height of emitting chimney should be 50 m or taller than all the buildings at any institution. This guides health institutions when constructing chimneys of their incinerators. However, in Zimbabwe, hospitals always fail to conform the standard; hence, they are liable to heavy fines. The atmospheric pollution act gives Environmental Management Agency authority to inspect emission structures, this means hospital incinerators are also inspected. Emission samples are also tested using blue, green, yellow and red bands. If incinerator emissions are above the required colour bands, medical facilities will be susceptible to polluter pays principle. Although, the penalties and cost of remediation are unexceptionally very low. In addition, occupational health and safety legislation such as Statutory Instrument 68 of 1990 supported by the 1996 Factories and Works Act Chapter 14:08 protect employees including health workers against workplace injuries by promoting safe work environments [48, 86]. This implies that medical solid waste generators, handlers and collectors are also protected since medical waste is hazardous. Factories and Works’ Act fail to address its objectives fully since it does not provide waste handling procedures and standards. In order to protect the general public, all organisations and individuals urged to discard or destroy pharmaceutical waste using strategies which are harmless to humans and their surroundings [48, 55]. This advocates that in the Zimbabwe, medical facilities are supposed to monitor management of medical solid waste from cradle to grave. However, the situation begs to differ since municipalities are responsible for management of medical waste from collection to disposal.
Proposed integrated sustainable model for medical solid waste management
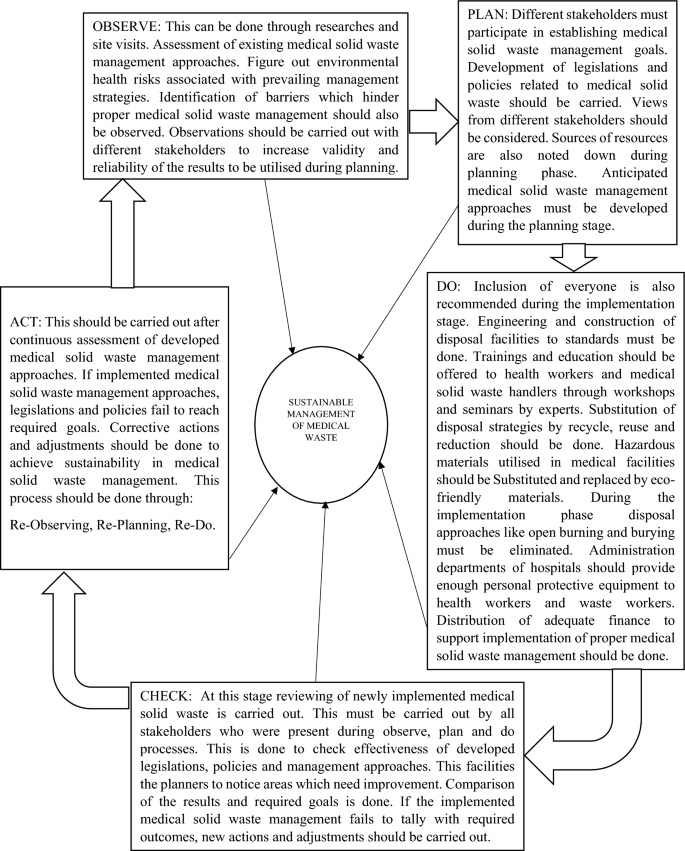
In the Zimbabwean context, medical solid waste mismanagement is omnipresent. This means there is need for a sustainable model to act as a pathway to achieve apt management of medical solid waste. As a result, an integrated sustainable model was crafted basing on the Deming OPDCA Circle of improvement. In the OPDCA abbreviation, O is for Observation, whereas P is planning, while D stands for Do, C represents Check and A is Act. OPDCA circle is considered as an effective strategy for improvement by [87, 88]. This implies that to improve medical solid waste management, the OPDCA system must be adopted for proper decision making and enhancement of existing strategies. The proffered model in Fig. 1 demonstrates that different stakeholders for instance Ministry of Health Care, Environmental Management Agency, Hospital Environmental Health Departments as well as Local Authorities must observe the status of medical solid waste management through researches and site visits. This assist in figuring out the strength and loopholes of existing medical solid waste management approaches. Observations enable medical solid waste experts to know who is slacking and what is lacking in medical solid waste management. Unearthing of environmental health risks associated with the management approaches provide enough information to utilise during planning.
