Abstract
In advancing our understanding of tinnitus, some of the more impactful contributions in the past two decades have come from human brain imaging studies, specifically the idea of both auditory and extra-auditory neural networks that mediate tinnitus. These networks subserve both the perception of tinnitus and the psychological reaction to chronic, continuous tinnitus. In this article, we review particular studies that report on the nodes and links of such neural networks and their inter-network connections. Innovative neuroimaging tools have contributed significantly to the increased understanding of anatomical and functional connections of attention, emotion-processing, and default mode networks in adults with tinnitus. We differentiate between the neural correlates of tinnitus and those of comorbid hearing loss; surprisingly, tinnitus and hearing loss when they co-occur are not necessarily additive in their impact and, in rare cases, additional tinnitus may act to mitigate the consequences of hearing loss alone on the brain. The scale of tinnitus severity also appears to have an impact on brain networks, with some of the alterations typically attributed to tinnitus reaching significance only in the case of bothersome tinnitus. As we learn more about comorbid conditions of tinnitus, such as depression, anxiety, hyperacusis, or even aging, their contributions to the network-level changes observed in tinnitus will need to be parsed out in a manner similar to what is currently being done for hearing loss or severity. Together, such studies advance our understanding of the heterogeneity of tinnitus and will lead to individualized treatment plans.


Similar content being viewed by others
References
Jarach CM, Lugo A, Scala M et al (2022) Global prevalence and incidence of tinnitus: a systematic review and meta-analysis. JAMA Neurol 79(9):888–900. https://doi.org/10.1001/jamaneurol.2022.2189
Henry JA, Griest S, Austin D, Helt W, Gordon J, Thielman E, Carlson K (2016) Tinnitus screener: results from the first 100 participants in an epidemiology study. Am J Audiol 25(2):153–160
Henry JA (2016) “Measurement” of tinnitus. Otol Neurotol 37(8):e276–e285
Eggermont JJ (2013) Hearing loss, hyperacusis, or tinnitus: what is modeled in animal research? Hear Res 295:140–149
Lobarinas E, Hayes SH, Allman BL (2013) The gap-startle paradigm for tinnitus screening in animal models: limitations and optimization. Hear Res 295:150–160
Melcher JR, Sigalovsky IS, Guinan JJ Jr, Levine RA (2000) Lateralized tinnitus studied with functional magnetic resonance imaging: abnormal inferior colliculus activation. J Neurophysiol 83(2):1058–1072
Melcher JR, Levine RA, Bergevin C, Norris B (2009) The auditory midbrain of people with tinnitus: abnormal sound-evoked activity revisited. Hear Res 257(1–2):63–74
Wienbruch C, Paul I, Weisz N, Elbert T, Roberts LE (2006) Frequency organization of the 40-Hz auditory steady-state response in normal hearing and in tinnitus. Neuroimage 33(1):180–194
Mühlnickel W, Elbert T, Taub E, Flor H (1998) Reorganization of auditory cortex in tinnitus. Proc Natl Acad Sci 95(17):10340–10343
Manning C, Thielman EJ, Grush L, Henry JA (2019) Perception versus reaction: comparison of tinnitus psychoacoustic measures and Tinnitus Functional Index scores. Am J Audiol 28:174–180. https://doi.org/10.1044/2018_AJA-TTR17-18-0041
Tyler R, Coelho C, Tao P, Ji H, Noble W, Gehringer A, Gogel S (2008) Identifying tinnitus subgroups with cluster analysis. Am J Audiol 17(2):S176–S184. https://doi.org/10.1044/1059-0889(2008/07-0044)
