Abstract
Background
The literature is inconclusive when comparing health-related quality of life following restorative anterior resection (AR) compared with abdominoperineal resection (APR). Consideration of functional outcomes may explain this inconsistency. The aim of this study was to compare health-related quality of life in patients post-anterior resection, stratified by low anterior resection syndrome score, and post-abdominoperineal resection patients.
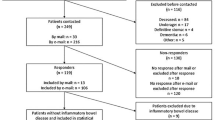
Methods
A cross-sectional study of consecutive patients post APR and AR for rectal or sigmoid adenocarcinoma at a tertiary centre in Sydney, Australia (Jan 2012- Dec 2021) was performed. HRQoL outcomes (SF36v2 physical [PCS] and mental component summary [MCS] scores) were compared between APR and AR patients, with subgroup analyses stratifying AR patients according to LARS score (no/minor/major). Age- and gender-adjusted comparisons were performed by linear regression.
Results
Overall, 248 post-AR patients (57.3% male, mean age 70.8 years, SD 11.6) and 64 post-APR patients (62.5% male, mean age 68.1 years, SD 13.1) participated. When stratified by LARS, ‘major LARS’ had a similar negative effect on age-and sex-adjusted PCS scores as APR. ‘No LARS’ (p < 0.001) and ‘minor LARS’ (p < 0.001) patients had higher PCS scores compared to post-APR patients. ‘Major LARS’ had a similarly negative effect on MCS scores compared with post-APR patients. MCS scores were higher in ‘no LARS’ (p = 0.006) compared with APR patients.
Conclusions
Postoperative bowel dysfunction significantly impacts health-related quality of life. Patients with ‘major LARS’ have health-related quality of life as poor as those following APR. This requires consideration when counselling patients on postoperative health-related quality of life, especially where poor postoperative bowel function is anticipated following restorative surgery.

Similar content being viewed by others
Data availability
De-identified data can be made available with a request of the corresponding author due to patient privacy concerns.
References
Ståhle E, Påhlman L, Enblad P (1986) Double stapling technique in the management of rectal tumours. Acta Chir Scand 152:743–747
Fernandes MC, Gollub MJ, Brown G (2022) The importance of MRI for rectal cancer evaluation. Surg Oncol 43:101739. https://doi.org/10.1016/j.suronc.2022.101739
Denlinger CS, Barsevick AM (2009) The challenges of colorectal cancer survivorship. J Natl Compr Canc Netw 7(8):883–893. https://doi.org/10.6004/jnccn.2009.0058
Croese AD, Lonie JM, Trollope AF, Vangaveti VN, Ho YH (2018) A meta-analysis of the prevalence of low anterior resection syndrome and systematic review of risk factors. Int J Surg 56:234–241. https://doi.org/10.1016/j.ijsu.2018.06.031
Bryant CL, Lunniss PJ, Knowles CH, Thaha MA, Chan CL (2012) Anterior resection syndrome. Lancet Oncol 13(9):e403–e408. https://doi.org/10.1016/s1470-2045(12)70236-x
Emmertsen KJ, Laurberg S (2012) Low anterior resection syndrome score: development and validation of a symptom-based scoring system for bowel dysfunction after low anterior resection for rectal cancer. Ann Surg 255(5):922–928. https://doi.org/10.1097/SLA.0b013e31824f1c21
Battersby NJ, Juul T, Christensen P et al (2016) Predicting the risk of bowel-related quality-of-life impairment after restorative resection for rectal cancer: a multicenter cross-sectional study. Dis Colon Rectum 59(4):270–280. https://doi.org/10.1097/dcr.0000000000000552
Al Rashid F, Liberman AS, Charlebois P et al (2022) The impact of bowel dysfunction on health-related quality of life after rectal cancer surgery: a systematic review. Tech Coloproctol 26(7):515–527. https://doi.org/10.1007/s10151-022-02594-0
Mols F, Lemmens V, Bosscha K, van den Broek W, Thong MS (2014) Living with the physical and mental consequences of an ostomy: a study among 1–10-year rectal cancer survivors from the population-based PROFILES registry. Psychooncology 23(9):998–1004. https://doi.org/10.1002/pon.3517
Cornish JA, Tilney HS, Heriot AG, Lavery IC, Fazio VW, Tekkis PP (2007) A meta-analysis of quality of life for abdominoperineal excision of rectum versus anterior resection for rectal cancer. Ann Surg Oncol 14(7):2056–2068. https://doi.org/10.1245/s10434-007-9402-z
Lawday S, Flamey N, Fowler GE et al (2021) Quality of life in restorative versus non-restorative resections for rectal cancer systematic review. BJS Open 5(6):zrab101. https://doi.org/10.1093/bjsopen/zrab101
Pachler J, Wille-Jørgensen P (2005) Quality of life after rectal resection for cancer with or without permanent colostomy. Cochrane Database Syst Rev 18(2):Cd004323. https://doi.org/10.1002/14651858.CD004323.pub3
Ng KS, Gladman MA (2020) Patient-reported and physician-recorded bowel dysfunction following colorectal resection and radical cystectomy: a prospective, comparative study. Colorectal Dis 22(10):1336–1347. https://doi.org/10.1111/codi.15041
Ware JE Jr, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30(6):473–483
Mrak K, Jagoditsch M, Eberl T, Klingler A, Tschmelitsch J (2011) Long-term quality of life in pouch patients compared with stoma patients following rectal cancer surgery. Colorectal Dis 13(12):e403–e410. https://doi.org/10.1111/j.1463-1318.2011.02740.x