Effective planning on medical solid waste management in Zimbabwe requires inclusion of different stakeholders. In order to establish real achievable goals towards medical solid waste management, various people from community to national level must be encompassed. A team comprising of people from different fields establish strategies and processes to be carried out to reach the required results. This suggests that numerous environmental experts, ministries, organisations as well as legal experts must be involved.
Ministry portfolios included in the framework are:
The Environment, Climate Change, Tourism and International Trade is included because medical solid waste can impact the environment, accelerate climate change. As well as minimise inflow of tourist from other countries since solid waste deform attractiveness of the environment. In addition, no single investor is attracted by an eye sore environment, thus affecting international trade. This implies that Minister of this Portfolio should be part of medical solid waste management planners. Furthermore, Finance and Economic Development Minister is one of the key stakeholders to facilitate the planning process. This is owing to the minister’s ability to do budgets and distribute finance to development processes in the country, including finance required to improve medical solid waste management. Minister of Health and Child Care must be encompassed in planning since the cadre is responsible for monitoring all the medical facilities in Zimbabwe. This means the minister is expected to have knowledge of existing medical solid waste management approaches. Challenges which hinder adoption of sustainable strategies at hospital level are also known by the minister and Hospital Environmental Department. Minister of Higher and Tertiary Education Science and Technology Development should be part of the planners. This is because the minister has power to deploy solid waste experts from universities to deal with medical solid waste issues. Ministry of Justice Legal and Parliamentary Affairs minister and his/her legal team assist Environmental management Agency to craft legislations and laws related to medical solid waste management.
The Local Authorities who deal with solid waste from collection to disposal in urban centres are governed by Minister of Local Government and Public Works. Solid waste budgets and by-laws crafted by Local Authorities are utilised after approval from the Local Government and Public Works minister. During the planning phase, health workers who are responsible for generation of medical solid and hospital cleaners must be involved. Similarly, the community people who are vulnerable environmental health risks that emanate from poorly managed medical solid waste should be present during planning. The reason is that National Social Security Authority is responsible protecting workers from workplace injuries. Planning enables financial and other resources desired in medical solid waste management to be put together before the implementation process. In addition, stakeholders involved in the planning stage should play a pivotal role in achieving sustainable management of medical solid waste. Those who are responsible for offering training and education to health workers must play their role for instance Hospital Environmental Health Departments. Enforcement of the developed medical solid waste legislations should be carried out by Environmental Management Agency. In order to achieve objectives highlighted during planning, finance directed to medical solid management should be pumped in. Engineering issues should be implemented effectively so that medical solid waste incinerators, landfills and ottoway pits are constructed to standards. This minimises contamination of air, water and soil which emerge as a result of poorly constructed disposal structures.
During the Do phase, supplied finance should be used to purchase environmental friendly resources to be used in hospitals. This implies that medical materials which are not eco-friendly are substituted to reach sustainability. Incineration should be substituted by processes like steaming which deactivate viruses and bacteria on medical solid waste. Elimination of disposal strategies which results in high environmental pollution and risks. This can be exemplified by eliminating uncontrolled open burning and burying of medical solid. Medical facility administrations should provide enough Personal Protective Equipment to health workers and waste workers to safeguard them from health problems associated with medical solid waste. Therefore, medical facilities administration departments must safeguard wellbeing of to reduce occurrence of injuries and health problems related to medical solid waste. At this stage, participation of every individual or group of people as well as applicability of developed strategies should be evaluated through checking.