Kochkin S, Tyler R (2008) Tinnitus treatment and the effectiveness of hearing aids: hearing care professional perceptions. Hear Rev 15(13):14–18
Unterrainer J, Greimel KV, Leibetseder M, Koller T (2009) Experiencing tinnitus: which factors are important for perceived severity of the symptom? Int Tinnitus J 9:130–133
Bartels H, Middel BL, van der Laan BF, Staal MJ, Albers FW (2008) The additive effect of co-occurring anxiety and depression on health status, quality of life and coping strategies in help-seeking tinnitus sufferers. Ear Hear 29(6):947–956
Husain FT (2020) Perception of, and reaction to, tinnitus: the depression factor. Otolaryngol Clin North Am 53(4):555–561
Hallam RS, Jakes SC, Hinchcliffe R (1988) Cognitive variables in tinnitus annoyance. Br J Clin Psychol 27(3):213–222
Newman CW, Jacobson GP, Spitzer JB (1996) Development of the tinnitus handicap inventory. Arch Otolaryngol Head Neck Surg 122(2):143–148
Meikle MB, Henry JA, Griest SE, Stewart BJ, Abrams HB, McArdle R et al (2012) The tinnitus functional index: development of a new clinical measure for chronic, intrusive tinnitus. Ear Hear 33(2):153–176
Tyler R, Ji H, Perreau A, Witt S, Noble W, Coelho C (2014) Development and validation of the tinnitus primary function questionnaire. Am J Audiol 23(3):260–272
Cederroth CR, Lugo A, Edvall NK, Lazar A, Lopez-Escamez JA, Bulla J, Gallus S (2020) Association between hyperacusis and tinnitus. J Clin Med 9(8):2412
Clifford RE, Ryan AF (2022) The interrelationship of tinnitus and hearing loss secondary to age, noise exposure, and traumatic brain injury. Ear Hear 43(4):1114–1124
Moring JC, Resick PA, Peterson AL, Husain FT, Esquivel C, Young-McCaughan S, Granato E, Fox PT; STRONG STAR Consortium (2022) Treatment of posttraumatic stress disorder alleviates tinnitus-related distress among veterans: a pilot study. Am J Audiol 31(4):1293–1298
Moring JC, Peterson AL, Kanzler KE (2018) Tinnitus, traumatic brain injury, and posttraumatic stress disorder in the military. Int J Behav Med 25:312–321
Carpenter-Thompson JR, Schmidt S, McAuley E, Husain FT (2015) Increased frontal response may underlie decreased tinnitus severity. PLoS ONE 10(12):e0144419
Boyen K, de Kleine E, van Dijk P, Langers DR (2014) Tinnitus-related dissociation between cortical and subcortical neural activity in humans with mild to moderate sensorineural hearing loss. Hear Res 312:48–59
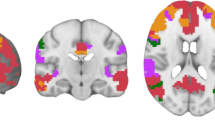
Schmidt SA, Akrofi K, Carpenter-Thompson JR, Husain FT (2013) Default mode, dorsal attention and auditory resting state networks exhibit differential functional connectivity in tinnitus and hearing loss. PLoS ONE 8(10):e76488
Husain FT, Zimmerman B, Tai Y, Finnegan MK, Kay E, Khan F, Gobin RL (2019) Assessing mindfulness-based cognitive therapy intervention for tinnitus using behavioural measures and structural MRI: a pilot study. Int J Audiol 58(12):889–901
Baliyan V, Das CJ, Sharma R, Gupta AK (2016) Diffusion weighted imaging: technique and applications. World J Radiol 8(9):785–789
Soares JM, Marques P, Alves V, Sousa N (2013) A hitchhiker’s guide to diffusion tensor imaging. Front Neurosci 7:31
Raffelt DA, Tournier JD, Smith RE, Vaughan DN, Jackson G, Ridgway GR, Connelly A (2017) Investigating white matter fibre density and morphology using fixel-based analysis. Neuroimage 144:58–73
Peelle JE, Troiani V, Grossman M, Wingfield A (2011) Hearing loss in older adults affects neural systems supporting speech comprehension. J Neurosci 31(35):12638–12643
Eckert MA, Cute SL, Vaden KI, Kuchinsky SE, Dubno JR (2012) Auditory cortex signs of age-related hearing loss. J Assoc Res Otolaryngol 13:703–713
