Abstract
Background
Limited direct comparative studies exist in terms of the effects of sodium-glucose cotransporter 2 inhibitors (SGLT2is) and dipeptidyl peptidase-4 inhibitors (DPP4is) on the kidney outcomes in Japanese individuals with type 2 diabetes.
Methods
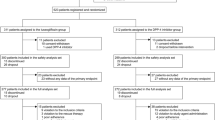
This retrospective cohort study included 561 Japanese adults with type 2 diabetes, who were newly prescribed either an SGLT2i or a DPP4i and had an eGFR ≥ 30 mL/min/1.73 m2. The cohort comprised 207 women and 354 men, with a mean (± standard deviation) age of 63 (± 12) years. The exposure and outcome were SGLT2i or DPP4i initiation and eGFR slope during the overall follow-up period, restricted to participants who were followed for ≥2 years. We adopted the on-treatment analysis. Analysis of covariance was used to compare the adjusted eGFR slope between the two groups, incorporating 10 variables at baseline.
Results
During the median follow-up period of 3.4 years, least square mean (95% CI) eGFR slopes were −1.91 (−2.15, −1.67) and −1.12 (−1.58, −0.67) mL/min/1.73 m2/year in individuals treated with a DPP4i (n = 460) and an SGLT2i (n = 101), respectively, demonstrating statistical significance (p = 0.002). The robustness of this finding was strengthened by sensitivity analyses.
Conclusions
This study provides potential evidence of the superiority of SGLT2is over DPP4is in slowing kidney function decline in Japanese adults with type 2 diabetes and eGFR ≥ 30 mL/min/1.73 m2.

Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Wanner C, Inzucchi SE, Lachin JM, et al. Empagliflozin and progression of kidney disease in type 2 diabetes. N Engl J Med. 2016;375:323–34.
Perkovic V, de Zeeuw D, Mahaffey KW, et al. Canagliflozin and renal outcomes in type 2 diabetes: results from the CANVAS Program randomised clinical trials. Lancet Diabetes Endocrinol. 2018;6:691–704.
Wiviott SD, Raz I, Bonaca MP, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2019;380:347–57.
Fox CS, Matsushita K, Woodward M, et al. Associations of kidney disease measures with mortality and end-stage renal disease in individuals with and without diabetes: a meta-analysis. Lancet. 2012;380:1662–73.
Masakane I, Nakai S, Ogata S, et al. An Overview of regular dialysis treatment in Japan (As of 31 December 2013). Ther Apher Dial. 2015;19:540–74.
GBD Chronic Kidney Disease Collaboration. Global, regional and national burden of chronic kidney disease, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2020;395:709–33.
American Diabetes Association Professional Practice Committee. 11. Chronic kidney disease and risk management: standards of care in diabetes-2024. Diabetes Care. 2024;47(Suppl 1):S219–30.
Perkovic V, Jardine MJ, Neal B, et al. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med. 2019;380:2295–306.
Heerspink HJL, Stefánsson BV, Correa-Rotter R, et al. Dapagliflozin in patients with chronic kidney disease. N Engl J Med. 2020;383:1436–46.
Heerspink HJL, Karasik A, Thuresson M, et al. Kidney outcomes associated with use of SGLT2 inhibitors in real-world clinical practice (CVD-REAL 3): a multinational observational cohort study. Lancet Diabetes Endocrinol. 2020;8:27–35.
Xie Y, Bowe B, Gibson AK. Comparative effectiveness of the sodium-glucose cotransporter 2 inhibitor empagliflozin versus other antihyperglycemics on risk of major adverse kidney events. Diabetes Care. 2020;43:2785–95.
Schechter M, Melzer-Cohen C, Rozenberg A, et al. Cardiorenal outcomes with sodium/glucose cotransporter-2 inhibitors in patients with type 2 diabetes and low kidney risk: real world evidence. Cardiovasc Diabetol. 2021;20:169.
Nagasu H, Yano Y, Kanegae H. Kidney outcomes associated with SGLT2 inhibitors versus other glucose-lowering drugs in real-world clinical practice: the Japan chronic kidney disease database. Diabetes Care. 2021;44:2542–51.
Mardetko N, Nabergoj Makovec U, Locatelli I, Janez A, Kos M. Uptake of new antidiabetic medicines in 11 European countries. BMC Endocr Disord. 2021;21:127.
Fang M, Wang D, Coresh J, Selvin E. Trends in diabetes treatment and control in U.S. adults, 1999–2018. N Engl J Med. 2021;384:2219–28.
Yagi N, Komiya I, Arai K, et al. Current status of oral antidiabetic drug prescribing patterns based on the body mass index for Japanese type 2 diabetes mellitus patients and yearly changes in diabetologists’ prescribing patterns from 2002 to 2019 (JDDM61). J Diabetes Investig. 2022;13:65–73.