Information gathered during the implementation phase is evaluated to compare the results with the anticipated outcomes. This suggests that Checking of effectiveness of planned and implemented medical solid waste management strategies is carried out. The Checking process facilitates to figure out the changes brought by newly implemented approaches as well as areas which need further improvement. This reviewing stage enable planners to check successfulness of newly initiated medical solid waste policies and legislations. If loopholes are discovered during reviewing of invented medical solid waste management strategies, new plans can be implemented. At this stage, if non-conformity or problems are noticed in terms of medical solid waste management, apt actions or adjustments are carried out. If the implemented medical solid waste management approaches fail to meet sustainability, the barriers are investigated. Therefore, re-observing of medical solid waste management from generation to disposal is done followed by altering issues noted during planning phase as shown in Fig. 1.
Conclusion
Reviewed literature depicts that nature of medical solid waste generated in Zimbabwe encompasses pathological, sharps, pharmaceutical, chemical, radioactive, cytotoxic, infectious waste as well as general waste. Medical solid waste generation is driven by population increase which exacerbates the number of people to be dealt with at medical facilities. Moreover, outbreak and spread of various types of diseases such as HIV and AIDS, malaria, tuberculosis, Covid-19, typhoid alongside cholera increase the volumes of medical solid waste. Management of medical solid waste from point of generation to disposal shows ineffectiveness and inefficiency in Zimbabwe. This is exemplified by indiscriminate storage of sharps and other types of solid waste in single containers. Medical solid waste overloaded bins are stored in wards and corridors releasing odours to health workers, patients and visitors. Onsite conveyance of mixed medical waste is carried out using trolleys and wheel burrows while multipurpose trucks ferry medical solid waste together with general waste to offsite disposal sites. In Zimbabwe, inapt monitoring of medical solid waste is occurring owing to lack of resources, inadequate know how among those who deal with waste, non-existence of clear medical solid waste laws and policies coupled by low enforcement of environmental legislations.
Medical solid waste in Zimbabwe is transported using multipurpose vehicles and disposed in improperly engineered landfills, dumpsites, substandard incinerators as well as open burning. However, rural hospitals also utilise open pits and burying of medical solid waste in open spaces. Disposal approaches utilised compromise the quality of the environment by posing air, soil, water contamination and flora and fauna is impacted since the pollutants accumulate in the food chain. Leachates from dumpsites, ottoway pits and landfills contaminate soil and water, whereas odours and gases pollute the air. Medical solid waste affects humanity indirectly since polluted water result in gastro-intestinal problems while incineration and open burning accelerate occurrence of respiratory diseases. The study revealed that medical solid waste management system have potential to cause occupational risks for instance musculoskeletal problems like shoulder pain to those who load and offload the waste. Health workers are also vulnerable to injuries posed by sharp waste, if they handle waste without safety gear. Similarly, waste collectors, children and scavengers are under threat of injuries, pricks associated with sharp waste since they visit unsecured dumpsites. The review shows that sharp injuries expose people to different viral and bacterial diseases such as Hepatitis B, C, HIV and AIDS and tetanus. Hence, it is anticipated that the developed model may be used as a foundation to build sustainability in medical solid waste management.
Data availability statement
The data will be available from the authors on reasonable request.