Yang M, Chen HJ, Liu B, Huang ZC, Feng Y, Li J, Teng GJ (2014) Brain structural and functional alterations in patients with unilateral hearing loss. Hear Res 316:37–43
Qi R, Su L, Zou L, Yang J, Zheng S (2019) Altered gray matter volume and white matter integrity in sensorineural hearing loss patients: a VBM and TBSS study. Otol Neurotol 40(6):e569–e574
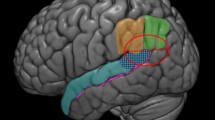
Husain FT, Medina RE, Davis CW, Szymko-Bennett Y, Simonyan K, Pajor NM, Horwitz B (2011) Neuroanatomical changes due to hearing loss and chronic tinnitus: a combined VBM and DTI study. Brain Res 1369:74–88
Koops EA, de Kleine E, van Dijk P (2020) Gray matter declines with age and hearing loss, but is partially maintained in tinnitus. Sci Rep 10(1):21801
Boyen K, Langers DR, de Kleine E, van Dijk P (2013) Gray matter in the brain: differences associated with tinnitus and hearing loss. Hear Res 295:67–78
Shahsavarani S, Khan RA, Husain FT (2019) Tinnitus and the brain: a review of functional and anatomical magnetic resonance imaging studies. Perspect ASHA SIGs 4(5):896–909
Mühlau M, Rauschecker JP, Oestreicher E, Gaser C, Röttinger M, Wohlschläger AM, Simon F, Etgen T, Conrad B, Sander D (2006) Structural brain changes in tinnitus. Cereb Cortex 16(9):1283–1288
Leaver AM, Renier L, Chevillet MA, Morgan S, Kim HJ, Rauschecker JP (2011) Dysregulation of limbic and auditory networks in tinnitus. Neuron 69(1):33–43
Schecklmann M, Lehner A, Poeppl TB, Kreuzer PM, Rupprecht R, Rackl J, Burger J, Frank E, Hajak G, Langguth B, Landgrebe M (2013) Auditory cortex is implicated in tinnitus distress: a voxel-based morphometry study. Brain Struct Funct 218:1061–1070
Landgrebe M, Langguth B, Rosengarth K, Braun S, Koch A, Kleinjung T, May A, de Ridder D, Hajak G (2009) Structural brain changes in tinnitus: grey matter decrease in auditory and non-auditory brain areas. Neuroimage 46(1):213–218
Melcher JR, Knudson IM, Levine RA (2013) Subcallosal brain structure: correlation with hearing threshold at supra-clinical frequencies (> 8 kHz), but not with tinnitus. Hear Res 295:79–86
Vanneste S, Van De Heyning P, De Ridder D (2015) Tinnitus: a large VBM-EEG correlational study. PLoS ONE 10(3):e0115122
Makani P, Thioux M, Pyott SJ, van Dijk P (2022) A combined image- and coordinate-based meta-analysis of whole-brain voxel-based morphometry studies investigating subjective tinnitus. Brain Sci 12(9):1192. https://doi.org/10.3390/brainsci12091192
Tarabichi O, Kozin ED, Kanumuri VV, Barber S, Ghosh S, Sitek KR, Reinshagen K, Herrmann B, Remenschneider AK, Lee DJ (2018) Diffusion tensor imaging of central auditory pathways in patients with sensorineural hearing loss: a systematic review. Otolaryngol Head Neck Surg 158(3):432–442
Huang L, Zheng W, Wu C, Wei X, Wu X, Wang Y, Zheng H (2015) Diffusion tensor imaging of the auditory neural pathway for clinical outcome of cochlear implantation in pediatric congenital sensorineural hearing loss patients. PLoS ONE 10(10):e0140643
Lin Y, Wang J, Wu C, Wai Y, Yu J, Ng S (2008) Diffusion tensor imaging of the auditory pathway in sensorineural hearing loss: changes in radial diffusivity and diffusion anisotropy. J Magn Reson Imaging 28(3):598–603
Rigters SC, Cremers LG, Ikram MA, van der Schroeff MP, de Groot M, Roshchupkin GV, Niessen WJN, Baatenburg de Jong RJ, Goedegebure A, Vernooij MW (2018) White-matter microstructure and hearing acuity in older adults: a population-based cross-sectional DTI study. Neurobiol Aging 61:124–131
Lee YJ, Bae SJ, Lee SH, Lee JJ, Lee KY, Kim MN, Chang Y (2007) Evaluation of white matter structures in patients with tinnitus using diffusion tensor imaging. J Clin Neurosci 14(6):515–519