Feddern ML, Emmertsen KJ, Laurberg S (2019) Quality of life with or without sphincter preservation for rectal cancer. Colorectal Dis 21(9):1051–1057. https://doi.org/10.1111/codi.14684
Honda M, Akiyoshi T, Noma H et al (2016) Patient-centered outcomes to decide treatment strategy for patients with low rectal cancer. J Surg Oncol 114(5):630–636. https://doi.org/10.1002/jso.24376
Koëter T, Bonhof CS, Schoormans D et al (2019) Long-term outcomes after surgery involving the pelvic floor in rectal cancer: physical activity, quality of life, and health status. J Gastrointest Surg 23(4):808–817. https://doi.org/10.1007/s11605-018-4014-4
Keane C, Fearnhead NS, Bordeianou LG et al (2020) International consensus definition of low anterior resection syndrome. ANZ J Surg 90(3):300–307. https://doi.org/10.1111/ans.15421
Juul T, Ahlberg M, Biondo S et al (2014) Low anterior resection syndrome and quality of life: an international multicenter study. Dis Colon Rectum 57(5):585–591. https://doi.org/10.1097/dcr.0000000000000116
Sun V, Grant M, McMullen CK et al (2014) From diagnosis through survivorship: health-care experiences of colorectal cancer survivors with ostomies. Support Care Cancer 22(6):1563–1570. https://doi.org/10.1007/s00520-014-2118-2
WOCN Society Clinical Guideline (2018) Management of the adult patient with a fecal or urinary ostomy-an executive summary. J Wound Ostomy Continence Nurs 45(1):50–58. https://doi.org/10.1097/won.0000000000000396
Danielsen AK, Burcharth J, Rosenberg J (2013) Patient education has a positive effect in patients with a stoma: a systematic review. Colorectal Dis 15(6):e276–e283. https://doi.org/10.1111/codi.12197
Christensen P, Im Baeten C, Espín-Basany E et al (2021) Management guidelines for low anterior resection syndrome - the MANUEL project. Colorectal Dis 23(2):461–475. https://doi.org/10.1111/codi.15517
van Heinsbergen M, den Haan N, Maaskant-Braat AJ et al (2020) Functional bowel complaints and quality of life after surgery for colon cancer: prevalence and predictive factors. Colorectal Dis 22(2):136–145. https://doi.org/10.1111/codi.14818
Acknowledgements
The authors thank the colorectal surgeons at Concord Hospital, Dr P Stewart, Dr M Suen, Dr H Cheung, Dr M Reece, Prof EL Bokey, A/Prof C Young and Dr A Gilmore who contributed patients to this study. And to Gael Sinclair who assisted with the management of the Concord Colorectal Cancer Database.
Funding
No external funding or grant support was obtained or received for the study. The authors declare that they have financial relationships to disclose.
Author information
Authors and Affiliations
Contributions
All authors have made substantial contributions to the paper and are in agreement of all aspects of the work. Details regarding author contributions are as below. SK: Study conception and design; Data acquisition; Data analysis and interpretation; Drafting the article; Critical revision for intellectual content; Final approval of the manuscript; Agreement to be accountable for all aspects of the work in ensuring that questions regarding accuracy & integrity are investigated & resolved. LB-S: Data acquisition; Drafting the article; Final approval of the manuscript; Agreement to be accountable for all aspects of the work in ensuring that questions regarding accuracy & integrity are investigated & resolved. MJFXR: Study conception and design; Critical revision for intellectual content; Final approval of the manuscript; Agreement to be accountable for all aspects of the work in ensuring that questions regarding accuracy & integrity are investigated & resolved. AK: Study conception and design; Critical revision for intellectual content; Final approval of the manuscript; Agreement to be accountable for all aspects of the work in ensuring that questions regarding accuracy & integrity are investigated & resolved. PHC: Study conception and design; Drafting the article; Critical revision for intellectual content; Final approval of the manuscript; Agreement to be accountable for all aspects of the work in ensuring that questions regarding accuracy & integrity are investigated & resolved. KSNg: Study conception and design; Data acquisition; Data analysis and interpretation; Drafting the article; Critical revision for intellectual content; Final approval of the manuscript; Agreement to be accountable for all aspects of the work in ensuring that questions regarding accuracy & integrity are investigated & resolved.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the Sydney Local Health District Human Research Ethics Committee of Concord Repatriation General Hospital (CGRH). This study was conducted with appropriate informed consent of study participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Koneru, S., Builth-Snoad, L., Rickard, M.J.F.X. et al. Major low anterior resection syndrome has equivalent health-related quality of life implications as having a permanent colostomy. Tech Coloproctol 28, 17 (2024). https://doi.org/10.1007/s10151-023-02879-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10151-023-02879-y