References
Coker A, Sangodoyin A, Sridar M, Booth MC, Olomolayaiye C, Hammond A (2009) Medical waste management in Ibadan, Nigeria. Obstacles and prospects. Waste Manag 29(2):804–811
Hossain MS, Santhanam A, Norulaini NAN, Omar AKM (2011) Clinical solid waste management practices and its impact on human health and environment-a review. WasteManag 31:754–766
Rupani PF, Nilash M, Abumalloh RA, Asadi S, Samadi S, Wang S (2020) Corona virus pandemic (Covid-19) and its natural environmental impacts. Int J Environ Sci Technol 17:4655–4666
Vasistha P, Ganguly R, Gupta AK (2018) Biomedical waste generation and management in public sector hospital in Shimla City. Environmental pollution. Springer, Singapore, pp 225–232
Dzawanda B, Moyo GA (2022) Challenges associated with household solid waste management (SWM) during COVID-19 lockdown period: a case of ward 12 Gweru City, Zimbabwe. Environ Monit Assess 194(7):1–15
Askarian M, Heidarpoor P, Assadian OA (2010) Total quality management approach to healthcare waste management in Namazi Hospital, Iran. Waste Manag 30(11):2321–2326
Udofia EA, Niragy J (2013) Healthcare waste in Africa: a silent Crisis? Glob Health Perspex 1(1):3–10
Udofia EA, Fobil JN, Gulis G (2015) Solid waste management in Africa. Afr J of Environ Sci Technol 9(3):244–254
Ali M, Wang W, Chaudhry N, Geng Y (2017) Hospital waste management in developing countries: a mini review. Waste Manag Res 34:87–90
Haji JJ, Subramanian A, Kumar P, Ramanathan K, Rajamani A (2020) State of personal protective equipment practice in lndian intensive care units amidst covid-19 pandemic: a nationwide survey. Ind J Crit Care Med 24:409–816
Rodriguez-Morales A (2013) Current topics in public health. InTech, Rijeka
Yves Chartier JE, Pieper U, Prüss A, Rushbrook P, Stringer R, Townend W, Wilburn S, Zghondi R (2014) Safe management of wastes from health-care activities. World Health Organization (WHO)
Ramteke S, Sahu BL (2020) Novel coronavirus disease 2019 (Covid 19) pandemic: considerations for the biomedical waste sector in India. Case Stud Chem Environ Eng 2:100029
Wei G, Manyu L (2020) The hidden risks of medical waste and the COVID-19 pandemic. https://www.waste360.com/medical-waste/hidden-risks-medical-waste-and-covid-19-pandemic. Accessed 1 June 2022
World Health Organisation (2020b) Water, sanitation, hygiene, and waste management for the COVID-19 virus: in- terim guidance, World Health Organization. https://www.who.int/publications-de-tail/water-sanitation-hygiene-and-waste-management-for-covid-19
Das S, Lee SH, Kumar P, Kim KH, Lee SS (2019) Solid waste management: scope and the challenge of sustainability. J Clean Prod 228:658–678
Vivek JM, Singh R, Sutar RS, Asolekar SR (2019) Characterisation and disposal of ashes from biomedical waste incinerator. Advances in waste management. Springer, Singapore, pp 421–435
Mathur P, Patan S, Shobhawat AS (2012) Need of biomedical waste management system in hospitals-an emerging issue-a review. Curr World Environ 7(1):117
Star TD (2020) Poor medical waste management will increase infections. The Daily, Star. https://www.thedailystar.net./editorial/news
Mangizvo RV, Chinamasa R (2008) Solid medical waste management: the case of Kwekwe City in Midlands Province, Zimbabwe. J Sustain Dev Afr 10:3
Mulukuen A, Haimot G, Mesafint M (2013) Healthcare waste management practises among healthcare facilities of Gonder town, Northwest Ethiopia. Health Sci J 7(3):135–326
Omwoma S, Lalah JO, Kueppers S (2017) Technological tools for sustainable development in developing countries: the example of Africa, a review. Sustain Chem Pharm 6:67–81
Adelodun B, Ajibade FO, Ibrahim RG, Ighalo JO, Bakare HO, Kumar P, Choi KS (2021) Insights into hazardous solid waste generation during COVID-19 pandemic and sustainable management approaches for developing countries. J Mater Cycles Waste Manag 23(6):2077–2086
Saad SA (2013) Management of hospital solid waste in Khartoum state. Environ Monit Assess 185(10):8567–8582
Makwara E, Magudu S (2013) Gambling with people’s health and lives: urban solid waste management in Zimbabwe. Eur J Sustain Dev 2:67–98
Mandevere B (2015) An investigation into effectiveness of household solid waste management strategies in Harare, Zimbabwe. Published Dissertation. MSc in Environmental Management. Faculty of Environmental Management. University of South Africa, Pretoria, South Africa.