Aldhafeeri FM, Mackenzie I, Kay T, Alghamdi J, Sluming V (2012) Neuroanatomical correlates of tinnitus revealed by cortical thickness analysis and diffusion tensor imaging. Neuroradiology 54:883–892
Khan RA, Sutton BP, Tai Y, Schmidt SA, Shahsavarani S, Husain FT (2021) A large-scale diffusion imaging study of tinnitus and hearing loss. Sci Rep 11(1):23395
Chen Q, Wang Z, Lv H, Zhao P, Yang Z, Gong S, Wang Z (2020) Reorganization of brain white matter in persistent idiopathic tinnitus patients without hearing loss: evidence from baseline data. Front Neurosci 14:591
Gunbey HP, Gunbey E, Aslan K, Bulut T, Unal A, Incesu L (2017) Limbic-auditory interactions of tinnitus: an evaluation using diffusion tensor imaging. Clin Neuroradiol 27:221–230
Crippa A, Lanting CP, van Dijk P, Roerdink JB (2010) A diffusion tensor imaging study on the auditory system and tinnitus. Open Neuroimag J 4:16–25. https://doi.org/10.2174/1874440001004010016 (PMID: 20922048; PMCID: PMC2948149)
Seydell-Greenwald A, Raven EP, Leaver AM, Turesky TK, Rauschecker JP (2014) Diffusion imaging of auditory and auditory-limbic connectivity in tinnitus: preliminary evidence and methodological challenges. Neural Plast 2014:145943
Benson RR, Gattu R, Cacace AT (2014) Left hemisphere fractional anisotropy increase in noise-induced tinnitus: a diffusion tensor imaging (DTI) study of white matter tracts in the brain. Hear Res 309:8–16
Ryu CW, Park MS, Byun JY, Jahng GH, Park S (2016) White matter integrity associated with clinical symptoms in tinnitus patients: a tract-based spatial statistics study. Eur Radiol 26:2223–2232
Schmidt SA, Zimmerman B, Medina ROB, Carpenter-Thompson JR, Husain FT (2018) Changes in gray and white matter in subgroups within the tinnitus population. Brain Res 1679:64–74
Koops EA, Haykal S, van Dijk P (2021) Macrostructural changes of the acoustic radiation in humans with hearing loss and tinnitus revealed with fixel-based analysis. J Neurosci 41(18):3958–3965
Jacobson GP, McCaslin DL (2003) A reexamination of the long latency N1 response in patients with tinnitus. J Am Acad Audiol 14(07):393–400
Melcher JR (2012) Human brain imaging of tinnitus. In: Eggermont J, Zeng FG, Popper A, Fay R (eds) Tinnitus. Springer Handbook of Auditory Research, vol 44. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-3728-4_8
Piarulli A, Vanneste S, Nemirovsky IE, Kandeepan S, Maudoux A, Gemignani A, De Ridder D, Soddu A (2023) Tinnitus and distress: an electroencephalography classification study. Brain Commun 5(1):fcad018
Adjamian P (2014) The application of electro-and magneto-encephalography in tinnitus research–methods and interpretations. Front Neurol 5:228
Mirz F (2000) Cortical networks subserving the perception of tinnitus-a PET study. Acta Otolaryngol 120(543):241–243
Mirz F, Gjedde A, Sdkilde-Jrgensen H, Pedersen CB (2000) Functional brain imaging of tinnitus-like perception induced by aversive auditory stimuli. NeuroReport 11(3):633–637
Carpenter-Thompson JR, Akrofi K, Schmidt SA, Dolcos F, Husain FT (2014) Alterations of the emotional processing system may underlie preserved rapid reaction time in tinnitus. Brain Res 1567:28–41
Bradley MM, Lang PJ (2007) The International Affective Digitized Sounds (IADS-2): Affective ratings of sounds and instruction manual. Tech Rep B-3. University of Florida, Gainesville, FL
Khan RA, Husain FT (2020) Tinnitus and cognition: can load theory help us refine our understanding? Laryngoscope Investig Otolaryngol 5(6):1197–1204