American Diabetes Association Professional Practice Committee. 10. Cardiovascular disease and risk management: standards of care in diabetes-2024. Diabetes Care. 2024;47(Suppl 1): S179–218.
Mosenzon O, Leibowitz G, Bhatt DL, et al. Effect of saxagliptin on renal outcomes in the SAVOR-TIMI 53 trial. Diabetes Care. 2017;40:69–76.
Kidney Disease: Improving Global Outcomes (KDIGO) Diabetes Work Group. KDIGO 2022 clinical practice guideline for diabetes management in chronic kidney Disease. Kidney Int. 2022;102(5S):S1–127.
de Boer IH, Khunti K, Sadusky T, et al. Diabetes management in chronic kidney disease: a consensus report by the american diabetes association (ADA) and kidney disease: improving global outcomes (KDIGO). Diabetes Care. 2022;45:3075–90.
Birkeland KI, Bodegard J, Banerjee A, et al. Lower cardiorenal risk with sodium-glucose cotransporter-2 inhibitors versus dipeptidyl peptidase-4 inhibitors in patients with type 2 diabetes without cardiovascular and renal diseases: A large multinational observational study. Diabetes Obes Metab. 2021;23:75–85.
Matsuo S, Imai E, Horio M, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92.
Levey AS, Gansevoort RT, Coresh J, et al. Change in albuminuria and GFR as end points for clinical trials in early stages of CKD: a scientific workshop sponsored by the national kidney foundation in collaboration with the US food and drug administration and European medicines agency. Am J Kidney Dis. 2020;75:84–104.
Itano S, Kanda E, Nagasu H, Nangaku M, Kashihara N. eGFR slope as a surrogate endpoint for clinical study in early stage of chronic kidney disease: from The Japan Chronic Kidney Disease Database. Clin Exp Nephrol. 2023;27:847–56.
Stuart EA. Matching methods for causal inference: a review and a look forward. Stat Sci. 2010;25:1–21.
Au PCM, Tan KCB, Cheung BMY, Wong ICK, Li HL, Cheung CL. Association between SGLT2 inhibitors vs DPP4 inhibitors and renal outcomes among patients with type 2 diabetes. J Clin Endocrinol Metab. 2022;107:e2962–70.
Cohen CM, Schechter M, Rozenberg M, et al. Long-term, real-world kidney outcomes with SGLT2i versus DPP4i in type 2 diabetes without cardiovascular or kidney disease. Clin J Am Soc Nephrol. 2023;18:1153–62.
Pasternak B, Wintzell V, Melbye M, et al. Use of sodium-glucose co-transporter 2 inhibitors and risk of serious renal events: Scandinavian cohort study. BMJ. 2020;369:m1186.
Idris I, Zhang R, Mamza JB, et al. Significant reduction in chronic kidney disease progression with sodium-glucose cotransporter-2 inhibitors compared to dipeptidyl peptidase-4 inhibitors in adults with type 2 diabetes in a UK clinical setting: an observational outcomes study based on international guidelines for kidney disease. Diabetes Obes Metab. 2022;24:2138–47.
Mosenzon O, Raz I, Wiviott SD, et al. Dapagliflozin and prevention of kidney disease among patients with type 2 diabetes: post hoc analyses from the DECLARE-TIMI 58 trial. Diabetes Care. 2022;45:2350–9.
Acknowledgements
We would like to thank Honyaku Center Inc. for English language editing.
Funding
We have not received any funding for the present study.
Author information
Authors and Affiliations
Contributions
All authors contributed to the conception and design of the study. NY and KH contributed to the data collection and preparation. KH contributed to the analysis and interpretation of data. NY and KH were responsible for drafting the manuscript. All authors revised the manuscript. All authors have approved the final version of the manuscript. TB is the guarantor of this work, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Conflicts of interest
The authors have nothing to disclose.
Ethical approval
All procedures performed in the present study were in accordance with the ethical standards of the institutional research committee of Tokyo Women’s Medical University School of Medicine (approval no. 3932) and with the tenets of the Declaration of Helsinki of 1964 and its later versions.
Informed consent
As the present study was an observational and historical but not a prospective interventional study, the ethics committee waived the need for direct informed consent. Instead, we offered participants the opportunity to opt-out to participate.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Yoshida, N., Hanai, K. & Babazono, T. Comparative effects of sodium–glucose cotransporter 2 inhibitors versus dipeptidyl peptidase-4 inhibitors on kidney function decline in Japanese individuals with type 2 diabetes. Clin Exp Nephrol (2024). https://doi.org/10.1007/s10157-024-02499-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10157-024-02499-2