Torkashvard J, Pasari H, Jonidi-jafari A, Kermani M, Nasri O, Farzadkia M (2020) Medical waste management in Iran and comparison with neighbouring countries. Int J Environ Anal Chem 13:1–4
United Nations Development Programme (2020) Zimbabwe Country profile: healthcare waste management (HCWM) in the context of covid-19 September 2020. http://www.api.savinglivesustainably.org/documents/file/9b12951086321300c7d0721508217dd9/full/hash. Accessed 10 June 2022
Nhubu T, Muzenda E, Mbowa C, Agbenyuku E (2020) Sustainability context analysis of municipal solid waste management in Harare, Zimbabwe. Population 828:1–896
Nhubu T, Muzenda E, Muhamed B, Charles M (2021) Assessment of municipal solid waste transfer stations suitability in Harare, Zimbabwe. Adv Sci Technol Eng Syst J 6(2):1002–1012
Taru P, Kuvarega AT (2005) Solid medical waste management, the Case of Parirenyatwa Hospital, Zimbabwe. Rev Biomed 16(3):153–158
EMA (2007) Environmental management agency (hazardous waste management) regulations, 2007, statutory instrument (SI) 10 of 2007. Environmental Management Agency 2007, Harare, pp 1–68
Zimbabwe’s National Climate Change Response Strategy (2015). http://www4.unfccc.int/sites/nama/_layouts/UN/FCCC/NAMA/Download.aspx?ListName=NAMA&Id=165&FileName=Climate%20Change%20Response%20Strategy.pdf. Accessed 1 June 2022
World Bank Open Data (2021). https://data.worldbank.org. Accessed 18 May 2022
Bradley K, Ingham K (2020) Zimbabwe. Encyclopedia britannica. https://www.britannica.com/place/Zimbabwe.
Mugandani R, Wuta M, Makarau A, Chipindu B (2012) Re-classification of agro-ecological regions of Zimbabwe inconformity with climate variability and change. Afr Crop Sci J 20(2):361–369
Manyeruke C, Hamauswa S, Mhandara L (2013) The effects of climate change and variability on food security in Zimbabwe: a socio-economic and political analysis. Int J Humanit Soc Sci Vol. 3 No. 6. http://www.ijhssnet.com/journals/
Brazier A (2017) Climate change in Zimbabwe. A guide for planners and decision-makers. Konrad-Adenauer-Stiftung
Chirisa I, Nyamadzawo L, Bandauko E, Mutsindikwa N (2015) The 2008/2009 cholera outbreak in Harare, Zimbabwe: case of failure in urban environmental health and planning. Rev Environ Health 30(2):117–124
Chigudu S (2020) The political life of an epidemic: cholera, crisis, and citizenship in Zimbabwe. Cambridge University Press
Banya N (2018) Zimbabwe’s health delivery system. ZimFact. Retrieved 21 June 2022.
Nyatsanza T, Kudzai NS (2016) The usefulness of including women in household solid waste management. a case study of Dzivaresekwa high density suburb, Harare. Int J Soc Sci 21(3):92–108
Jerie S (2012) Occupational health and problems among workers in wood processing industries in Mutare, Zimbabwe. J Emerg Trends Econ Manag Sci 3(3):278–285
Sinthumule NI, Mkumbuzi SH (2019) Participation in community-based solid waste management in Nkulumane suburb, Bulawayo, Zimbabwe. Resources 8(1):30–46. https://doi.org/10.3390/resources8010030
Rahman MM, Bodrud-Doza M, Griffiths MD, Mamun MA (2020) Biomedical waste amid covid-19: perspectives from Bangladesh. Lancet Glob Health 8:E1262
Jerie S, Musasa T (2022) Solid waste management and the covid 19 pandemic lockdown in Zvishavane town, Zimbabwe. Ethiop J Environ Stud Manag 15(3):323–334
Medicines Control Authority of Zimbabwe (2020) Pharmacy guidelines for investigational medical products. Available at: https://www.mcaz.co.zw/index.php/downloads/category/15-guidelines?Download=319:pharmacy-guidelines-for-investigat-ional-medical-products.