Schmidt SA, Shahsavarani S, Khan RA, Tai Y, Granato EC, Willson CM et al (2023) An examination of the reliability of seed-to-seed resting state functional connectivity in tinnitus patients. Neuroimage Rep 3(1):100158
Kok TE, Domingo D, Hassan J, Vuong A, Hordacre B, Clark C, Shekhawat GS (2022) Resting-state networks in tinnitus: a scoping review. Clin Neuroradiol 32(4):903–922
Arnold W, Bartenstein P, Oestreicher E, Römer W, Schwaiger M (1996) Focal metabolic activation in the predominant left auditory cortex in patients suffering from tinnitus: a PET study with [18F] deoxyglucose. ORL J Otorhinolaryngol Relat Spec 58(4):195–199
Geven LI, De Kleine E, Willemsen ATM, Van Dijk P (2014) Asymmetry in primary auditory cortex activity in tinnitus patients and controls. Neuroscience 256:117–125
Langguth B, Eichhammer P, Kreutzer A, Maenner P, Marienhagen J, Kleinjung T, Hajak G (2006) The impact of auditory cortex activity on characterizing and treating patients with chronic tinnitus–first results from a PET study. Acta Otolaryngol 126(sup556):84–88
Schecklmann M, Landgrebe M, Poeppl TB, Kreuzer P, Männer P, Marienhagen J, Langguth B (2013) Neural correlates of tinnitus duration and distress: a positron emission tomography study. Hum Brain Mapp 34(1):233–240
Zimmerman BJ, Schmidt SA, Khan RA, Tai Y, Shahsavarani S, Husain FT (2021) Decreased resting perfusion in precuneus and posterior cingulate cortex predicts tinnitus severity. Curr Res Neurobiol 2:100010
Moring JC, Husain FT, Gray J, Franklin C, Peterson AL, Resick PA, Garrett A, Esquivel C, Fox PT (2022) Invariant structural and functional brain regions associated with tinnitus: A meta-analysis. PLoS ONE 17(10):e0276140
Fransson P (2005) Spontaneous low-frequency BOLD signal fluctuations: An fMRI investigation of the resting-state default mode of brain function hypothesis. Hum Brain Mapp 26(1):15–29
Sridharan D, Levitin DJ, Menon V (2008) A critical role for the right fronto-insular cortex in switching between central-executive and default-mode networks. Proc Natl Acad Sci 105(34):12569–12574
De Ridder D, Elgoyhen AB, Romo R, Langguth B (2011) Phantom percepts: tinnitus and pain as persisting aversive memory networks. Proc Natl Acad Sci 108(20):8075–8080
Elgoyhen AB, Langguth B, De Ridder D, Vanneste S (2015) Tinnitus: perspectives from human neuroimaging. Nat Rev Neurosci 16(10):632–642
Shahsavarani S, Schmidt SA, Khan RA, Tai Y, Husain FT (2021) Salience, emotion, and attention: the neural networks underlying tinnitus distress revealed using music and rest. Brain Res 1755:147277
De Ridder D, Vanneste S, Song JJ, Adhia D (2022) Tinnitus and the triple network model: a perspective. Clin Exp Otorhinolaryngol 15(3):205–212
Simonetti P, Ono CR, de Godoi Carneiro C, Khan RA, Shahsavarani S, Husain FT, Oiticica J (2022) Evaluating the efficacy of hearing aids for tinnitus therapy–a positron emission tomography study. Brain Res 1775:147728
Krick CM, Grapp M, Daneshvar-Talebi J, Reith W, Plinkert PK, Bolay HV (2015) Cortical reorganization in recent-onset tinnitus patients by the Heidelberg Model of Music Therapy. Front Neurosci 9:49
Krick CM, Argstatter H, Grapp M, Plinkert PK, Reith W (2017) Heidelberg neuro-music therapy enhances task-negative activity in tinnitus patients. Front Neurosci 11:384
McKenna L, Marks EM, Hallsworth CA, Schaette R (2017) Mindfulness-based cognitive therapy as a treatment for chronic tinnitus: a randomized controlled trial. Psychother Psychosom 86(6):351–361
McKenna L, Marks EM, Vogt F (2018) Mindfulness-based cognitive therapy for chronic tinnitus: evaluation of benefits in a large sample of patients attending a tinnitus clinic. Ear Hear 39(2):359–366