Nyakatswau ST, Bangure D, Pierre G, Nyika H (2022) Disposal of medical waste: a legal perspective in Zimbabwe. Int J Community Med Public Health 9:2331–2333
Ansari M, Ehrampoush MH, Farzadkia M, Ahmadi O (2019) Dynamic assessment of economic and environmental performance index and generation, composition, environmental and human health risks of hospital solid waste in developing countries a state of that art of review. Environ Int 132(2019):105073
Kalogianndou K, Nikolakopoulou E, Komilis D (2018) Generation and composition of waste from medical histopathology laboratories. Waste Manag 79:435–442
Jerie S (2016) Occupational risks associated with solid waste management in the informal sector of Gweru, Zimbabwe. J Environ Public Health. https://doi.org/10.1155/902460
Nhubu T, Muzenda E (2019) Determination of the least impactful municipal solid waste management option in Harare, Zimbabwe. Processes 7:785–807
Nhubu T, Muzenda E, Mbohwa C (2019b) Impacts of waste management practices on waste resources in Harare. paper presented at the wastes: solutions, treatments and opportunities III: selected papers from the 5th international conference wastes 2019, Lisbon, Portugal, 4–6 September 2019.
World Health Organisation (2014) Safe management of wastes from healthcare activities, 2nd edn. Geneva, pp 5–6
Zimbabwe Ministry of Health (2013) National infection prevention and control guidelines. Ministry of Health and Child Care
Mahamba C (2015) Characterisation and management of non-formal solid waste management disposal sites in Harare, Zimbabwe. Published Dissertation. MSc in environmental management. Faculty of Environmental Management. University of South Africa, Pretoria, South Africa.
Makarichi L, Ka R, Jutidamrongphan W, Techato K (2018) Suitability of municipal solid waste in African cities for thermochemical wasteto-energy conversion: the case of Harare Metropolitan City, Zimbabwe. Waste Manag Res 37(1):83–94
Kwenda PR, Gareth L, Sibel E, Bas VR (2022) A mini-review on household solid waste management systems in low-income developing countries: a case study of urban Harare City, Zimbabwe. Waste Manag Res 40(2):139–153
Haregu TN, Ziraba AK, Aboderin I, Amugsi D, Muindi K, Mberu B (2017) An assessment of the evolution of Kenya’s solid waste management policies and their implementation in Nairobi and Mombasa: analysis of policies and practices. Environ Urban 29(2):515–532
Tanyanyiwa VI (2015) Not in my backyard (NIMBY)?: the accumulation of solid waste in the avenues area, Harare, Zimbabwe. Int J Innov Res Dev 4(2):122–128
Mandevere B, Jerie S (2018) Household solid waste management: how effective are the strategies used in Harare Zimbabwe. J Environ Waste Manag Recycl 2(1):29–35
Chikobvu D, Makarati F (2011) The challenges of solid waste disposal in rapidly urbanizing cities: a case of highfiel-d suburb in Harare, Zimbabwe. J Sustain Dev Afr 13:184–199
Ferreira AP, Veiga MM (2003) Hospital waste operational procedures: a case study in Brazil. Waste Manage Res 21(4):377–382
Rana R, Ganguly R, Kumar Gupta A (2017) Evaluation of solid waste management in satellite Towns of Mohali and Panchkula-India. J Solid Waste Technol Manag 43(4):280–294
Mafume N, Zendera W, Mutetwa M (2016) Challenges of solid waste management in Zimbabwe: a case study of Sakubva high density suburb. J Environ Waste Manag 3:142–155
Jerie S, Zulu S (2017) Site suitability analysis for solid waste landfill site location using geographic information systems and remote sensing. A case study of Banket Town Board. Zimbabwe. Rev Social 2:19–31
Chapungu L, Zinhiva H, Marange E (2015) Assessment of domestic solid waste management systems in rural district services centres: the case of Ngangu residential area in Chimanimani District, Zimbabwe. J Solid Waste Technol Manag 41:96–105
Munyai O, Nunu WN (2020) Health effects associated with proximity to waste collection points in Beitbridge Municipality, Zimbabwe. Waste Manage 105:501–510
Federation of Red Cross and Red Crescent (2010) Zimbabwe: cholera emergency appeal. Retrieved from: http://reliefweb.int/node/345114
Chanza N, Gundu-Jakarasi V (2020) Deciphering the climate change conundrum in Zimbabwe: an exposition. Global warming and climate change. IntechOpen
Heera S, Rajor A (2014) Bacterial treatment and metal characterization of biomedical waste ash. J Waste Manag. https://doi.org/10.1155/2014/956316
Luo H, Cheng Y, He D, Yang EH (2019) Review of leaching behavior of municipal solid waste incineration (MSWI) ash. Sci Total Environ 668:90–103
Shi P, Schulin R (2018) Erosion-induced losses of carbon, nitrogen, phosphorus and heavy metals from agricultural soils of contrasting organic matter management. Sci Total Environ 618:210–218. https://doi.org/10.1016/j.scitotenv.2017.11.060
Chatsiwa J (2015) Land pollution and population density: the case of Kwekwe City residential areas, Zimbabwe (Doctoral dissertation).