Philippot P, Nef F, Clauw L, de Romrée M, Segal Z (2012) A randomized controlled trial of mindfulness-based cognitive therapy for treating tinnitus. Clin Psychol Psychother 19(5):411–419
Roland LT, Lenze EJ, Hardin FM, Kallogjeri D, Nicklaus J, Wineland AM, Piccirillo JF (2015) Effects of mindfulness based stress reduction therapy on subjective bother and neural connectivity in chronic tinnitus. Otolaryngol Head Neck Surg 152(5):919–926
Zimmerman B, Finnegan M, Paul S, Schmidt S, Tai Y, Roth K, Husain FT (2019) Functional brain changes during mindfulness-based cognitive therapy associated with tinnitus severity. Front Neurosci 13:747
Kleinjung T, Steffens T, Londero A, Langguth B (2007) Transcranial magnetic stimulation (TMS) for treatment of chronic tinnitus: clinical effects. Prog Brain Res 166:359–551
Poeppl TB, Langguth B, Lehner A, Frodl T, Rupprecht R, Kreuzer PM, Schecklmann M (2018) Brain stimulation-induced neuroplasticity underlying therapeutic response in phantom sounds. Hum Brain Mapp 39(1):554–562
Hamza Y, Zeng FG (2021) Tinnitus is associated with improved cognitive performance in non-Hispanic elderly with hearing loss. Front Neurosci 15:735950
Ivansic D, Guntinas-Lichius O, Müller B, Volk GF, Schneider G, Dobel C (2017) Impairments of speech comprehension in patients with tinnitus—a review. Front Aging Neurosci 9:224
Zeng FG, Richardson M, Turner K (2020) Tinnitus does not interfere with auditory and speech perception. J Neurosci 40(31):6007–6017
Oosterloo BC, Homans NC, Goedegebure A (2020) Tinnitus affects speech in noise comprehension in individuals with hearing loss. Otol Neurotol 41(9):e1074–e1081
Tai Y, Shahsavarani S, Khan RA et al (2023) An inverse relationship between gray matter volume and speech-in-noise performance in tinnitus patients with normal hearing sensitivity. JARO 24:385–395. https://doi.org/10.1007/s10162-023-00895-1
Husain FT, Akrofi K, Carpenter-Thompson JR, Schmidt SA (2015) Alterations to the attention system in adults with tinnitus are modality specific. Brain Res 1620:81–97
Husain FT, Pajor NM, Smith JF, Kim HJ, Rudy S, Zalewski C, Horwitz B (2011) Discrimination task reveals differences in neural bases of tinnitus and hearing impairment. PLoS ONE 6(10):e26639
Tai Y, Husain FT (2019) The role of cognitive control in tinnitus and its relation to speech-in-noise performance. J Audiol Otol 23(1):1–7
Sharma A, Mohanty M, Panda N, Munjal S (2023) Neuropsychological differences between the unilateral and bilateral tinnitus participants with normal hearing. Folia Phoniatr Logop 75(2):67–80
Roberts LE, Eggermont JJ, Caspary DM, Shore SE, Melcher JR, Kaltenbach JA (2010) Ringing ears: the neuroscience of tinnitus. J Neurosci 30(45):14972–14979
Schaette R (2014) Tinnitus in men, mice (as well as other rodents), and machines. Hear Res 311:63–71
Eggermont JJ, Roberts LE (2004) The neuroscience of tinnitus. Trends Neurosci 27(11):676–682
Baguley D, McFerran D, Hall D (2013) Tinnitus. Lancet 382(9904):1600–1607
Koops EA, Eggermont JJ (2021) The thalamus and tinnitus: bridging the gap between animal data and findings in humans. Hear Res 407:108280
Schmidt SA, Carpenter-Thompson J, Husain FT (2017) Connectivity of precuneus to the default mode and dorsal attention networks: a possible invariant marker of long-term tinnitus. NeuroImage Clin 16:196–204
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflict of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Husain, F.T., Khan, R.A. Review and Perspective on Brain Bases of Tinnitus. JARO 24, 549–562 (2023). https://doi.org/10.1007/s10162-023-00914-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10162-023-00914-1