World Health Organisation (2018) Healthcare waste. Available at https.//www.who.int/news/room/factsheets/detail/healthcare waste. Accessed 15 July 2022.
Nyoni M (2020) Covid 19: the huge threat to Zimbabwe’s economy. Available at https://www.thestandard.co.zw/202.covid-19-huge-threatzimbabwes-economy.
Chikombe S (2017) Occupational safety and health hazards associated with solid waste management in Bindura, Zimbabwe. Masters Thesis. Midlands State University. Available at http://www.ir.msu.ac.zw:8080/jspui/bitstream/11408/2993/1/FINAL%20DISSERTATION%20SHUVAI%20C
Njaya T (2016) An evaluation of income disparities between male and female street vendors of Harare in Zimbabwe. J Study Soc Sci Humanit 2:106–114
Nemadire S, Mapurazi S, Nyamadzawo G (2017) Formalising informal solid waste recycling at the Pomona dumpsite in Harare, Zimbabwe. Nat Res Forum 41:176–178
Ghafuri Y, Shiri R, Jafari NA, Izanloo H (2020) Risk characterization and quantification of medical waste in Qom Province. J Environ Treat Tech 8(2):634–638
United Nations General Assembly (2015) Transforming our world: the 2030 agenda for sustainable development. United Nations; 2015. http://www.un.org/ga/.
Zimbabwean Government (2018) Statutory instrument. 268 of 2018. Harare: government printer. Available at https://www.ema.co.zw/index.php/agency/downloads/file/Statutory%20Instruments/S.%20I.%20268%20of%202018%20Environmental%20Management%20Hazardous%20Sub.pdf. Accessed 7 July 2022.
Zimbabwean Government (2013) Constitution of Zimbabwe, No. 20 of 2013. Harare: Government Printer. Available at: https://www.parlzim.gov.zw/component/k2/download/1290_da9279a81557040d47c3a2c27012f6e. Accessed 1 July 2022. Management issues in Beitbridge border town: evidence from a participatory research.
de Gobbi M (2020) Environmental integrity and doing business in Zimbabwe challenges and engagement of sustainable enterprises. Proc Environ Sci 35:176–184. https://doi.org/10.1016/j.proenv.2016.07.073
Ministry of Local Government and Public Works (2021) Section 229 of the Urban Council Act Chapter 29:15
Zimbabwean Government (1996) Factories and works act (Chap 14:08). Government Printer. Available at: https://www.nssa.org.zw/uncategorized/factories-works-act-ensures-workers-safety/. Accessed 1 July 2022.
Moen R, Norman C (2009) Evolution of the PDCA cycle (PDF). Westga.edu. Paper delivered to the Asian Network for Quality Conference in Tokyo on September 17, 2009. Retrieved 14 June 2022.
Dubberly H (2008) [2004]. How do you design? A compendium of models. Dubberly.com. Retrieved 21 Dec 2017
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Takunda, S., Steven, J. Medical solid waste management status in Zimbabwe. J Mater Cycles Waste Manag 25, 717–732 (2023). https://doi.org/10.1007/s10163-022-01578-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10163-022-01578-4